Translate this page into:
Prevalence of onychomycosis in patients with diabetes mellitus: A cross-sectional study from a tertiary care hospital in North India
Corresponding author: Dr. Archana Singal, Department of Dermatology & STD, University College of Medical Sciences & GTB Hospital, Delhi, India archanasingal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal S, Singal A, Grover C, Das S, Arora VK, Madhu SV. Prevalence of onychomycosis in patients with diabetes mellitus: A cross-sectional study from a tertiary care hospital in North India. Indian J Dermatol Venereol Leprol 2023;89:710-7
Abstract
Background
Though diabetes mellitus (DM) is a well-recognised risk factor for onychomycosis (OM), the epidemiology of OM in diabetic patients remains largely unexplored, especially from the Indian subcontinent.
Aims and objectives
To estimate the prevalence of OM in diabetic patients, to identify and analyse risk factors, and correlate the severity of nail changes with glycemic control (HBA1c).
Methods
This cross-sectional, analytical study involved 300 diabetic patients. Patients with the clinical diagnosis of OM, supplanted by at least two of the four tests (KOH, culture, onychoscopy and nail histopathology) were considered cases of OM. Demographic and haematological profile was analysed using chi-square test/ Fischer’s exact test. Logistic regression was applied to assess the independent risk factors.
Results
The prevalence of OM in DM patients was 34% (102/300) and significant risk factors included; age >60 years, male gender, closed shoes, disease duration >5 years, high BMI (>25) and lack of awareness about nail changes. Distal and lateral subungual OM (78%) was the commonest presentation followed by proximal subungual OM, superficial OM and total dystrophic OM. Correlation between HbA1c and the number of nails involved was found to be significant.
Limitation
As cases were recruited from a hospital setting, there could be chances of Berksonian bias.
Conclusion
The prevalence of OM in diabetic patients is high and the severity of nail changes correlates with HbA1C levels. It is important to diagnose OM early in order to treat and prevent complications.
Keywords
Onychomycosis
prevalence
diabetes mellitus
dermatophytosis
Plain Language Summary
The epidemiology of onychomycosis (OM) in diabetic patients is largely unexplored. This cross-sectional analytical study was conducted in 300 diabetic patients to estimate the prevalence of OM, identify and analyse the risk factors and correlate the severity of nail changes with glycemic control. Demographic and haematological profiles were recorded, and analysed using Chi square test/ Fischer’s exact test. Logistic regression was applied to assess the independent risk factors for OM. We found a 34% prevalence of OM in diabetes mellitus (DM) patients, with age >60 years, male gender, closed shoes, disease duration >5 years, high BMI (>25) and lack of awareness about nail changes as significant risk factors. Distal and Lateral Subungual OM was the most common type of OM. There was a significant correlation between HbA1c and the number of nails involved.
Introduction
Onychomycosis (OM) accounts for 40–50% of all onychopathies with a worldwide prevalence of 5%. 1 India, which is considered the world capital of diabetes has a 0.5–5% prevalence of OM. 2 Risk factors associated with OM include diabetes mellitus (DM), peripheral arterial disease, immunosuppression, tinea pedis, smoking, recurrent trauma, psoriasis, sharing of public bathing facilities, etc. 3
DM is a metabolic disorder with a rising global prevalence; 4 In India, the total number of diabetics is around 61.3 million and this is further estimated to rise to 101.2 million by the year 2030. 4 Though DM is an established risk factor for OM, its clinico-epidemiological and mycological characteristics in a diabetic population remain largely unexplored, in particular from the Indian subcontinent.
The present study aimed to assess the prevalence of OM in diabetic patients. The objectives were to identify and analyse the risk factors for OM and to establish a correlation between the number of nails involved and glycemic control (levels of HBA1c) if any.
Materials and methods
This cross-sectional analytical study was conducted in the Departments of Dermatology and Endocrinology at the University College of Medical Sciences, New Delhi, India from November 2018 to April 2020, after getting ethics committee approval. Appropriate nail samples were sent for investigations to the departments of microbiology and pathology.
Based on the published prevalence of OM in 17% of diabetic patients, 5 a sample size of 270 was calculated with an allowable absolute error of 4.5% and confidence interval (CI) of 95%. However, assuming a 10% non-response rate, the patient number was finalised at 300.
Three hundred consecutive diabetic patients (type 1 and 2) attending the outpatient Departments of Dermatology and Endocrinology constituted the study population.
After written informed consent was obtained, detailed history was taken (age of onset of DM, duration, type of DM, treatment, risk factors and co-morbidities) followed by thorough examination and haematological investigations, and findings were recorded on a pre-designed proforma. Nails were cleansed with sterile alcohol to look for any clinical evidence of OM (onycholysis, subungual hyperkeratosis, chromonychia, nail plate thickening and dystrophy). A representative nail with suspected OM was thus identified and clinical photographs were taken. The severity of nail involvement was calculated based on the number of affected nails (mild- <3, moderate- 4–6 and severe- >6 nails) and was correlated with the patient’s glycosylated haemoglobin (HbA1c) level.
Case definition
The patient was said to have OM if the clinical findings of OM were corroborated with at least two or more positive tests, viz onychoscopy, direct microscopic examination (DME) in KOH, fungal culture and histopathology with PAS staining.
