Translate this page into:
Post kala-azar dermal leishmaniasis with mucosal and multisite upper airway involvement: Diagnostic challenge and management strategy
Corresponding author: Dr. Neetu Bhari, Department of Dermatology, AIIMS, New Delhi, India. drntbhari@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar R, Monga R, Radhani P, Ramesh V, Singh R, Ramam M, et al. Post kala-azar dermal leishmaniasis with mucosal and multisite upper airway involvement: Diagnostic challenge and management strategy. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_686_2023
Dear Editor,
A 59-year-old man from Bihar (India) presented with a palatal lesion and hoarseness of voice for 6–7 months. He also provided a history of nodular skin lesions involving his lower lip and forehead, gradually progressing in size for the last 3 years. There was no history of prolonged fever or weight loss. On examination, two well-defined erythematous firm nodules sized 1 × 1 cm were noted on the lower lip and forehead [Figure 1a]. Lesions were smooth and round to oval shaped. There were ill-defined erythematous papular lesions on the chin. Oral cavity examination revealed an erythematous infiltrated plaque involving soft and hard palate, along with few surface erosions [Figure 1b]. Fibre-optic endoscopic evaluation revealed a mucosa covered mass in the nasopharynx and a similar lesion at the anterior commissure extending into the sub-glottis while the remaining surrounding mucosa was grossly normal [Figures 1c and 1d]. Systemic examination did not reveal generalised lymphadenopathy or hepatosplenomegaly. A provisional differential diagnosis of mucosal carcinoma including adenoid cystic and mucoepidermoid was made. Blood counts and serum biochemistry were normal and viral markers (HBsAg, HIV 1&2, anti-HBc and anti-HCV antibodies) were negative. Biopsy from the forehead nodule showed epidermal atrophy, follicular plugging and dense dermal infiltrate composed of foamy histiocytes, histiocytes, lymphocytes and plasma cells [Figures 2a and 2b]. Similar infiltrate and epidermal atrophy were also noted in the mucosal plaque biopsy. No evidence of dysplasia was seen in these biopsies. Based on the histopathology a diagnosis of PKDL was considered. Although amastigote forms of Leishmania donovani were not seen in the biopsies, serum rK-39 antigen was positive. DNA isolated from skin scrapings showed positive amplification for Leishmania donovani when subjected to ITS-1 polymerase chain reaction (PCR) [Figure 2c]. This was further confirmed by sequence analysis of the polymerase chain reaction product.

- Well-defined firm nodules on the lower lip and forehead.

- Hypertrophy of the soft and hard palates and nodule on the lower lip.
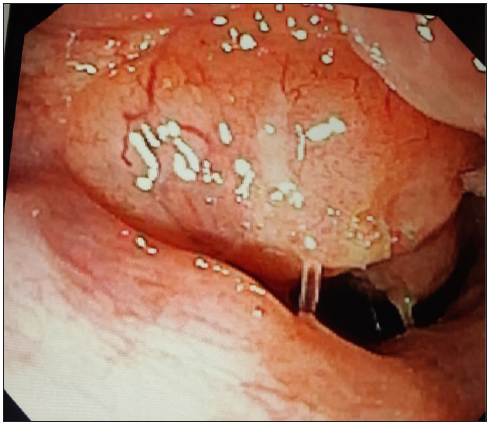
- Zero-degree endoscopy (straight angled scope for nose and nasopharynx) showing a mass occupying almost the whole of the nasopharynx.
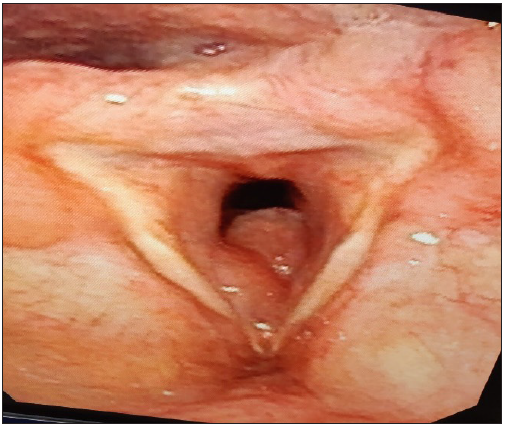
- Fibreoptic laryngoscopy showing lesion extending from the anterior commissure to subglottis, obscuring more than 50% of the subglottis.
