Translate this page into:
Post COVID-19 cutaneous infection caused by Scedoporium apiospermum in a patient with epidermolysis bullosa acquisita
Corresponding author: Dr. Abin Varghese, Department of Dermatology, Government Medical College, Thiruvananthapuram, India. abin054@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Varghese A, Jayapalan S, George AE, Chandran R. Post COVID-19 cutaneous infection caused by Scedoporium apiospermum in a patient with epidermolysis bullosa acquisita. Indian J Dermatol Venereol Leprol. 2024;90:266. doi: 10.25259/IJDVL_830_2022
Dear Editor,
Scedosporium apiospermum is a saprophytic filamentous fungus found in soil, manure and polluted water, causing localised infections of the skin, bones and eyes, following penetrating trauma. In immunocompetent individuals, it causes mycetoma. Disseminated infection occurs in immunocompromised persons.1 Widespread use of corticosteroids, immunosuppressants and anti-neoplastic agents has contributed to the increasing number of cases in recent years.2 Immune dysregulation caused by the COVID-19 illness predisposes the patients to invasive fungal infections.3 Here, we report a case of cutaneous S. apiospermum post-COVID-19 infection in a patient on immunosuppressant therapy for epidermolysis bullosa acquisita (EBA).
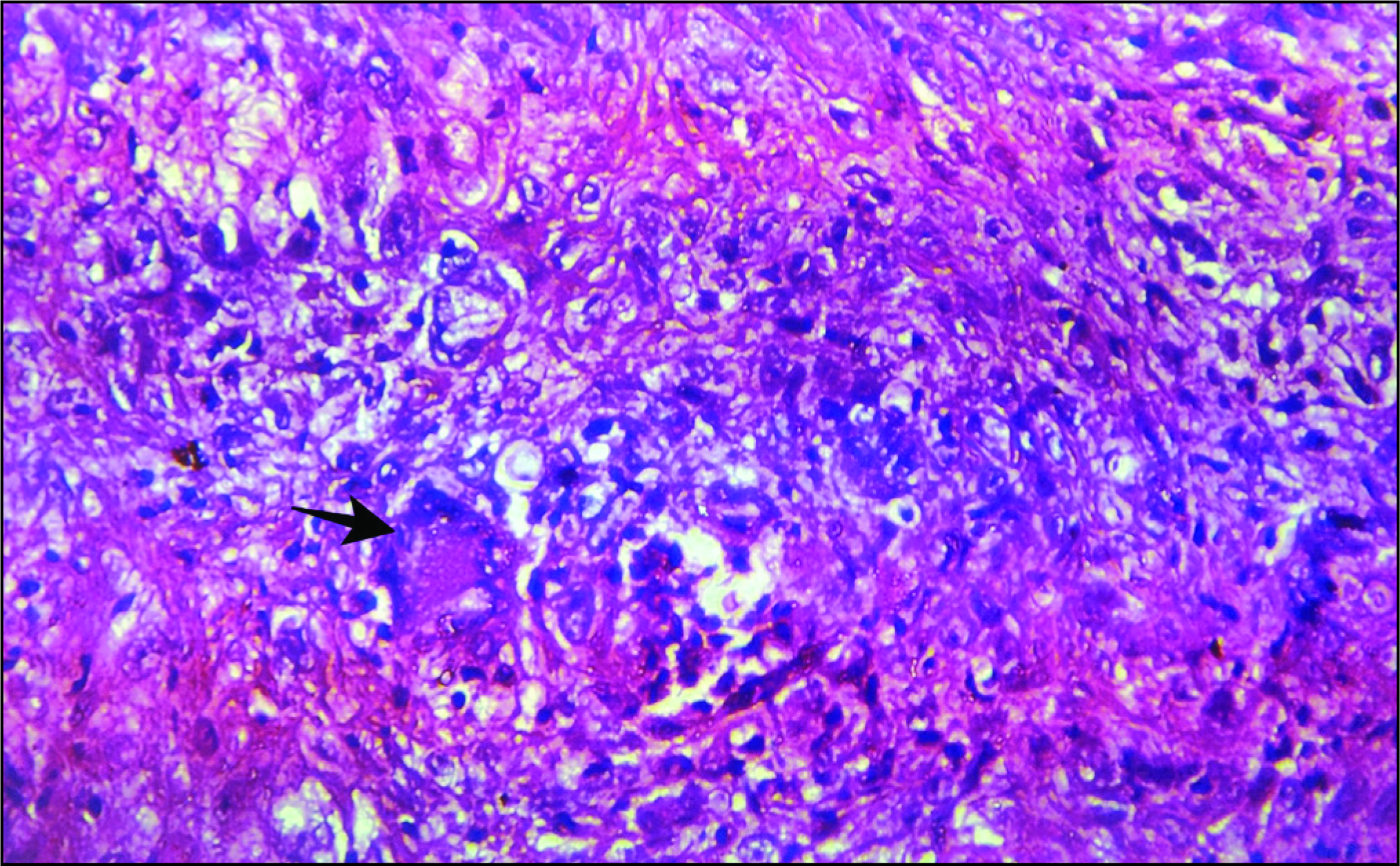
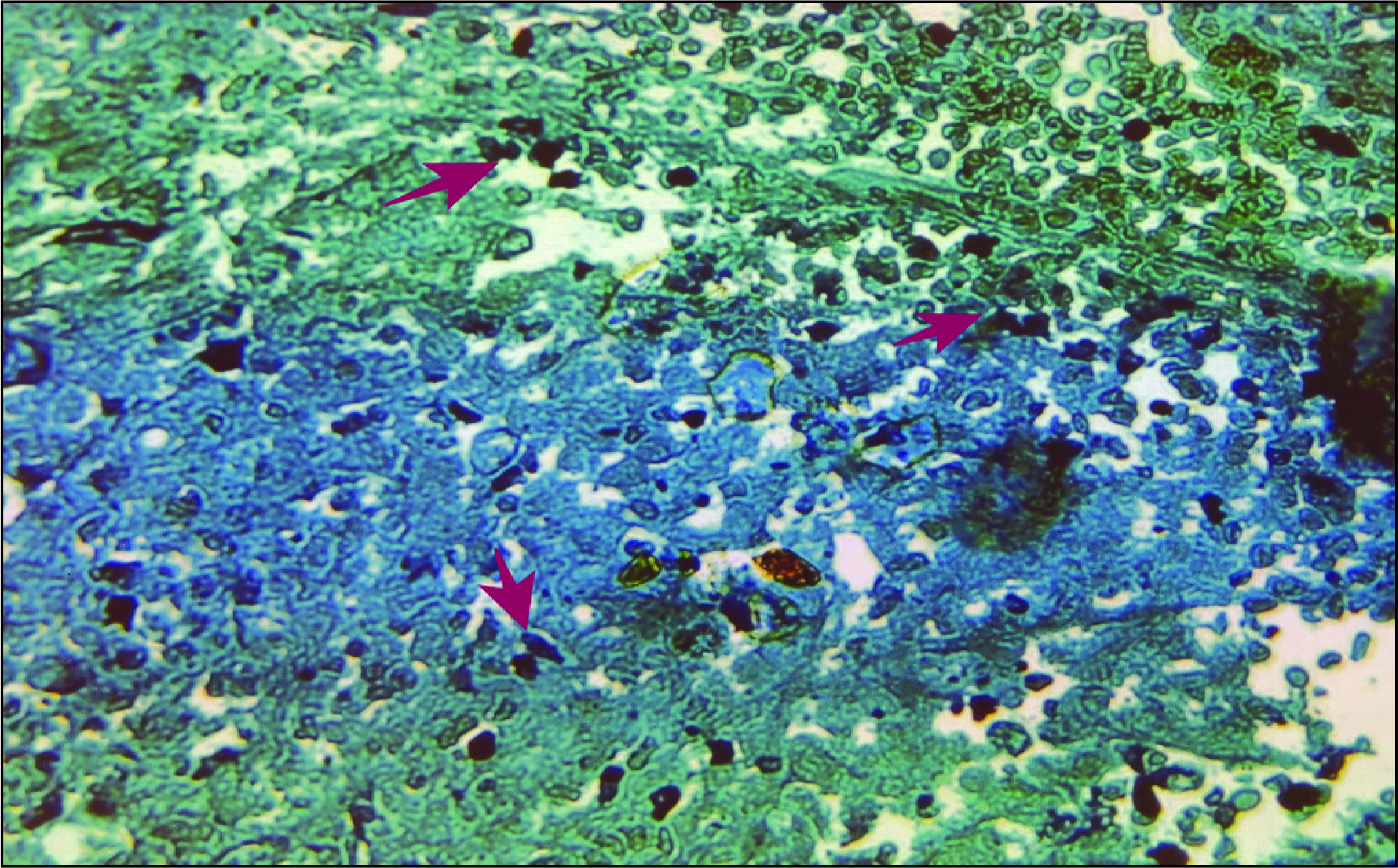
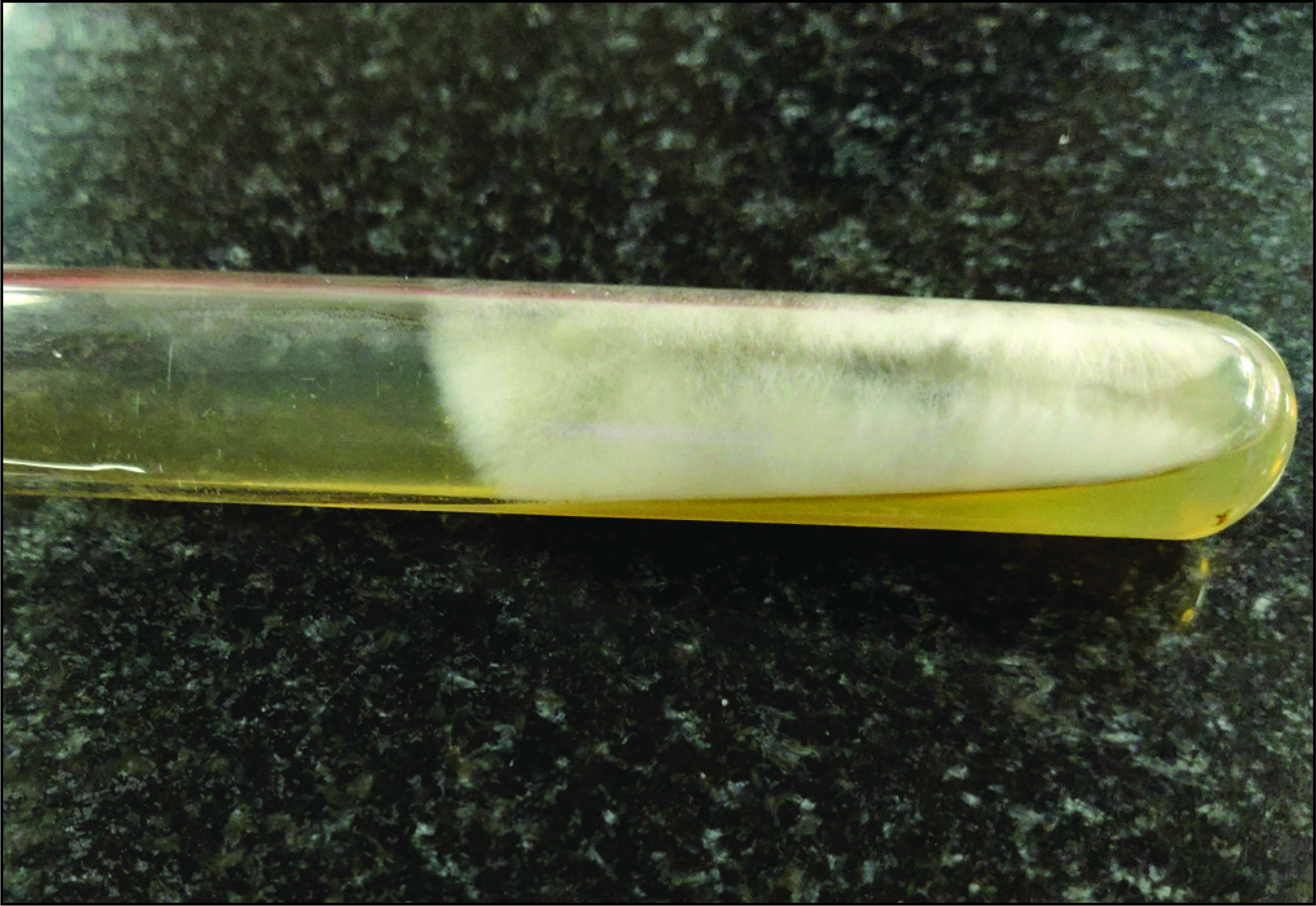
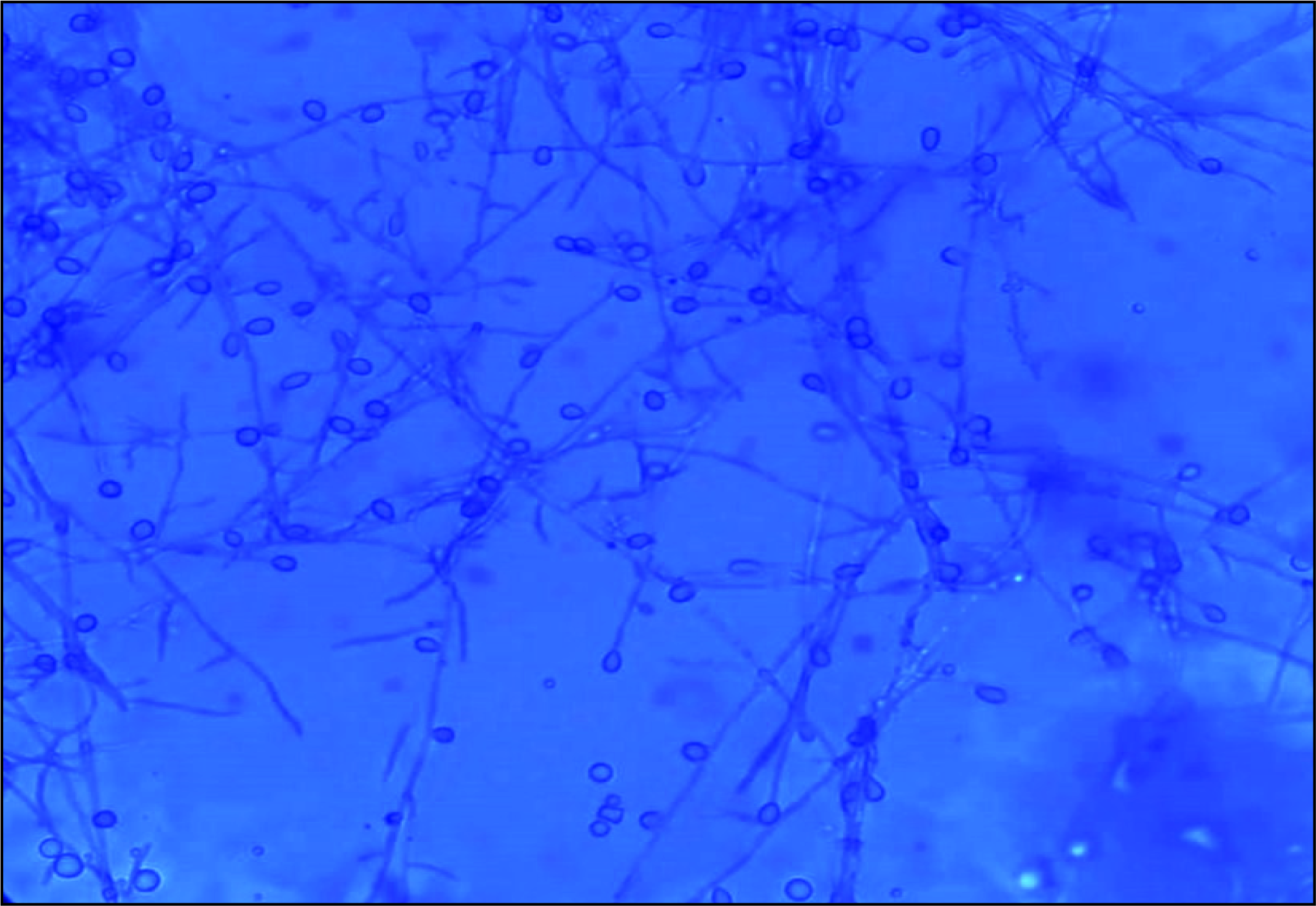
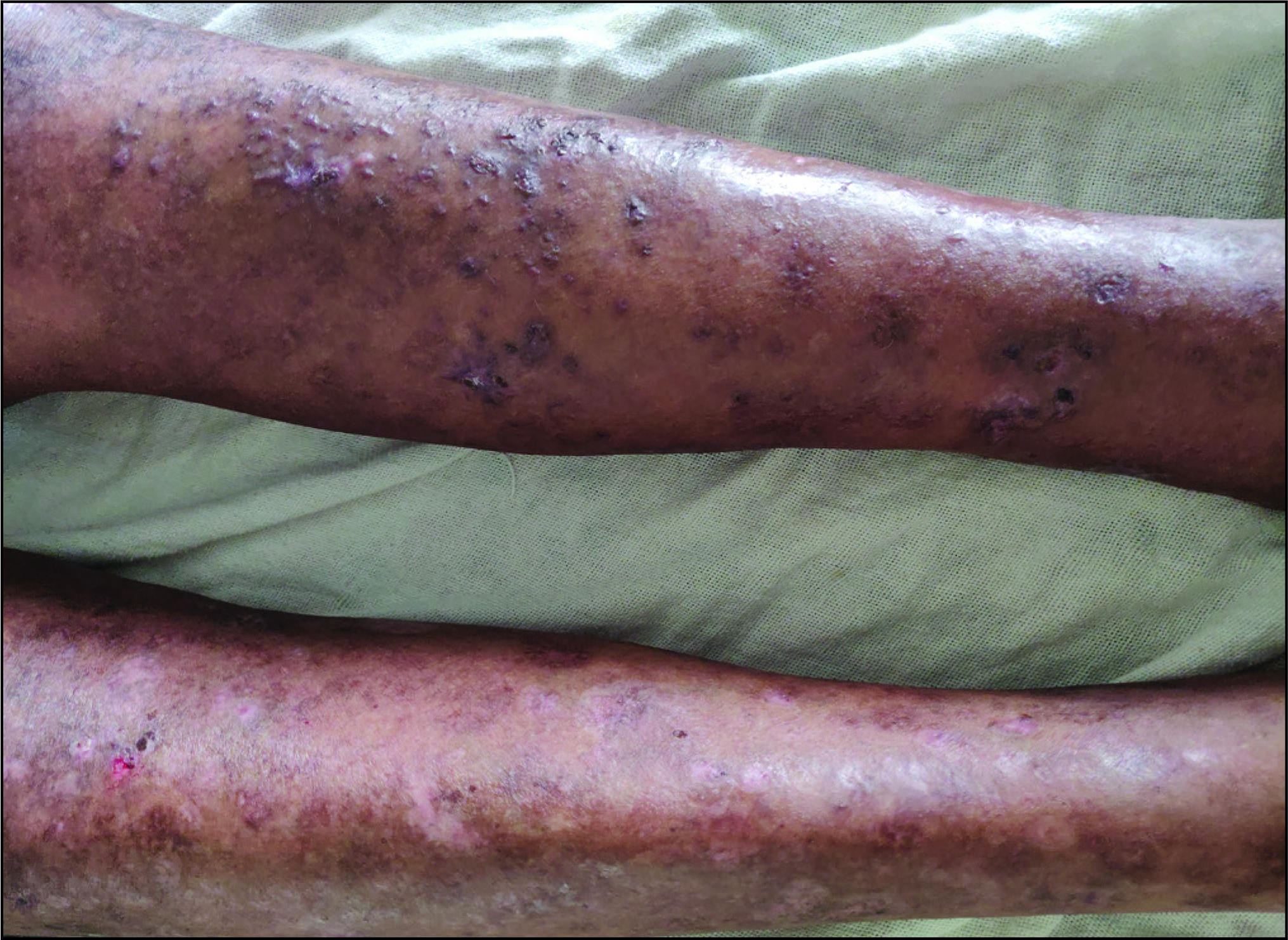