Onychoscopy was performed using Dinolite AM 7515 MZT dermatoscope (New Taipei city, Taiwan, 20x-220x) on all the nails with isopropyl alcohol as interface medium. The presence of spiked pattern and subungual hyperkeratosis with or without ruinous aspects were considered to be characteristic features indicative of the distal and lateral subungual onychomycosis (DLSO) variant of OM. 6 For the endonyx variant, the dendritic pattern was considered a positive diagnostic feature. 7 The diagnostic criteria used for proximal subungual onychomycosis (PSO) were proximal onycholysis and homogenous opacity; superficial onychomycosis (SO) was diagnosed based on homogenous opacity without subungual hyperkeratosis and total dystrophic onychomycosis (TDO) was diagnosed by the presence of both ruinous aspects and longitudinal striae. 6
Nail clippings from appropriate sites were collected for DME in 40% KOH. A part of the nail clipping was sent in a sterile envelope for inoculation on Sabouraud’s dextrose agar (SDA) with and without chloramphenicol (0.05 gm/L), gentamycin (20 mg/l) and cycloheximide (0.5 gm/L), at 25 degrees celsius for optimal growth. In the case of growth, colony characteristics were studied on lactophenol cotton blue (LPCB) mount preparation. The culture was considered negative if no growth was observed after four weeks of incubation. Nail clipping was also sent for histopathology (H&E and PAS staining); the presence of subungual hyperkeratosis, hyphae in the nail lamellae and fungal elements in the stratum corneum were considered diagnostic of onychomycosis. 6
Statistical analysis
The data was analysed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). Comparative analysis was done using chi-square test of significance/Fischer’s exact test and P < 0.05 was considered significant. Logistic regression was applied to calculate the significant risk factors for OM in the studied patients.
Results
Of the 300 consecutive diabetic patients that were screened, 122 (40.7%) were suspected to have OM. However, based on the case definition, the diagnosis of OM was confirmed in 102 (34%) patients.
The prevalence of OM was significantly higher (P < 0.001) in males than females (61.8% vs. 38.2%, M: F = 1.6:1). The mean age of the 102 cases was 57.16 + 11.15 years (range 26–80 years), which was significantly higher (P < 0.001) than that of the OM negative group (57.16 vs. 50.85 years) [Table 1].
*P-value less than 0.05 is considered significant, NS: not significant, HIV: human immunodeficiency virus, OM: onychomycosis
Risk factor
OM positive cases (N = 102)
OM negative cases (N = 198)
P-value
Frequency n (%)
Frequency n (%)
Age group (years):
<0.001*
<40
8 (7.8)
47 (23.7)
41–59
40 (39.3)
79 (39.9)
>60
54 (52.9)
72 (36.4)
Type of diabetes:
0.173 (NS)
1
1 (1)
(4)
2
101 (99)
190 (96)
H/O closed shoes:
0.001*
Yes
46 (45)
51 (25.8)
No
56 (55)
147 (74.2)
Gender:
<0.01*
Male
63 (61.8)
64 (32.3)
Female
39 (38.2)
134 (67.7)
H/O sports:
0.341 (NS)
Yes
3 (2.9)
2 (1)
No
99 (97.1)
196 (99)
H/O trauma:
0.094 (NS)
Yes
34 (33.3)
48 (24.2)
No
68 (66.7)
150 (75.8)
H/O Peripheral vascular disease:
0.115 (NS)
Yes
4 (3.9)
2 (1)
No
98 (96.1)
196 (99)
HIV:
0.550 (NS)
Yes
0 (0)
2 (1)
No
102 (100)
196 (99)
Hyperhidrosis:
0.083 (NS)
Yes
31 (30.4)
80 (40.4)
No
71 (69.6)
118 (59.6)
H/O surgery:
0.903 (NS)
Yes
20 (19.6)
40 (20.2)
No
82 (80.4)
158 (79.8)
Concomitant tinea infection:
0.242 (NS)
Yes
35 (34.3)
55 (27.8)
No
67 (65.7)
143 (72.2)
Lack of awareness about nail changes:
<0.001*
Yes
32 (31.4)
8 (4)
No
70 (68.6)
190(96)
On immunosuppressive:
0.185 (NS)
Yes
4 (3.9)
2 (1)
No
98 (96.1)
196 (99)
Peripheral neuropathy:
0.893 (NS)
Yes
41 (40.2)
78 (39.4)
No
61 (59.8)
120 (60.6)
Body mass index:
0.05*
Underweight
2 (2)
1 (0.5)
Normal
18 (17.6)
17 (8.6)
Overweight
14 (13.7)
26 (13.1)
Obese
68 (66.7)
154 (77.8)
The duration of diabetes in the study participants ranged from 2.5 months to 480 months. For OM-positive cases, the median duration was significantly higher than in OM-negative cases (60 months vs. 36 months, P = 0.02).
Almost 50% of OM-positive cases had mild nail involvement with <3 nails involved. Seventeen (16.7%) cases had a moderate degree of nail involvement while severe nail involvement (>6 nails) was present in 34 (33.3%). DLSO was the most common morphological variant in 80/102 (78.4%) patients [Figure 1a], followed by the mixed variant in 10 (9.8%) [Figure 1b] and Endonyx in 5 (4.9%) cases [Figure 1c], while TDO, PSO [Figure 1d] and SO were present in 4 (3.9%), 1 (1%) and 2 (2%) of cases, respectively.

- Distal and lateral subungual onychomycosis with chromonychia

- Mixed variant of onychomycosis

- Endonyx onychomycosis (Black arrow)

- Proximal subungual onychomycosis
Multiple co-morbidities were observed in all the patients included in the study. Among the OM-positive cases, hypertension and peripheral neuropathy were present in 45 (44.1%) and 41 (40.2%) cases, respectively.
Risk factors predisposing to OM were analysed [Table 1]. Both peripheral vascular disease and peripheral neuropathy, though considered predisposing factors for OM in DM, were not found to be significant in our study. History of participation in sports, trauma, immunosuppressive therapy, hyperhidrosis, HIV and concomitant tinea infection were also not found to be significant predisposing factors for OM.
A multivariate binomial logistic regression analysis was carried out to know the independent risk factors for OM [Table 2].
