Translate this page into:
Porphyrias amongst patients with cutaneous photosensitivity in Kashmir: A seven year experience
2 Department of Dermatology, STD and Leprosy, Govt Medical College Srinagar, Jammu and Kashmir, India
Correspondence Address:
Sabhiya Majid
Associate Professor and Head, Department of Biochemistry, Govt Medical College Srinagar, Jammu and Kashmir
India
| How to cite this article: Majid S, Ahmad QM, Shah IH. Porphyrias amongst patients with cutaneous photosensitivity in Kashmir: A seven year experience. Indian J Dermatol Venereol Leprol 2012;78:520 |
Sir,
Porphyrias are rare, exact prevalence differs, and need to be excluded in patients with typical medical, psychiatric, and surgical history. Cutaneous porphyrias present with skin lesions, photosensitivity, and anemia. Coordination between Deptt. of Dermatology and specialized porphyria testing laboratory in Department of Biochemistry made possible diagnosis, treatment of porphyrias and this pioneering major referral hospital-based 7-year study, from August 2003 to August 2010, to analyze percentage of porphyrias amongst patients with cutaneous photosensitivity from Kashmiri population. No such prior study had been done. Patients with cutaneous photosensitivity, attending OPD and IPD of hospitals associated with Govt. Medical College Srinagar, underwent routine physical examination, relevant biochemical and hematological tests. After confirming normal ANA and ds-DNA levels, 601 symptomatic patients negative for hepatitis and HIV were referred for porphyria testing as part of differential diagnosis comprised study sample. Mathematical and statistical analysis included calculation and comparison of percentage of types of porphyrias diagnosed. As a specialized porphyria testing center of Kashmir, we estimated our data covers 85-95% of all diagnosed cases in Kashmir. Our aim was effective management of cutaneous photosensitivity by improving awareness of porphyrias, seemingly very rare disorder, amongst medical professionals.
For diagnosing porphyrias analysis of clinical picture and biochemical -′porphyria profile′ comprising of analysis of porphyrins in urine, stool, blood and porphyrin precursors in urine was done. Porphyria typing is essential for management. Spectrophotometric quantification of porphyrin type increased and not exact isomer was considered serving as prototype for porphyria diagnosis /typing in developing countries. Here, sophisticated technique, high performance liquid chromatography needed for isomer identification is alternated. [1],[2],[3] Exemplarily, based on clinical picture and porphyrin data analysis, CEP was diagnosed by ruling out regime in 16-year-old male [[Figure - 1], clinical image] presenting with features of cutaneous photosensitivity, hyper pigmentation, hypertrichosis, pinched nose, sclerodermoid changes, erythrodontia, oncholysis of terminal phalanges, pallor, history of red-colored urine since childhood and splenomegaly. Investigations revealed hemolytic anemia with negative comb′s test, normal ANA, ds DNA. Normal delta amino levulinate and porphobilinogen levels excluded acute porphyrias, increased urine, stool, and erythrocyte porphyrins were suggestive of Congenital Erythropoietic Porphyria (CEP) or Hepato Erythropoietic Porphyria (HEP) - other types were excluded. Quantitative studies revealed urinary porphyrin levels >50 times normal with uroporphyrins more than coproporphyrins, elevated fecal porphyrins with coproporphyrins more than uroporphyrins. Erythrocytes showed greatly increased coproporphyrins, small amounts of uroporphyrins, protoporphyrins levels near normal. [4] Similarly, Erythropoietic protoporphyria (EPP) was diagnosed in 1-year-old baby girl [[Figure - 2], clinical image].
 |
| Figure 1: Clinical image: 17-year-old male with features of congenital erythropoietic porphyria |
 |
| Figure 2: Clinical image: 1-year-old baby with features of erythropoietic protoporphyria |
Overall, from study sample, 30 patients were diagnosed as porphyrias. 16 were erythropoietic type, 10 CEP, and 6 EPP. 14 were hepatic type, 2 Variegate Porphyria (VP), and 12 Porphyria Cutanea Tarda (PCT). A specific percentage pattern of porphyrias was observed in patients with cutaneous photosensitivity. Overall 5% were porphyrias, 2.66% erythropoietic type, and 2.34% were hepatic type. Comprising of 1.67% CEP, 0.99% EPP, 1.99% PCT, and 0.34% were VP [Figure - 3]. Thus, 54% porphyrias were of erythropoietic type, and 46% were of hepatic type. Further, amongst erythropoietic porphyrias, 64.2% had CEP, only 33.7% had EPP. Amongst hepatic porphyrias, 91.4% had PCT, only 8.5% had VP.
