Translate this page into:
Prepubertal onset of hidradenitis suppurativa in a girl: A case report and literature review
Correspondence Address:
Jelena M Stojkovic-Filipovic
Pasterova 2, 11000 Belgrade
Serbia
| How to cite this article: Stojkovic-Filipovic JM, Gajic-Veljic MD, Nikolic M. Prepubertal onset of hidradenitis suppurativa in a girl: A case report and literature review. Indian J Dermatol Venereol Leprol 2015;81:294-298 |
Sir,
Hidradenitis suppurativa is a chronic inflammatory disorder characterized by sterile inflamed lesions, folliculitis, abscesses, fibrosis and scarring affecting the axillae, groin and anogenital region. [1] The primary pathogenic event seems to be follicular occlusion in apocrine gland-bearing skin. [1] Despite known predisposing factors, the etiology remains unclear. Though it is a common disease in adults (prevalence 4%) and more frequent in females, it is rare before puberty and after menopause. [1]
We present an 8-year-old Caucasian girl whose lesions commenced at the age of 6 years as painful nodules in the groins, before any signs of puberty. There was no family history of hidradenitis suppurativa or severe acne. Examination revealed few polyporous comedones, red papules, nodules, and atrophic scars in the inguinal regions [Figure - 1]. Axillary and anogenital lesions were absent. She had not attained menarche and the breasts and pubic hair were Tanner stage 2, and body mass index was 23.6 kg/m 2 . Routine laboratory investigations including lipid profile were normal. Fasting glucose, insulin, follicle stimulating hormone, luteinizing hormone, estradiol, testosterone, androstenedione, dehydroepiandrosterone sulfate, sex hormone binding globulin, and prolactin were within normal limits for age. Abdominal and pelvic ultrasonography showed normal adrenal glands and prepubertal uterus and ovaries. Pus cultures were sterile. ELISA for human immunodeficiency virus (HIV) was negative. The mother did not consent for skin biopsy. After the exclusion of bacterial and mycotic infections, a diagnosis of hidradenitis suppurativa was made based on the characteristic clinical presentation. The disease extent was Hurley stage 1. The patient had previously been treated with oral (cephalexin, azithromycin) and topical antibiotics (chloramphenicol, clindamycin, fusidic acid, gentamicin) for 3 weeks with no improvement. In January 2014, oral isotretinoin (0.6 mg/kg/day) and topical 20% azelaic acid cream twice a day were introduced with which marked improvement was noted after 4 weeks, and 2 months later she was in complete remission [Figure - 2]. After 3 months, the isotretinoin dose was reduced to 0.4 mg/kg/day. At the last follow up 7 months after the introduction of isotretinoin, there were no signs of recurrence and the dose was further reduced to 0.3 mg/kg. It is planned to continue isotretinoin for a total of 12 months.