*P-value less than 0.05 is considered significant, OM: onychomycosis, CI: confidence interval, NS: not significant
Independent variable
Prevalence of OM
Adjusted odds ratio (95% CI)
P-value
Yes n (%)
No n (%)
Gender:
0.013*
Male
63 (61.8)
64 (32.3)
2.256 (1.19–4.278)
Female
39 (38.2)
134 (67.7)
Reference
H/O closed shoes:
0.592 (NS)
Yes
46 (45)
51 (25.8)
1.212 (0.600–2.446)
No
56 (55)
147 (74.2)
Reference
Lack of awareness about nail change:
<0.001*
Yes
32 (31.4)
8 (4)
8.583 (3.463–21.272)
No
70 (68.6)
190 (96)
Reference
Age (years):
0.085 (NS) 0.015*
≤40
8 (7.8)
47 (23.7)
Reference
41–59
40 (39.3)
79 (39.9)
2.266 (0.894–5.742)
≥60
54 (52.9)
72 (36.4)
3.229 (1.255–8.309)
The correlation between levels of HbA1c and the number of nails involved was found to be statistically significant (P = 0.014 and correlation coefficient (r) = 0.141). On applying the ANOVA test, the HbA1C was found to be significantly higher in patients with severe nail involvement (P = 0.03) [Table 3].
*P-value less than 0.05 is considered significant, SD: standard deviation