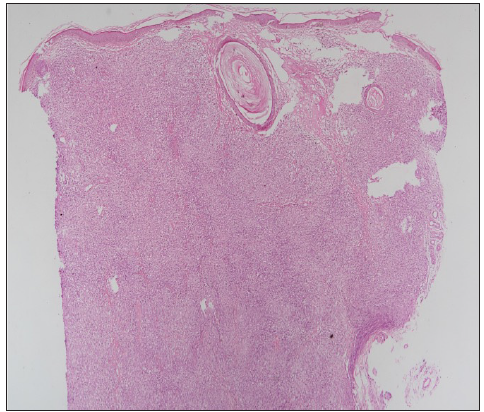
- Biopsy from nodule on the forehead and hard palate, respectively, showing dense pan-dermal infiltrate composed of foamy histiocytes, histiocytes, lymphocytes and plasma cells (Haematoxylin & Eosin, 100x).
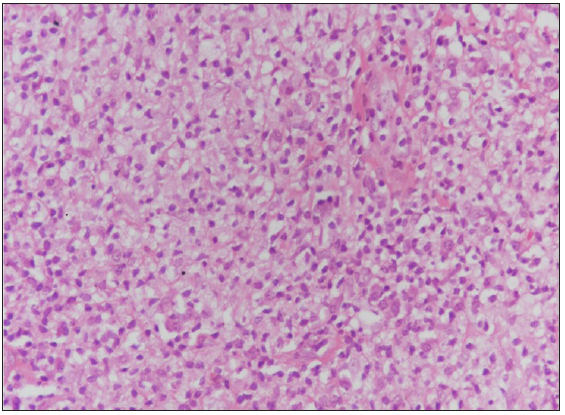
- Biopsy from the nodule on the forehead and hard palate, respectively, showing dense pan-dermal infiltrate composed of foamy histiocytes, histiocytes, lymphocytes and plasma cells (Haematoxylin & Eosin, 400x).
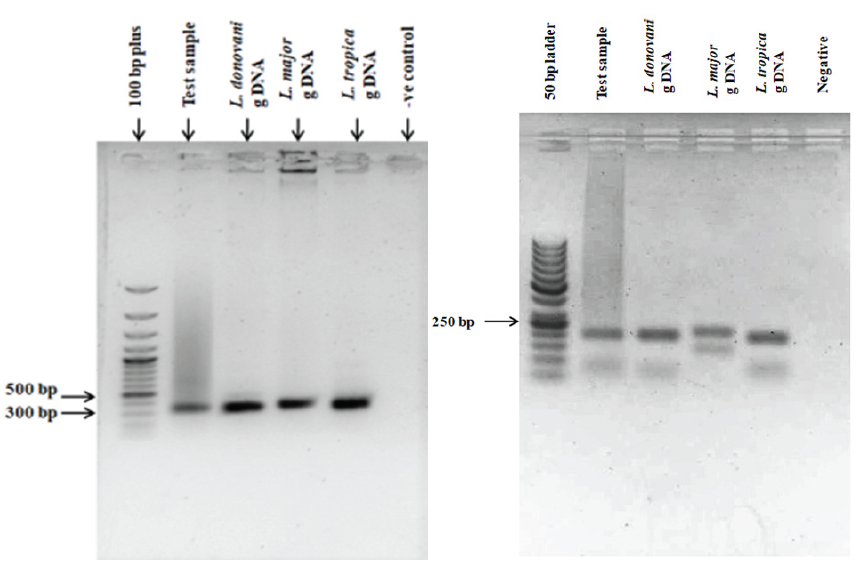
- Polymerase chain reaction test positive for L. donovani.
