Translate this page into:
Pretibial myxedema, ophthalmopathy and acropachy in a male patient with Graves� disease
Correspondence Address:
S Veeranna
Department of Skin and STD, J.S.S.Hospital, Mysore, Karnataka - 570004
India
| How to cite this article: Veeranna S, K, Betkerur J, S. Pretibial myxedema, ophthalmopathy and acropachy in a male patient with Graves� disease. Indian J Dermatol Venereol Leprol 2004;70:380-382 |
 |
 |
 |
 |
Sir,
The thyroid gland plays an important role in the maintenance of normal cutaneous function. Five per cent of men and 15% of women with thyroid dysfunction show cutaneous changes.[1] Graves′ disease is the most common cause of hyperthyroidism, affecting 15-50 of 100000 people per year, mostly females.[2] Classical findings include thyroid swelling, exophthalmos, pretibial myxedema and acropachy.[2] We report a man presenting with all the features.
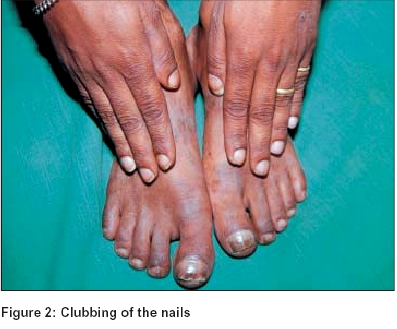
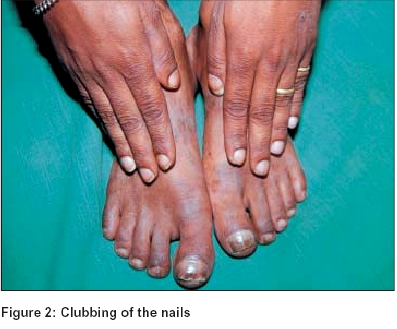
A 29-year-old man presented with a history of asymptomatic swelling over the legs for the past 2 years. It was gradual in onset and progressive in nature. There was no history of trauma, excessive sweating, heat intolerance or loss of appetite. The patient had undergone thyroidectomy 2½ years back for Graves′ disease. Skin examination revealed multiple well-defined plaques and nodules of varying size situated bilaterally over the tibia. The overlying skin was waxy and indurated with some areas of hyperpigmentation [Figure - 1]. There was clubbing of the nails with thickened periungual skin [Figure - 2]. The patient also had exophthalmos.
Routine blood and urine examinations were normal. Thyroid function tests showed decreased T3 (0.30 ng/ml) and T4 (2.10 mg/ml) and increased TSH (39.41 mIU/ml) levels, suggestive of hypothyroidism. A skin biopsy specimen from the pretibial skin showed normal epidermis, marked dermal pallor due to mucin deposition and dispersed stellate shaped fibroblasts, findings suggestive of myxedema.
The patient was put on oral thyroxin and received 5 doses of intralesional triamcinolone, 0.5-1 ml per lesion, with marked improvement in the skin lesions. Later, a high potency steroid ointment was used.
Graves′ disease is an autoimmune disease of the thyroid gland with IgG antibodies against TSH-R.[2] The triad of ophthalmopathy, dermopathy and acropachy tends to occur chronologically in the course of the disease.[2] Graves′ ophthalmopathy is found in 30-45% of patients. It can manifest as lid lag, exophthalmos, strabismus, lagophthalmos or optic neuropathy.[2]
Pretibial myxedema is also known as thyroid dermopathy.[3] Clinically it may present as non-pitting edema, nodules and tuberous lesions, or the elephantiasic type.[4] The overlying skin is waxy and translucent with a ′peau d′orange′ appearance. There may be overlying hypertrichosis or hyperhidrosis. Common sites of affection are the pretibial area, arms, shoulders, and neck.[4] It may not be related to levels of thyroxin.[3] Correction of thyrotoxicosis has no effect on skin lesions.[5] It occurs in 4% of patients of hypothyroidism.[2] It can also be seen in Hashimoto′s thyroiditis and in euthyroid states.[3] Dermopathy in Graves′ disease may occur many years after ophthalmopathy.[2]
The exact pathogenesis of dermopathy is not known. However, the orbital and pretibial fibroblasts are probably the targets of autoimmune attack.[2] Thyrotropin receptor antibody binding sites have been demonstrated in pretibial fibroblasts, and, these may be stimulated to produce high amounts of hyaluronic acid. According to another theory, T cells that react with thyrotropin receptors on fibroblasts may cause cytokine-induced production of hyaluronic acid.[2]
Acropachy is a rare component of the triad, with an incidence of 0.8 to 1%. It can manifest up to 25 years after the onset of thyroid disease and may even appear after its treatment.[2] It is characterized by digital clubbing, periosteal bone proliferation, and soft tissue swelling.
Treatment of thyroid dermopathy includes steroids (topical, intralesional or under occlusion), compressive stockings,[3] pentoxifylline, gamma globulin, plasmapheresis, surgery and radiotherapy.[2] Recently octreotide, a somatostatin analog, was found to be effective in improving ophthalmopathy.[3] Acropachy, being asymptomatic, doesn′t require treatment. Partial or complete remission may occur in time.[3] Options for therapy include excision, hyaluronidase, local radiotherapy and topical potent steroids.[3]
| 1. |
Rosen T, Kleman GA. Thyroid and the skin. In: Callen JP, editor. Dermatological signs of internal disease. 2nd Ed. Philadelphia: WB Saunders; 1995. p. 189-95.
[Google Scholar]
|
| 2. |
Anderson CK, Miller OF. Triad of exophthalmos, pretibial myxedema and acropachy. J Am Acad Dermatol 2003;48:970-2.
[Google Scholar]
|
| 3. |
Julia Ai, Leonlordt, Warren H, Janie M. Autoimmune thyroiditis etiology pathogenesis and dermatological manifestations, J Am Acad Dermatol 2003;48:641-59.
[Google Scholar]
|
| 4. |
Weisman K, Graham RM. Systemic disease and the skin. In: Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Rook-Wilkinson-Ebling Textbook of Dermatology, Vol 3. 6th Ed. London: Blackwell; 1998. p. 2703-18.
[Google Scholar]
|
| 5. |
Freinkel RK. Other endocrine disorders. In: Freedberg IM, Eisen AZ, Wolff K, Austen FK, Goldsmith LA, Katz SI, et al. editors. Dermatology in internal medicine, 5th Ed. New York: McGraw Hill; 1999. p. 1976-8.
[Google Scholar]
|
Fulltext Views
6,035
PDF downloads
1,895