Nail changes
Frequency
Mean (SD) HbA1c
F
P-value
No involvement
178
8.92 (2.15)
3.024
0.03*
Mild involvement(≤3 nails)
64
9.39 (2.09)
Moderate involvement(4–6 nails)
21
9.29 (1.86)
Severe involvement(>6 nails)
37
10.12 (3.38)
Total
300
9.19 (2.33)
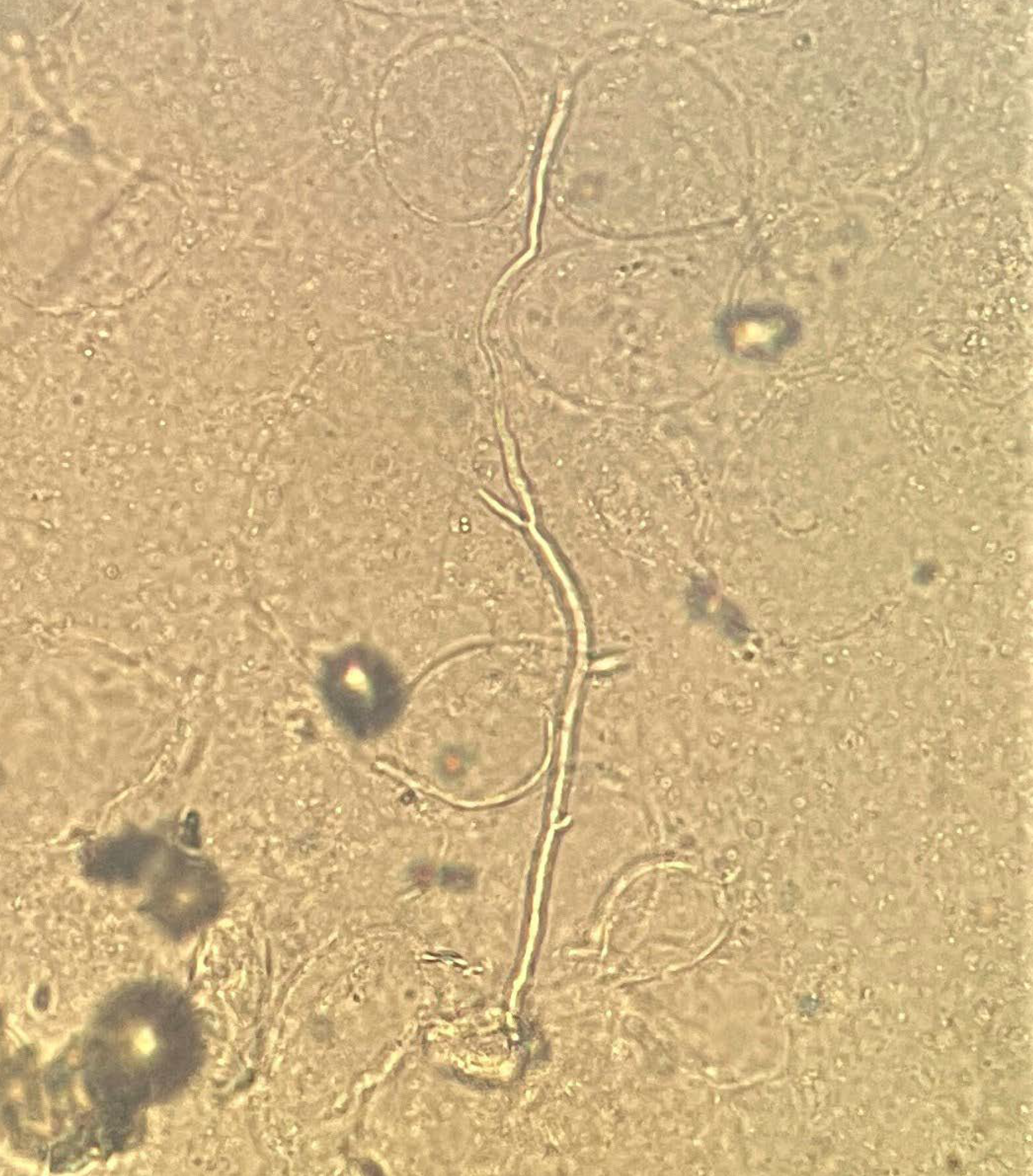
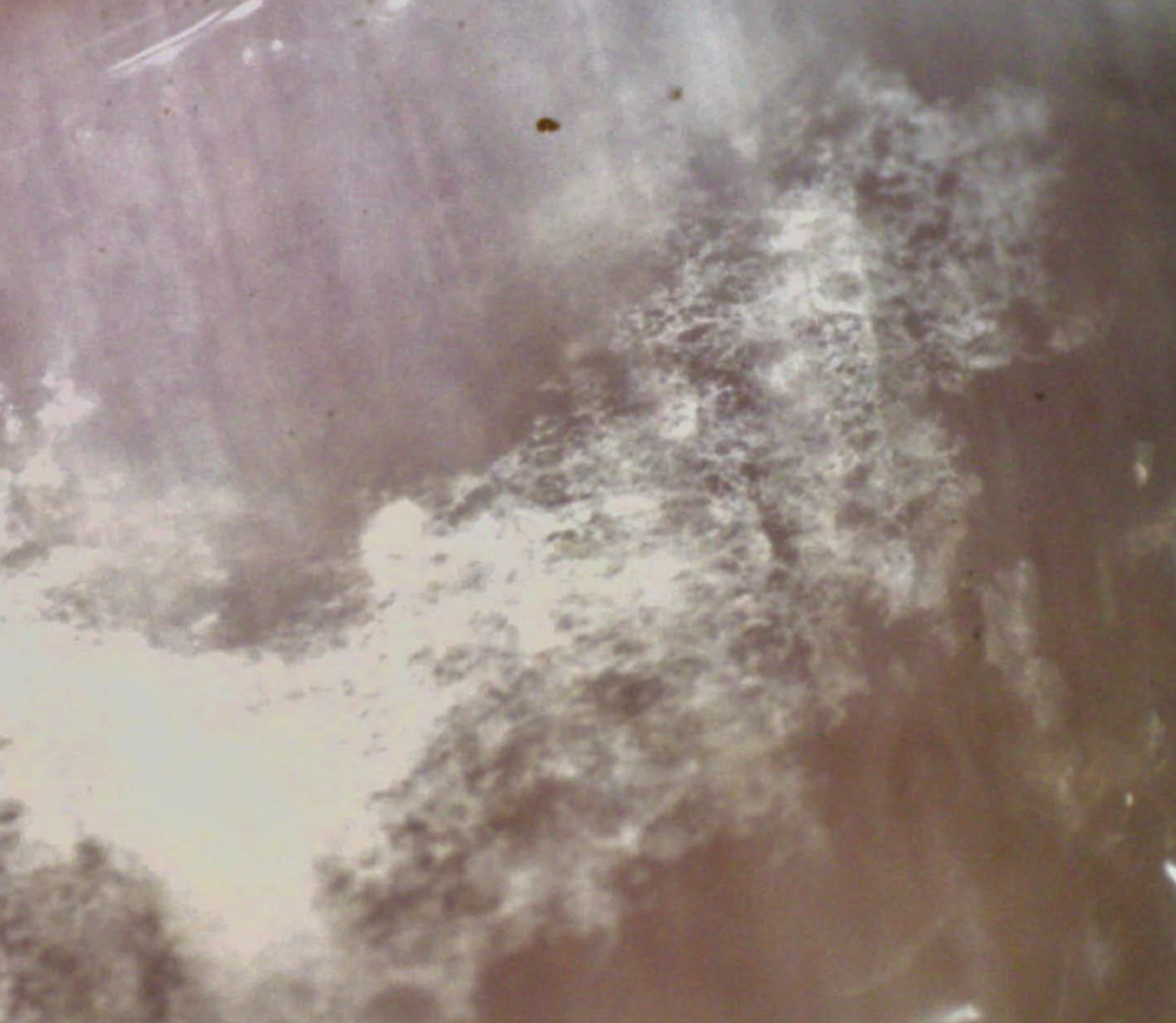
The positivity of different diagnostic modalities used varied in the 102 OM-positive cases [Figure 2]; DME with KOH was positive in 87 (85.3%) [Figures 3a and b], histopathology with PAS in 