A final diagnosis of post-kala-azar dermal leishmaniasis with multisite mucosal (palate, nasopharynx and larynx) involvement was made and the patient was treated with oral miltefosine 50 mg twice daily. After 1 month of treatment, the skin and palatal lesions started improving. Treatment was stopped after 3 months when a complete clinical cure in the form of resolved cutaneous and palatal lesions was observed along with improvement in his voice quality [Figures 3a–3d]. No adverse effects were reported during and after the therapy. The patient has been advised 3 monthly regular follow-ups to detect any relapse.

- Follow-up at 45 days showing (a) decrease in the size of nodule over lower lip and forehead, (b) decrease in hypertrophy of soft and hard palates and (c) complete resolution of pharyngeal (d) as well as laryngeal lesions.
Post-kala-azar dermal leishmaniasis is a dermatologic manifestation seen in patients with a previous history of visceral leishmaniasis (VL) or kala-azar caused by Leishmania donovani. Incidence of post-kala-azar dermal leishmaniasis after visceral leishmaniasis varies from 5% to 10% in the Indian Subcontinent while it is about 60% in Sudan.1 Cutaneous manifestations of post-kala-azar dermal leishmaniasis include hypopigmented macules and papulo-nodular lesions on the face, arms and chest in patients who are otherwise asymptomatic. Mucosal involvement in post-kala-azar dermal leishmaniasis is rare but has been reported relatively frequently in the recent past 2–3 and usually involves lips, tongue, pharynx and conjunctiva. These lesions may present as nodules or hypertrophy at the commissural area, the dorsum of the tongue, the buccal mucosa or the soft palate.4 Laryngeal and nasopharyngeal involvement has also been reported in post-kala-azar dermal leishmaniasis.5 Our case presented with classical skin lesions of post-kala-azar dermal leishmaniasis over the chin associated with multiple mucosal lesions in the form of hypertrophy of hard palate and submucosal nodules in nasopharynx and glottis–subglottis region which is an extremely rare finding.
Our patient did not show any parasite in the slit smear. As per the proposed WHO diagnostic algorithm for post-kala-azar dermal leishmaniasis, along with clinical examination, past history of travel or living in an endemic area, past history of visceral leishmaniasis and positive rK39 test indicate a probable post-kala-azar dermal leishmaniasis. The diagnosis should be confirmed by slit smear examination or molecular test for detection of Leishmania parasite.6
The Advisory Panel of World Health organisation and National Vector Borne Disease Control Programme (NVBDCP) recommends the use of miltefosine or amphotericin B for post-kala-azar dermal leishmaniasis patients in India.7 Our patient was treated with miltefosine 50 mg twice daily for 90 days and showed significant improvement in the form of near-complete clearance of the lesions.
Thus, in patients from endemic regions with such rare presentations, leishmanial aetiology should be considered as a differential. Accessibility to diagnosis by polymerase chain reaction should be increased as it provides a specific tool that is most sensitive. Miltefosine has emerged as a preferred treatment with promising efficacy and safety profile.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Post kala azar dermal leishmaniasis in Sudan. East Mediterr Health J. 2001;7:1061-4.
- [PubMed] [Google Scholar]
- Mucosal and peri-orificial involvement in Post-Kala-Azar dermal leishmaniasis. Indian Journal of Dermatology, Venereology, and Leprology. 2004;70:280.
- [PubMed] [Google Scholar]
- Indian mucosal leishmaniasis due to leishmania donovani infection. New England Journal of Medicine. 2008;358:313-5.
- [Google Scholar]
- Post-kala-azar dermal leishmaniasis with an atypical presentation. J Dermatol. 2001;28:341-2.
- [CrossRef] [PubMed] [Google Scholar]
- Laryngeal involvement during post kala-azar dermal leishmaniasis in India. Trop Med Int Health. 1997;2:371-3.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of blood as the clinical specimen for the molecular diagnosis of post-kala-azar dermal leishmaniasis. J Clin Microbiol. 2021;59:e0013221.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- WHO | Post-kala-azar dermal leishmaniasis: a manual for case management and control [Internet]. WHO. World Health organisation; [cited 2020 Jul 2]. Available from: http://www.who.int/neglected_diseases/resources/9789241505215/en/






