Translate this page into:
Polarized and ultraviolet dermoscopy for the diagnosis of dermatophytosis of vellus hair
Correspondence Address:
Yuping Ran
No. 37, Guo Xue Xiang, Chengdu, Sichuan 610041
China
| How to cite this article: Tang J, Ran Y. Polarized and ultraviolet dermoscopy for the diagnosis of dermatophytosis of vellus hair. Indian J Dermatol Venereol Leprol 2020;86:607 |
Sir,
Dermatophytosis of vellus hair is an uncommon condition. Diagnostic and therapeutic guidelines are lacking. However, dermoscopy has been shown to be a valuable tool in the diagnosis of several fungal dermatoses. Herein, we report a case of dermatophytosis of vellus hair in whom both polarized and ultraviolet (UV) light helped us determine vellus hair involvement.
A 4-year-old girl presented to the department of dermatovenereology with a history of pruritic rash on the right side of the face of 6 months duration. In spite of treatment with topical antifungal agents and topical steroids, the lesions persisted. The patient was otherwise healthy. A contact history with cats and dogs was elicited. Clinical examination revealed multiple erythematous papules and ill-defined plaques with fine scales on the right cheek and eyebrow [Figure - 1].
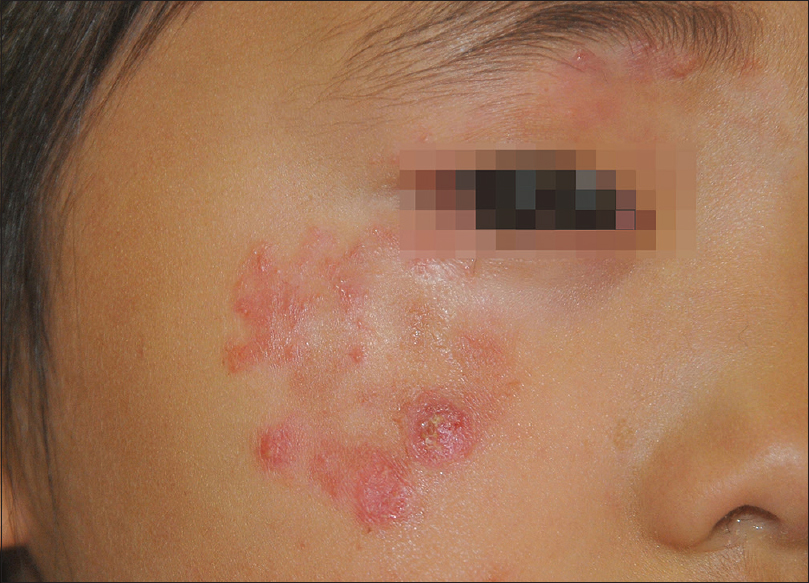 |
| Figure 1: Multiple erythematous papules and plaques with fine scales on the right cheek and eyebrow |
Polarized dermoscopy (Dino-Lite DermaScope; Dino-Lite, Naarden, Holland) of the lesions revealed non-homogeneous erythematous background with scattered linear vessels, follicular micropustules and yellowish scales [Figure - 2]. Vellus hair with white sheath around hair shaft [Figure - 2], arrowheads] was also noted. UV dermoscopy (dermoscopy with UV light, UV band 400 nm, SmartV 150DF; JEDA, Nanjing, China) elicited green fluorescence at the proximal hair shaft of the vellus hair [Figure - 3], arrowheads]. Direct microscopy of the abnormal vellus hair revealed ectothrix hyphae on the proximal hair shaft [Figure - 4]. Microsporum gypseum was identified by both fungal culture and ribosomal DNA sequence analysis (GenBank accessing number: MK418260).