70 (68.6%) [Figures 4a and b], onychoscopy in 58 (56.9%) [Figures 5a to d) and mycological culture in 57 (55.9%) [Figures 6a to d].
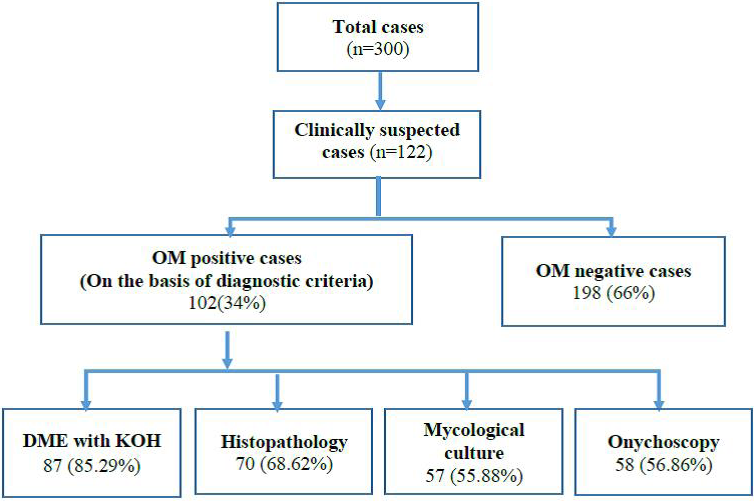
- Flowchart depicting the results of various diagnostic modalities
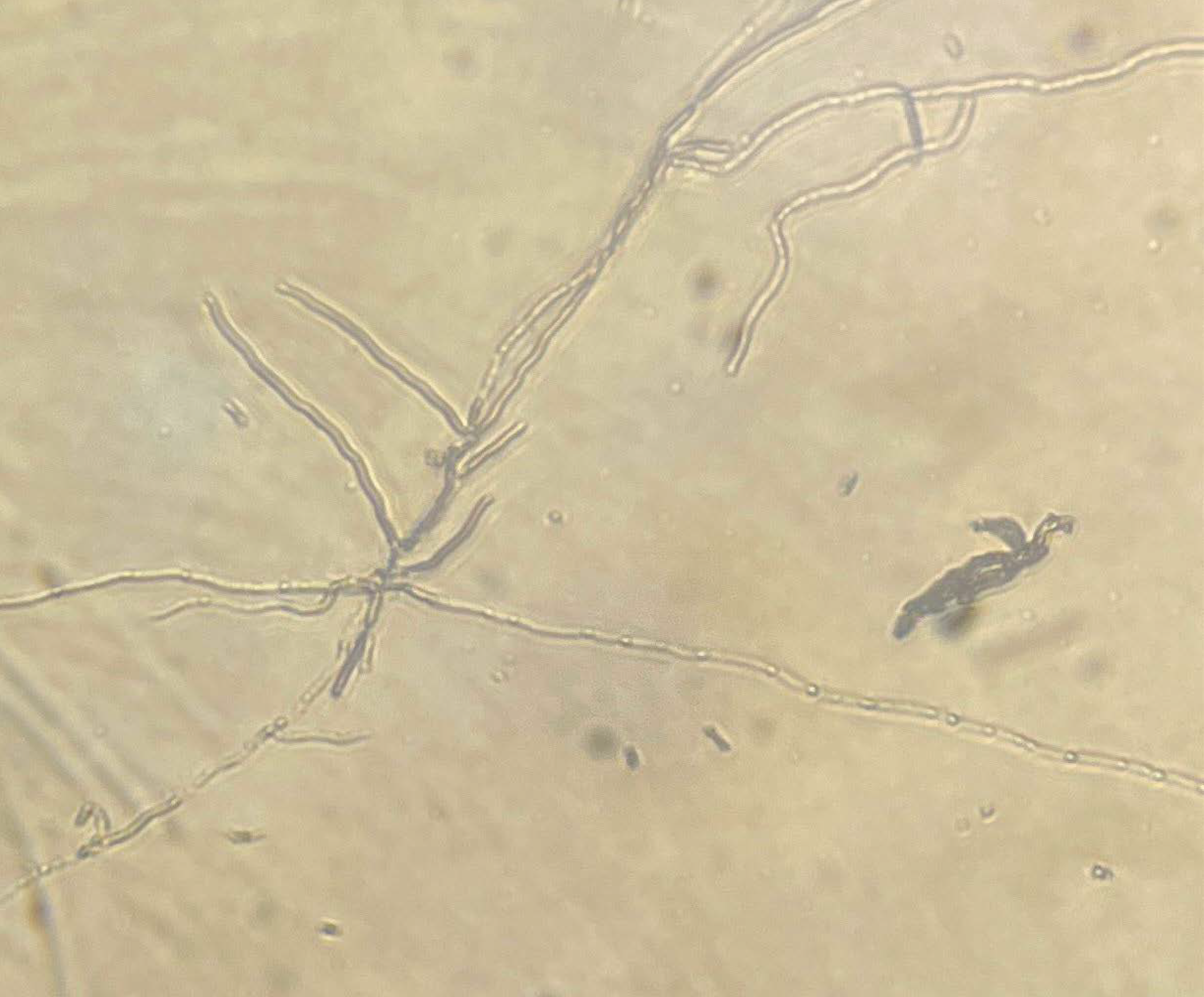
- DME with KOH showing multiple branched and filamentous septate hyphae
- DME with KOH showing multiple pseudohyphae suggestive of Candida species
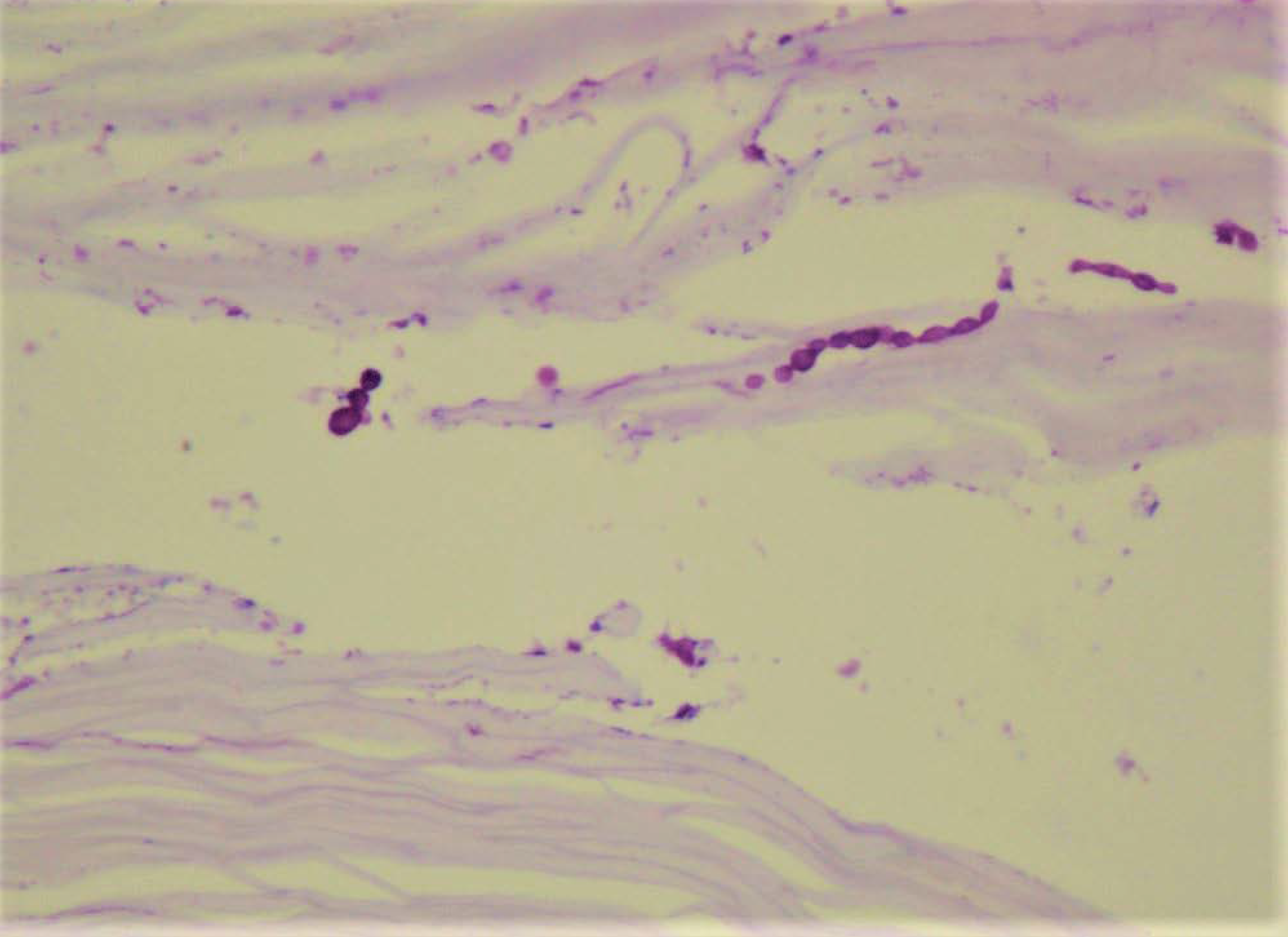