A 50-year-old man, with a two-month prior history of COVID-19 infection, presented with an exacerbation of his already existing bullous disease of four months duration. The diagnosis of EBA was confirmed by direct and indirect immunofluorescence, and he was treated with oral prednisolone (1 mg/kg body weight) and azathioprine (2 mg/kg body weight). Due to an inadequate response, treatment was changed to monthly dexamethasone-cyclophosphamide pulse (DCP) therapy. After a period of initial improvement, there were new erythematous papules, pustules, small punched-out ulcers, painless subcutaneous nodules in a linear pattern and pus discharging sinuses on the leg and medial aspect of the left thigh with underlying oedema [Figure 1]. Patient was investigated with clinical suspicion of subcutaneous fungal infection, botryomycosis and atypical mycobacterial infection. His baseline laboratory investigation showed anaemia (9.7g/dL), hyperglycaemia (303mg/dL) and hypoproteinemia (4.6g/dL). Ten percent potassium hydroxide mount and Gram stain from the pus revealed fungal elements. Histopathological examination showed granulomatous infiltrates composed of epithelioid cells, giant cells and lymphocytes in hematoxylin-eosin staining [Figure 2a]. Periodic acid-Schiff and Grocott methenamine silver staining revealed septate hyphae [Figure 2b]. Ultrasonography of the medial aspect of the left thigh and upper leg showed multiple reactive lymph nodes (>27 in number) and a few showing early suppuration. A fungal culture of pus obtained by ultrasound-guided fine needle aspiration from a lymph node in the left thigh on Sabouraud dextrose agar showed cottony fluffy white mould suggestive of Scedosporium [Figure 3]. Microscopy with lactophenol cotton blue stain showed septate hyphae with clavate-shaped conidia [Figure 4] characteristic of Scedosporium. Matrix-assisted laser desorption ionisation-time of flight (MALDI-TOF) mass spectrometry identified the fungal species as S. apiospermum. Lymphocutaneous type of scedosporiosis was diagnosed due to the direct involvement of numerous lymph nodes.4 He was treated with terbinafine 250 mg once daily and voriconazole 200 mg twice daily. A favourable response was observed after four months of therapy [Figure 5].