 |
| Figure 1: Hidradenitis suppurativa: Inflamed nodules, papules and atrophic scars involving the groins |
 |
| Figure 2: Complete remission after 3 months of therapy, with residual scarring and hyperpigmentation |
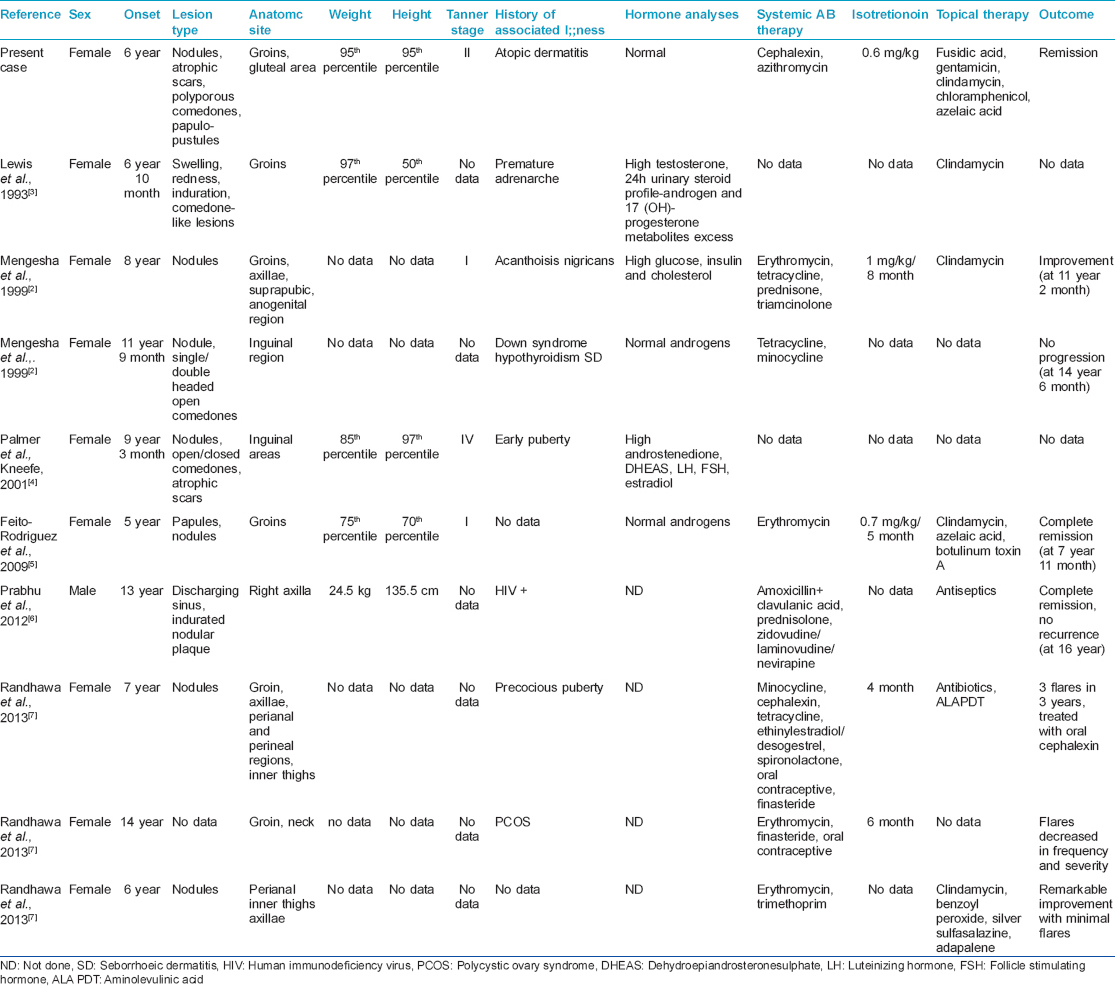
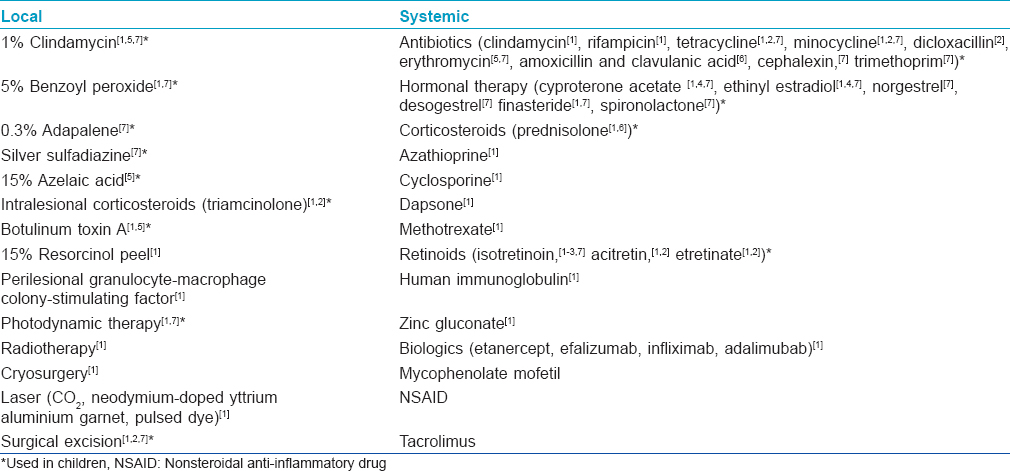
Hidradenitis suppurativa usually develops in the second or third decade of life, with a female: male ratio of 2:1 to 5:1. [1],[2] We found only nine previous reports of hidradenitis suppurativa in children, [2],[3],[4],[5],[6],[7] of which eight were girls [Table - 1]. Though the average age of onset in adults is 23 years; [1] in pediatric cases the mean age of onset was 8 years and 9 months (range 5-14 years). The main clinical presentation in pediatric cases were nodules in 7 (77.8%) of 9 children [2],[4],[5],[6],[7] and clinical features in prepubertal cases were not different from adults. In adults this condition affects intertriginous apocrine gland-bearing areas; most frequently the genito-femoral region in women. [1] In children, groins were reported as the most common site involved in 7 (77.8%) patients. Other localizations (axillae, [2],[7] perianal region, [7] inner thighs, and posterior neck [7] ) were noted only in one HIV-positive boy and two girls, and these were refractory to several treatment modalities [Table - 1]. Positive family history was reported in 26% of adults (autosomal-dominant mode of inheritance) [1] and in 3 (33.3%) children. HLA associations were not demonstrated. [1],[4] In adults, the importance of hormones has not been fully elucidated and hyperandrogenism most likely does not play a role. [1] Only 3 (33.3%) children had some hormonal abnormalities [2],[3],[4] [Table - 1]. Abdomino-pelvic ultrasonography has been performed only in our patient and a girl with premature adrenarche, [3] and was normal in both cases. The role of bacteria is unclear; as secondary colonizers, they might exacerbate the condition. [1] Among children, Gram-positive bacteria were found in 3 (33.3%) patients. [2],[5],[6] Obesity is strongly associated with the disease in adults, [1] different from children, where it has been reported only in one girl. [3] Despite multiple treatment