- Histopathology with PAS: Pesudohyphae and ovoid to round yeast forms of Candida species in the hypertrophic stratum corneum and underlying nail plate (PAS, 400x)
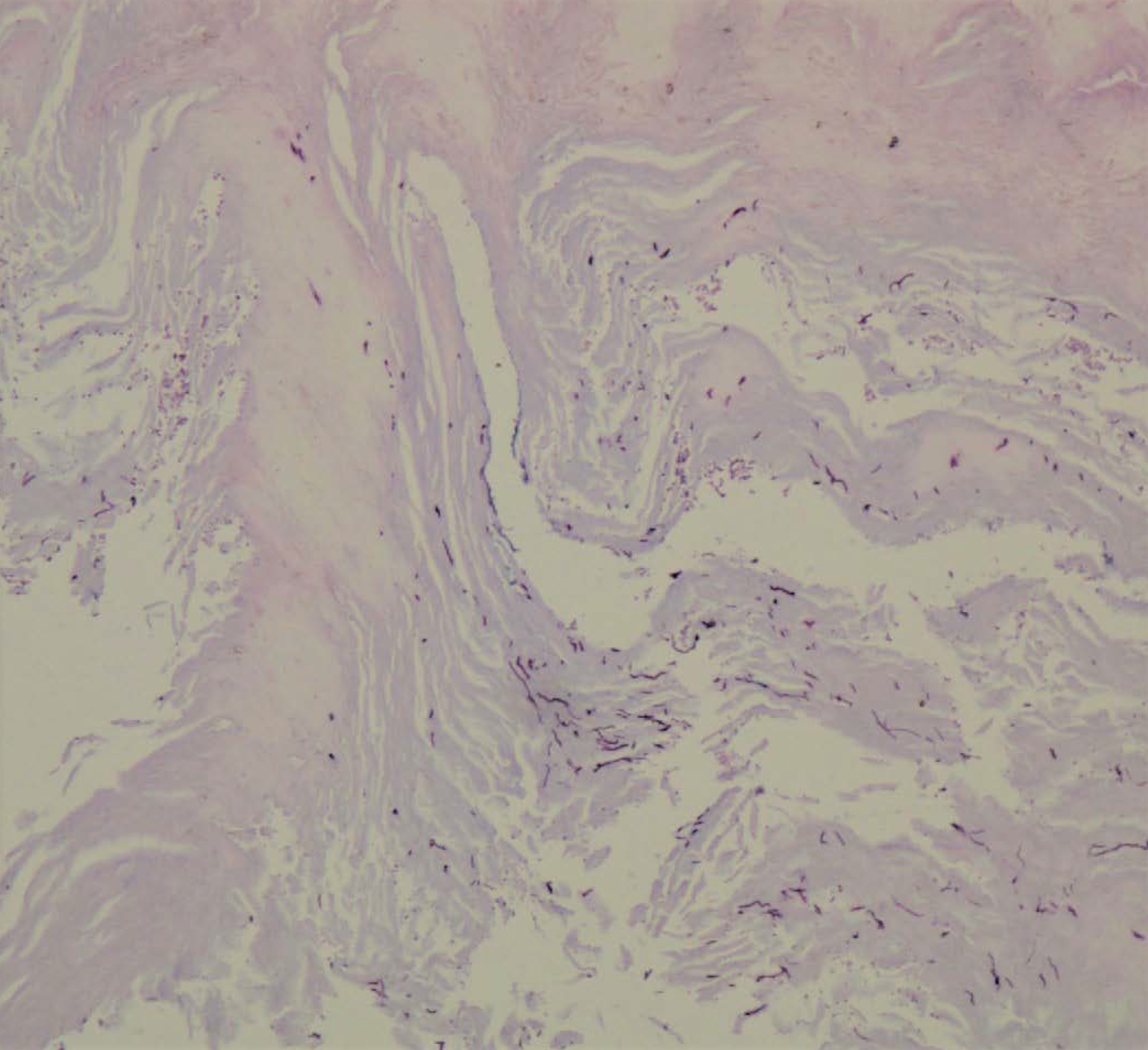
- Histopathology with PAS: Thin regular fungal hyphae in the stratum corneum of nail plate (PAS, 100x)
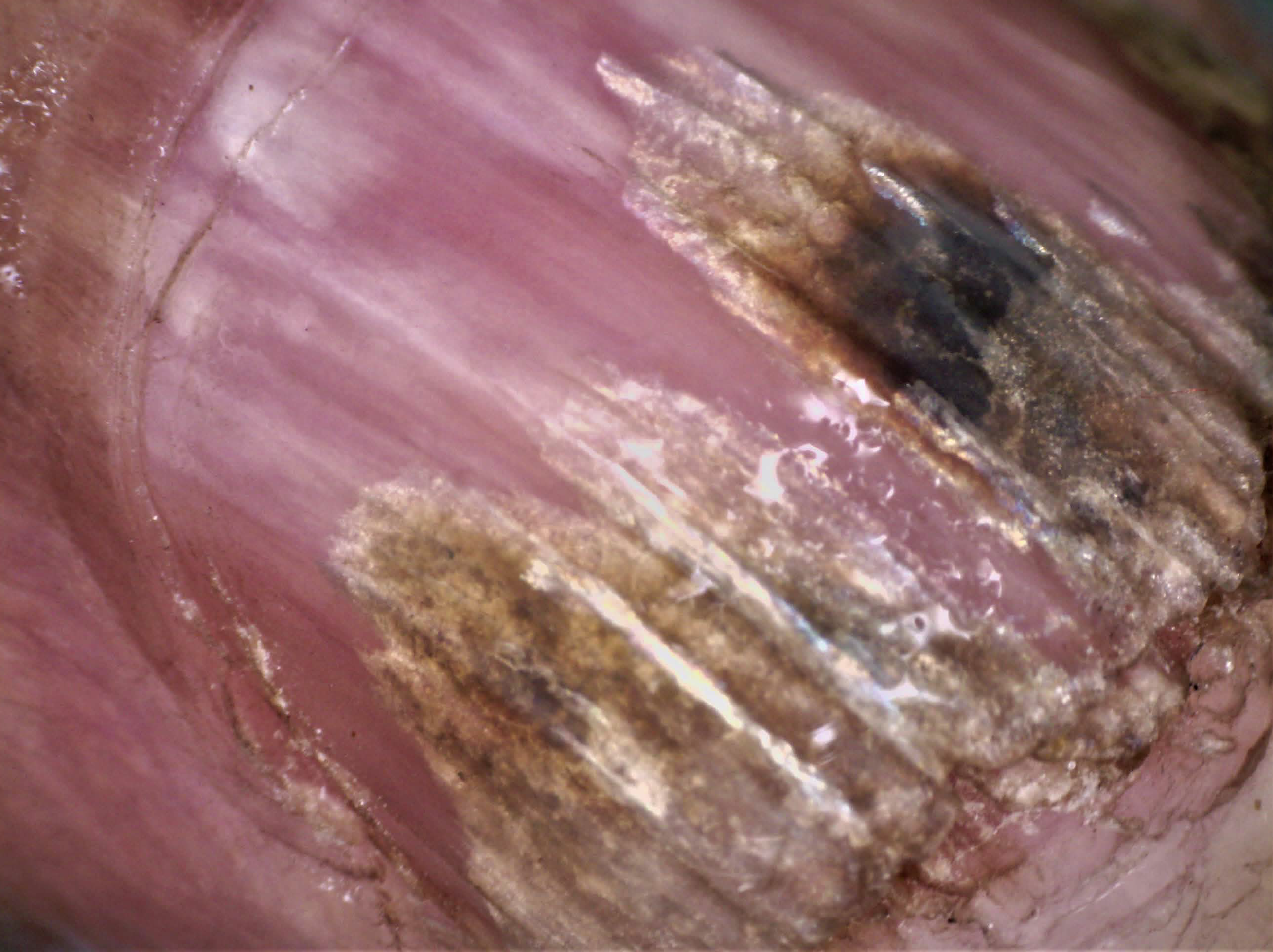
- Onychoscopy of the nail plate (polarised) showing distal onycholysis with proximal jagged pattern and chromonychia with Aurora Borealis pattern
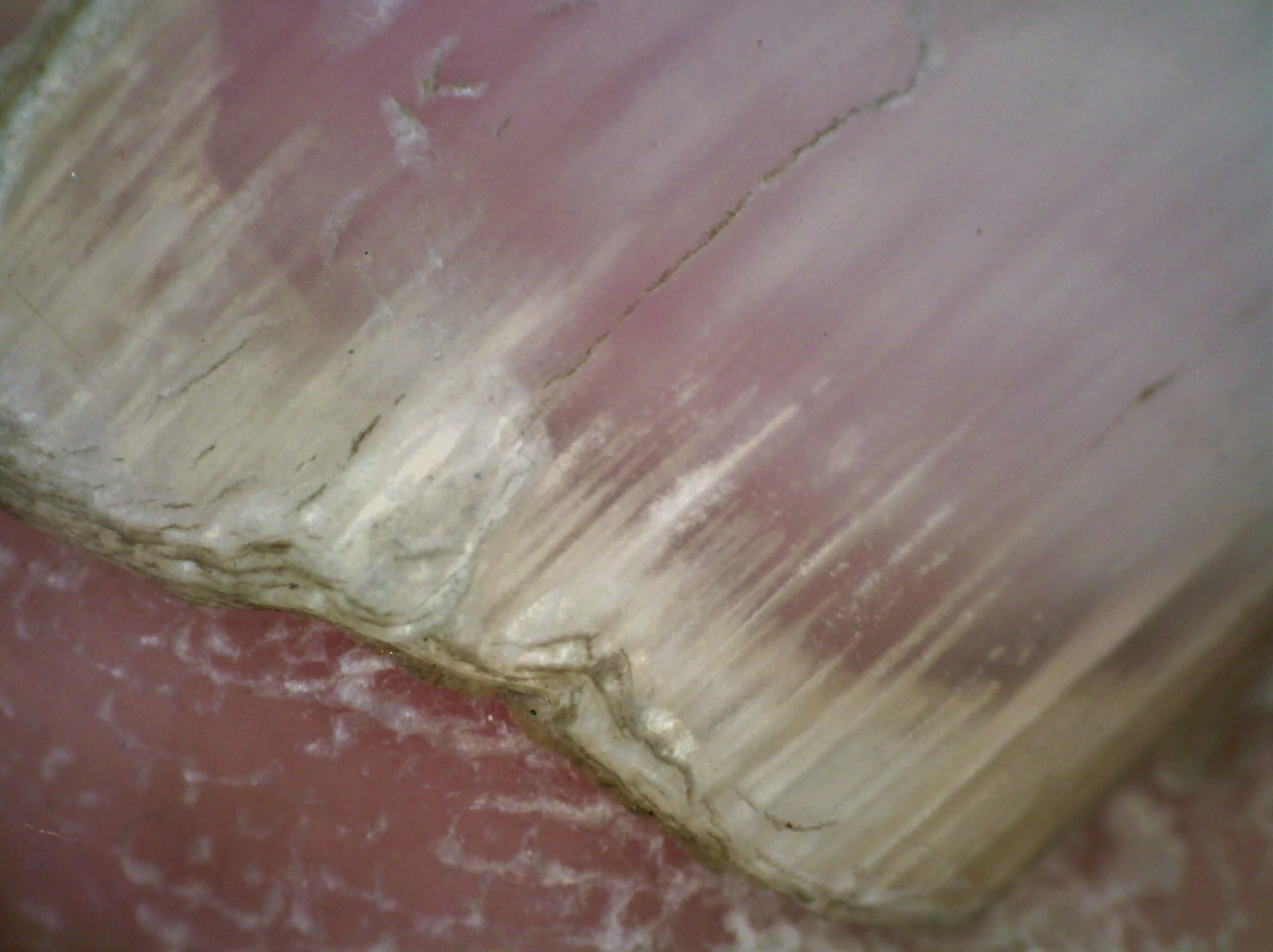
- Distal onycholysis with spiked pattern