- Punched out ulcers and pus discharging sinuses on the left leg.
-
Cellular infiltrate with giant cell (indicated by arrow), epithelioid cells and lymphocytes (H &E, 400x).
-
Fungal hyphae (Grocott’s methenamine silver (GMS), 400x).
-
Culture on Sabouraud dextrose agar showing cottony fluffy white colonies suggestive of Scedosporium.
-
Microscopy with lactophenol cotton blue stain showing septate hyphae with clavate-shaped conidia.
-
Treatment response after 4 months of therapy.
Scedosporium infection in humans is mainly caused by Scedosporium apiospermum and S. boydii.5 The infection originates from the inoculation of fungal elements into minor injuries, and therefore the extremities are commonly involved.1,6 Though it is a known cause of mycetoma, in recent years it has been identified as an opportunistic pathogen, causing non-mycetoma skin diseases such as subcutaneous abscesses, ulcers, folliculitis-like nodes and lymphocutaneous-type sporotrichosis-like nodes in immunosuppressed individuals.1,4,6
On culture, Scedosporium spp has a white cottony appearance that later turns grey or brown. The hyphae are septate with simple, long or short conidiophores bearing oval or clavate conidia singularly or in small groups.
The literature review showed that almost all cases of cutaneous Scedosporium infection were seen in immunocompromised individuals.2,6 Immune dysregulation in COVID-19 infection occurs via various mechanisms like cytokine storm, hyperinflammatory response and coagulopathy.3 Higher pro-inflammatory (IL-1, IL-2, IL-6, tumour necrosis factor-a) cytokine levels and lower CD4, and interferon-gamma expression predispose to invasive fungal infection.7 DCP pulse therapy has been in vogue in our centre for the last 30 years and we have never seen a case of subcutaneous fungal infection among our treated patients. The post-COVID-19 infection under the backdrop of high-dose corticosteroid therapy might have compromised the immune response of this patient, making him a susceptible candidate for the opportunistic fungal infection.
The inherent resistance of Scedosporium spp. to amphotericin B and azoles limits the treatment options. Voriconazole is the preferred drug.8 Since the addition of terbinafine along with voriconazole has shown a synergistic effect5, we tried this combination in our patient with good response.
S. apiospermum is an emerging opportunistic pathogen that can be life-threatening. Inherent resistance to antifungals makes it difficult to treat. It is important to be aware of the wide array of clinical presentations of Scedosporiosis to avoid delay in diagnosis and prompt treatment.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Skin infection caused by Scedosporium apiospermum. Mycoses. 2003;46:524-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous Scedosporium apiospermum infection in an immunocompromised patient and a review of the literature. Acta Derm Venereol. 2005;85:156-9.
- [CrossRef] [PubMed] [Google Scholar]
- Post COVID-19 acute invasive fungal rhinosinusitis caused by Scedosporium apiospermum: a cover pathogen. Int J Otorhinolaryngol Head Neck Surg. 2021;7:1187-92.
- [Google Scholar]
- Scedosporium apiospermum infection imitating lymphocutaneous sporotrichosis in a patient with myeloblastic-monocytic leukaemia. Br J Dermatol. 1995;133:805-9.
- [CrossRef] [PubMed] [Google Scholar]
- Scedosporium apiospermum fungemia successfully treated with voriconazole and terbinafine. IDCases. 2020;22:e00928.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Case of cutaneous Scedosporium apiospermum infection successfully treated with voriconazole. J Dermatol. 2009;36:98-102.
- [CrossRef] [PubMed] [Google Scholar]
- Post Covid-19 Infection Presenting as Rhino-Orbital Mycosis. Indian J Otolaryngol Head Neck Surg. 2022;74 Suppl 2:3050-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Susceptibility of Pseudallescheria boydii and Scedosporium apiospermum to New Antifungal Agents. Jpn J Med Mycol. 2004;45:101-4.
- [CrossRef] [PubMed] [Google Scholar]