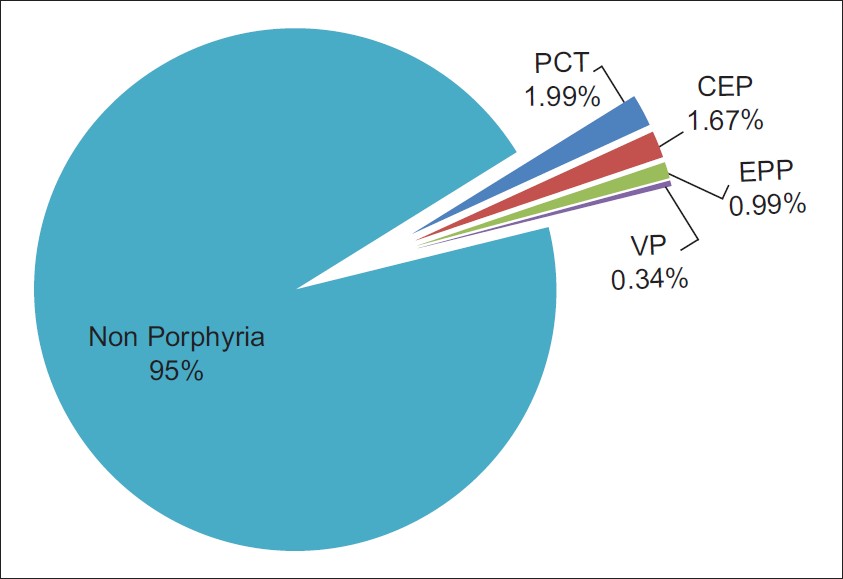 |
| Figure 3: Percentage of various types of porphyrias in patients with cutaneous photosensitivity |
Reported prevalence of porphyrias varies, from 1 in 500 to 1 in 50,000 people worldwide. Definitely genetic predisposition dependent on race and geographical locale has been observed and implicated. [4] PCT, documented as the commonest cause of ′cutaneous porphyrias′ worldwide, has greatest prevalence in Bantus tribe of S. Africa. Similarly, high incidence of 3 per 1000 people in South African white population for VP, 2 per million in Denmark for HCP, and 5-10 per 10,000 people for acute intermittent porphyria in Lapland, Scandinavia, and UK has been observed. [5],[6]
Reportedly, regarding CEP, till now no clear racial or sex predominance has been observed. Genetic predisposition to CEP in Kashmiri population dependent on race and geographical locale is implied based on striking observation in this pioneering study wherein percentage of CEP was comparable to PCT, commonest cutaneous porphyria worldwide and more than EPP documented most prevalent erythropoietic porphyria. Interestingly, although regarded as rare disease, considerable number of affected patients lives in Kashmir. Detailed population-based studies over longer period are further needed to account for this striking observation.
Diagnosis and management of porphyrias require multi-disciplinary collaborations among family practitioners, dermatologists, and porphyria specialists. Development of specialized porphyria centers to provide information, services, support to patients, clinicians and to conduct clinical trials/research on the many unknown aspects of porphyrias is need of the hour.
Acknowledgements
Ethical Committee Clearance: The project was cleared by the Departmental Ethical Committee.
| 1. |
Poh Fitzpatrick MB. Laboratory testing in porphyrias. Int J Dermatol 1979;18:453-60.
[Google Scholar]
|
| 2. |
Elder GH, Smith SG, Smyth SJ. Laboratory investigations of the porphyrias. Ann Clin Biochem 1990;27:395-412.
[Google Scholar]
|
| 3. |
Majid S, Massod Q, Hassan I, Veshnavi S, Hussain ST. Feasibility of diagnosis and typing Porphyrias in developing countries like India-its biochemical basis. J K Practitioner 2006;13:30-3.
[Google Scholar]
|
| 4. |
Majid S, Massod Q, Hassan I, Syed N, Sameen F, Rasool M. Puberty onset congenital erythropoietic porphyria - A case report. Timok Med J 2006;31:176-9.
[Google Scholar]
|
| 5. |
Kappas A, Sassa S, Galbriath RA, Nordmann Y. The porphyrias. In: Scriver C, Beaudett AL, Sly WS, Valle D, editors. The metabolic and molecular basis of inherited disease. 7th ed. USA: McGraw Hill;1995. p. 2103-39.
[Google Scholar]
|
| 6. |
Kauppinen R. Porphyrias. Lancet 2005;365:37-8.
[Google Scholar]
|
Fulltext Views
2,732
PDF downloads
2,131





