Translate this page into:
Plasma cell vulvitis: A vulvar itching dilemma
2 Faculty Dermatology Division, Maltepe University Medicine, Istanbul, Turkey
3 Faculty Pathology Division, Maltepe University Medicine, Istanbul, Turkey
Correspondence Address:
Aygen �elik
Maltepe University Medicine, Faculty Obstetrics and Gynecology Division, Istanbul
Turkey
| How to cite this article: �elik A, Haliloglu B, Tanri�ver Y, Ilter E, G�nd�z T, Ulu I, Midi A, �zekici �. Plasma cell vulvitis: A vulvar itching dilemma. Indian J Dermatol Venereol Leprol 2012;78:230 |
Sir,
Plasma cell vulvitis is an extremely rare skin disease that affects vulva during the lifetime of a woman. It can be seen especially during the climacterium and characterized by plasma cell infiltration. In the English literature nearly 46 cases were reported until now. The name derives from the plasma cells seen on biopsies of affected skin. The rarity of plasma cell vulvitis leads to both difficult diagnosis and treatment especially for gynecologists. It may even mimic intraepithelial neoplasia. In the presenting rare report we aim to draw attention to the importance of both consultation with a dermatologist and suspicion of plasma cell vulvitis at doubtful vulvar itching cases.
A 57-year-old woman was referred to our clinic with a 3-year history of recurrent vulvar pruritis, intermittent punctate hemorrhage and dyspareunia. She received medication for her recurrent itching symptoms a number of times, and also had a biopsy for her resistant recurrent vulvar pruritis that was reported as reactive changes in the squamous epithelium. Neither any other chronic diseases nor any trauma exist in her history. During her current physical examination smooth, well-defined, bright red erythematous macules with a diameter of 3 mm to 2 cm were observed on the vulva and vagina, and the lesions were fragile [Figure - 1]. We consulted the patient with a dermatologist and decided to perform another punch biopsy. Screening for sexually transmitted infections (including herpes, human papilloma viruses and syphilis) were negative. The skin biopsy revealed epithelial thinning, inflammatory cell infiltration predominantly plasma cells infiltration (more than 50%), tissue edema, vascular proliferation and dilatation. Plasma cells were predominantly located around the vessels and beneath the mucosa, and there were no premalignant changes [Figure - 2].
 |
| Figure 1: The vulva showing bright red erythematous macules |
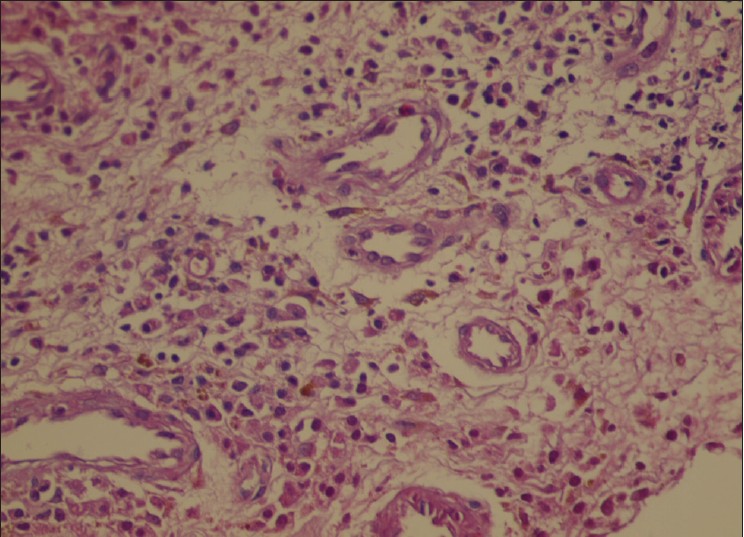 |
| Figure 2: Picture of histopathological examination; (H and E, ×400) |
Topical clobetasol 17-dipropionate cream 0.05%, twice daily was prescribed. Three weeks after starting the treatment with the topical steroids, 50% of her complaints had resolved and the lesions significantly improved. After 3 months, all the symptoms and signs were relieved [Figure - 3].
 |
| Figure 3: Lesions improved after 3 weeks of topical steroid |
Plasma cell vulvitis (or Zoon′s vulvitis) is a chronic and a very rare inflammatory disease. Lesions are usually seen on the vulvar mucosa in the form of well-defined, shiny, erythematous macules or papules that are sometimes eroded. Etiological factors are known as; viral, autoimmune, hormonal, and irritant (poor hygiene, sweating, trauma and persistent friction). The symptoms are generally pruritis, pain, burning, dyspareunia and bleeding. Differential diagnosis includes contact dermatitis, syphilis or herpes simplex infection, lichen planus, lichen sclerosus et atrophicus, pemphigus vulgaris, drug eruptions and squamous cell carcinoma. It is important to remember that plasma cell vulvitis does not undergo malignant change. Histological examination reveals infiltration of plasma cell in more than 50% of the dermis. Epidermal atrophy with elongated keratinocytes and vascular proliferation are the other findings. Patients with plasma cell vulvitis have been treated in a number of different ways. Topical steroid creams might be useful in some cases, local injections of interferon alpha into the lesion, [1] synthetic retinoid; etretinate [2] were shown to have benefits in a few patients. Antifungal and antibiotic preparations might be tried, tacrolimus oinment (topical calcineurin inhibitor) [3] might be an alternative treatment for plasma cell vulvitis cases that are resistant to conventional therapies. Imiquimod cream [4] might also be tried. Surgical excision, laser destruction [5] are the other choices for treatment. The response to the topical steroids in our patient was satisfactory. Plasma cell vulvitis should always be kept in mind in the patients with complaints of recurrent and resistant pruritis and dyspareunia.
| 1. |
Morioka S, Nakajima S, Yaguchi H, Naito K, Iwahara K, Ogawa H. Vulvitis circumscripta plasma cellularis treated successfully with interferon alpha. J Am Acad Dermatol 1988;19:947-50.
[Google Scholar]
|
| 2. |
Robinson JB, Im DD, Simmons-O'Brien E, Rosenshein NB. Etretinate: Therapy for plasma cell vulvitis. Obstet Gynecol 1998;92:706.
[Google Scholar]
|
| 3. |
Virgili A, Mantovani L, Lauriola MM, Marzola A, Corazza M. Tacrolimus 0,1% ointment: Is it really effective in plasma cell vulvitis? Report of four cases. Dermatology 2008;216:243-6.
[Google Scholar]
|
| 4. |
Frega A, Rech F, French D. Imiquimod treatment of vulvitis circumscripta plasmacellularis. Int J Gynaecol Obstet 2006;95:161-2.
[Google Scholar]
|
| 5. |
Retamar RA, Kien MC, Chouela EN. Zoon's balanitis: Presentation of 15 patients, five treated with a carbon dioxide laser. Int J Dermatol 2003;42:305-7.
[Google Scholar]
|
Fulltext Views
5,210
PDF downloads
4,523