options [Table - 2], no single uniformly effective therapy has been established. [1] Early disease is often treated with antibiotics. In children, the most commonly used oral antibiotic was erythromycin in 4 (44.4%) cases. As the second option, isotretinoin has been tried in 4 (44.4%) cases (0.7-1 mg/kg), for 4-8 months. In 2 (22.2%) children, surgical excision was undertaken. [2],[7] Other treatment modalities (botulinum toxin A, finasteride) [5],[7] have been tried in children, but the real efficacy is difficult to estimate since none of these was used as monotherapy. Only one child has been treated with topical 15% azelaic acid cream. [5] According to the outcomes of reported cases of prepubertal onset [Table - 1], the prognosis might be better than in adults, but the number of cases is too few to make a definitive comment on this.
Although rare in prepubertal children, hidradenitis suppurativa should be considered in the differential diagnosis of furunculosis-like inguinal/axillary lesions, combination of oral isotretinoin and topical azelaic acid cream may be a useful treatment option in children.
ACKNOWLEDGMENT
The Ministry of Science of the Republic of Serbia, supported Milos Nikolic and Mirjana Gajic-Veljic, Grant No 175065.
| 1. |
Zouboulis C, Tsatsou F. Disorders of the apocrine sweet glands. In: Goldsmith LA, editor. Fitz-patrick's dermatology in general medicine. 8 th ed. New York: The McGraw-Hill; 2012. p. 2350-2.
th ed. New York: The McGraw-Hill; 2012. p. 2350-2.'>[Google Scholar]
|
| 2. |
Mengesha YM, Holcombe TC, Hansen RC. Prepubertal hidradenitissuppurativa: Two case reports and review of the literature. Pediatr Dermatol 1999;16:292-6.
[Google Scholar]
|
| 3. |
Lewis F, Messenger AG, Wales JK. Hidradenitissuppurativa as a presenting feature of premature adrenarche.Br J Dermatol 1993;129:447-8.
[Google Scholar]
|
| 4. |
Palmer RA, Keefe M. Early-onset hidradenitissuppurativa. Clin Exp Dermatol 2001;26:501-3.
[Google Scholar]
|
| 5. |
Feito-Rodríguez M, Sendagorta-Cudós E, Herranz-Pinto P, de Lucas-Laguna R. Prepubertal hidradenitissuppurativa successfully treated with botulinum toxin A. Dermatol Surg 2009;35:1300-2.
[Google Scholar]
|
| 6. |
Prabhu G, Laddha P, Manglani M, Phiske M. Hidradenitissuppurativa in a HIV-infected child. J Postgrad Med 2012;58:207-9.
[Google Scholar]
|
| 7. |
Randhawa HK, Hamilton J, Pope E. Finasteride for the treatment of hidradenitissuppurativa in children and adolescents. JAMA Dermatol 2013;149:732-5.
[Google Scholar]
|
Fulltext Views
6,417
PDF downloads
2,157