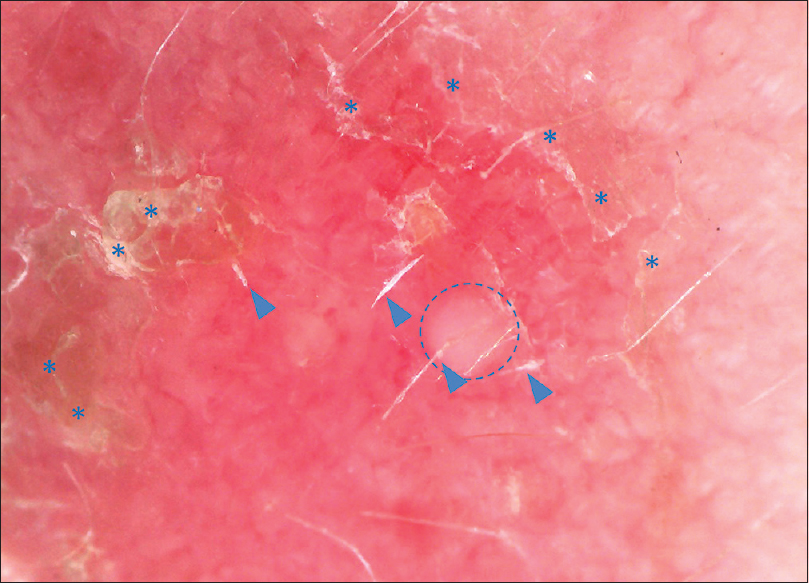 |
| Figure 2: Polarized dermoscopy showing yellowish scales (asterisks), follicular micropustules (circle) and vellus hair with white sheath around hair shaft (arrowheads) (×50) |
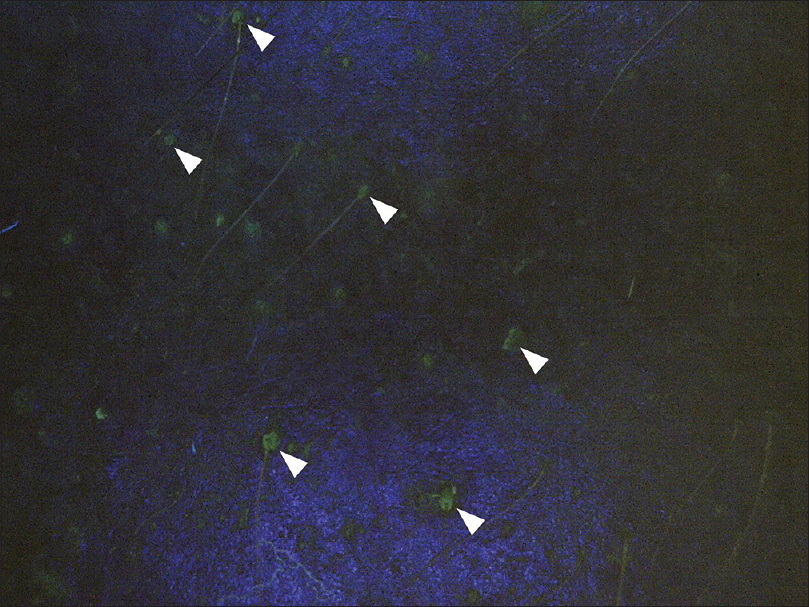 |
| Figure 3: UV dermoscopy showing green fluorescence at the proximal hair shaft of the vellus hair (arrowheads, ×50) |
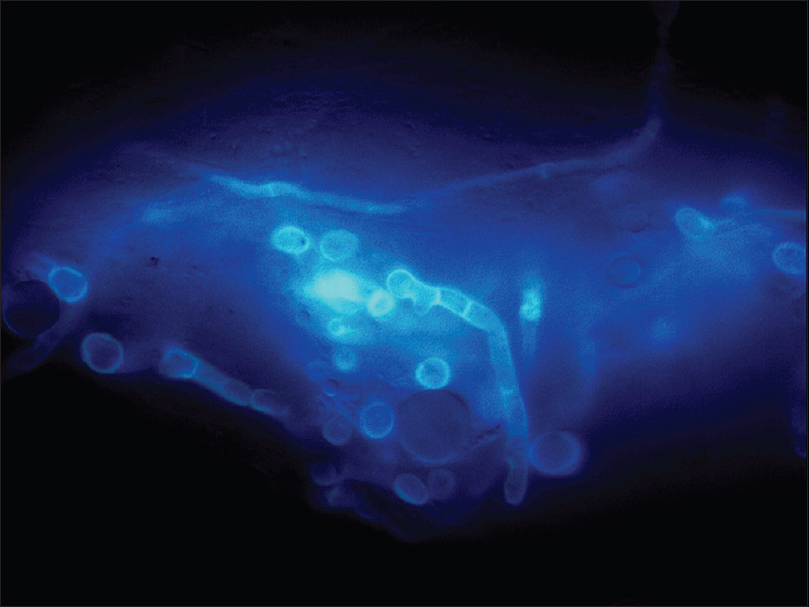 |
| Figure 4: Direct microscopy after calcofluor-white staining showing hyphae at the proximal hair shaft (×400) |
Based on these results, the patient was diagnosed with dermatophytosis of vellus hair. Oral itraconazole 100 mg/day, topical naftifine hydrochloride and ketoconazole cream were administered. Unfortunately, the patient was lost to follow-up.
Dermatophytosis of vellus hair is an entity which was initially proposed by Eby and Jetton in a 3-year-old boy with Nannizzia incurvata infection of vellus hair in 1971.[1] It mostly infects children by zoophilic or geophilic species due to increased chance of contact with soil or pets. Follicular micropustules and inflammatory or excoriated papules are the main clinical features.[2] Use of topical steroids is a predisposing factor and resistance to topical antifungal agents is common.[2]
The pathogenesis of dermatophytosis of vellus hair has not so far been elucidated. Inappropriate use of topical corticosteroids may cause local immunosuppression facilitating parasitism of the hair. Non-anthropophilic species cause more inflammatory response.
Dermatophytosis has a broad clinical spectrum that varies depending on the affected sites. Involvement of hair follicle is the common factor in dermatophytosis of vellus hair and tinea capitis. Tinea incognito, Majocchi granuloma and dermatophytosis of vellus hair share predisposing factor of previous use of steroids and clinical manifestation of pustules. Therefore, dermatophytosis of vellus hair is more akin to those refractory kinds of dermatophytosis than tinea faciei or tinea corporis. Based on the definition, dermatophytosis of vellus hair is easy to differentiate from tinea faciei, for the latter lacks vellus hair involvement and related appearance clinically and dermoscopically, such as follicular micropustules and abnormal vellus hair. Classically, systemic antifungal treatment is usually mandatory in dermatophytosis affecting cutaneous appendages like hair and nail. Topical therapy may be insufficient as penetration of antifungals is limited and hence dermatophytosis of vellus hair is an indication for systemic antifungal therapy.[1],[3]
Diagnosis of dermatophytosis of vellus hair is important because it has prognostic and therapeutic implications. Microscopic and mycological studies are the gold standard for diagnosis of dermatophytosis. However, dermatophytosis of vellus hair may represent various dermoscopic findings, which are useful for the diagnosis. Dermoscopy often reveals an erythematous background without any specific vascular pattern.[4],[5] Follicular pustules, empty follicles and black dots may be noted,[3],[4] which may suggest fungal invasion of hair follicle. Importantly, the involved hair may have a different appearance, such as translucent hair, broken hair, corkscrew hairs, dystrophic hair and morse code–like hair.[3],[5]
Dermoscopy is also helpful for assisting sampling for fungal examination in our clinical practice based on its amplification effect. When fungal infection is suspected under dermoscope, we may take samples for direct microscopy from specific sites like vellus hair with white sheath as in this case.
It is also worth mentioning that UV dermoscopy, acting as a miniature and portable Wood's lamp device, is a new noninvasive and efficient auxiliary diagnostic tool.[6] The chemical responsible for positive fluorescence when exposed to UV light is pteridine, which can be produced by some kinds of fungi like Microsporum species.[7] Therefore, UV light helps in identification of species of dermatophytes showing fluoresence, like Microsporum species, especially when the fluoresence corresponds to the infected hair observed by the polarized dermoscope. We have observed it to be useful in patients with tinea capitis and now for dermatophytosis of vellus hair.[5] However, accuracy and specificity remain to be studied in larger case series.
Dermatophytosis of vellus hair has distinct clinical manifestations, dermoscopic features and therapeutic implications. It is possibly an underdiagnosed entity. Awareness regarding this condition is necessary among the clinicians for early and appropriate diagnosis and treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given his consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Eby CS, Jetton RL. Nannizzia incurvata infection of vellus hair. Br J Dermatol 1971;85:582-4.
[Google Scholar]
|
| 2. |
Gómez-Moyano E, Crespo-Erchiga V. Tinea of vellus hair: An indication for systemic antifungal therapy. Br J Dermatol 2010;163:603-6.
[Google Scholar]
|
| 3. |
Gómez-Moyano E, Crespo Erchiga V, Martínez Pilar L, Martínez García S, Martín González T, Godoy Diaz DJ, et al. Using dermoscopy to detect tinea of vellus hair. Br J Dermatol 2016;174:636-8.
[Google Scholar]
|
| 4. |
Knöpfel N, del Pozo LJ, Escudero Mdel M, Martín-Santiago A. Dermoscopic visualization of vellus hair involvement in tinea corporis: A criterion for systemic antifungal therapy? Pediatr Dermatol 2015;32:e226-7.
[Google Scholar]
|
| 5. |
Xu X, You Z, Dai Y, Singh N, Zhang C, Ran Y. Dermoscopic, fluorescence staining and scanning electronic microscopic observation on facial tinea of vellus hair in a child. Chin J Dermatovenerol 2018;3:299-301.
[Google Scholar]
|
| 6. |
Tang J, Ran X, Ran Y. Ultraviolet dermoscopy for the diagnosis of tinea capitis. J Am Acad Dermatol 2017;76:S28-30.
[Google Scholar]
|
| 7. |
Wolf FT. Chemical nature of the fluorescent pigment produced in Microsporum-infected hair. Nature 1957;180:860-1.
[Google Scholar]
|
Fulltext Views
4,882
PDF downloads
2,065