- Endonyx onychomycosis showing a dendritic pattern

- Thickened nail plate with distal irregular termination and ruinous subungual hyperkeratosis

- Inoculation tubes showing the growth of various fungi

- DME with LPCB mount showing growth of Aspergillus versicolor (long transparent and septate hyphae with biseriate conidiophores)
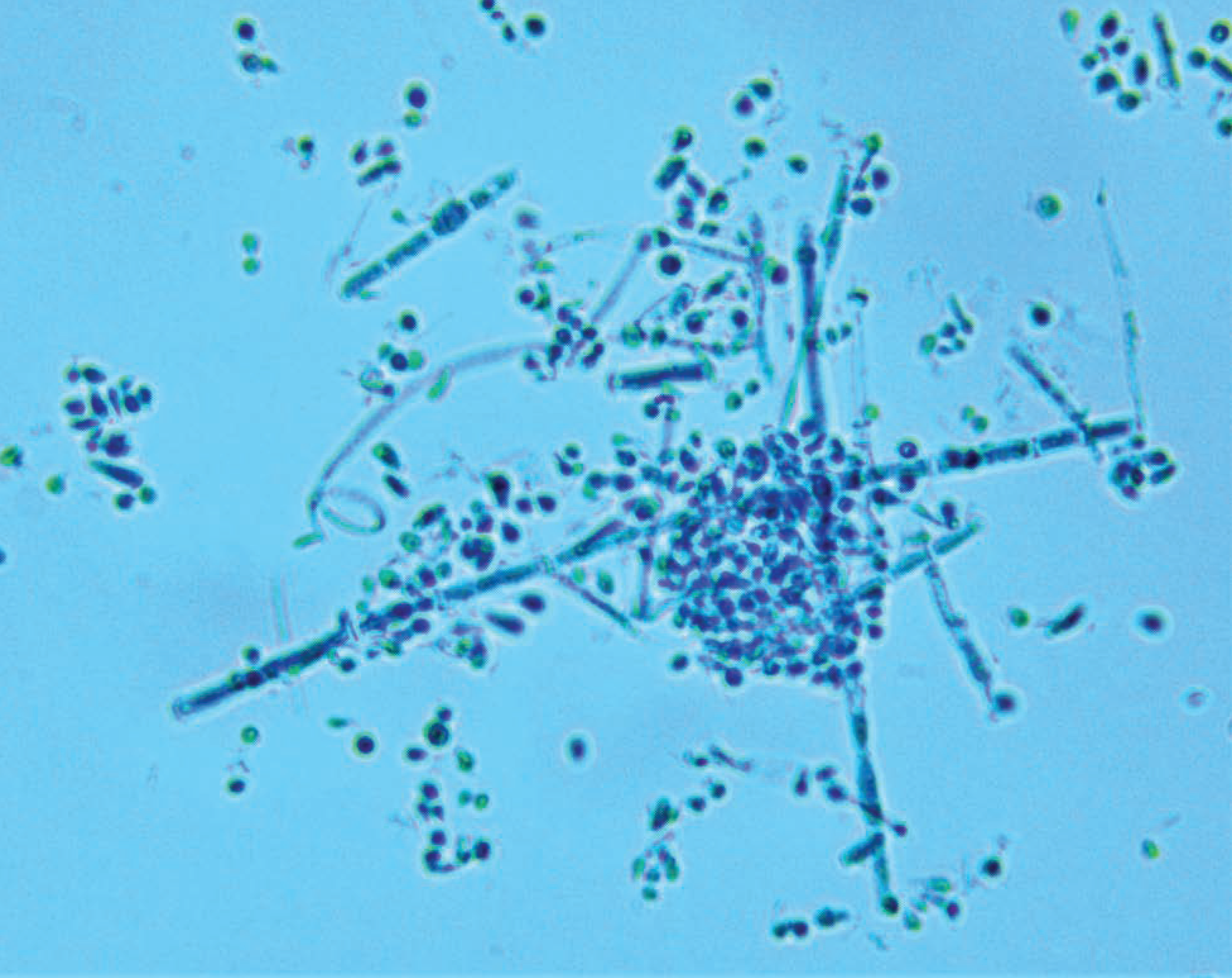
- DME with LPCB mount showing numerous single-celled microconidia in dense clusters (hyaline and smooth-walled) with spherical chlamydospores and spiral hyphae
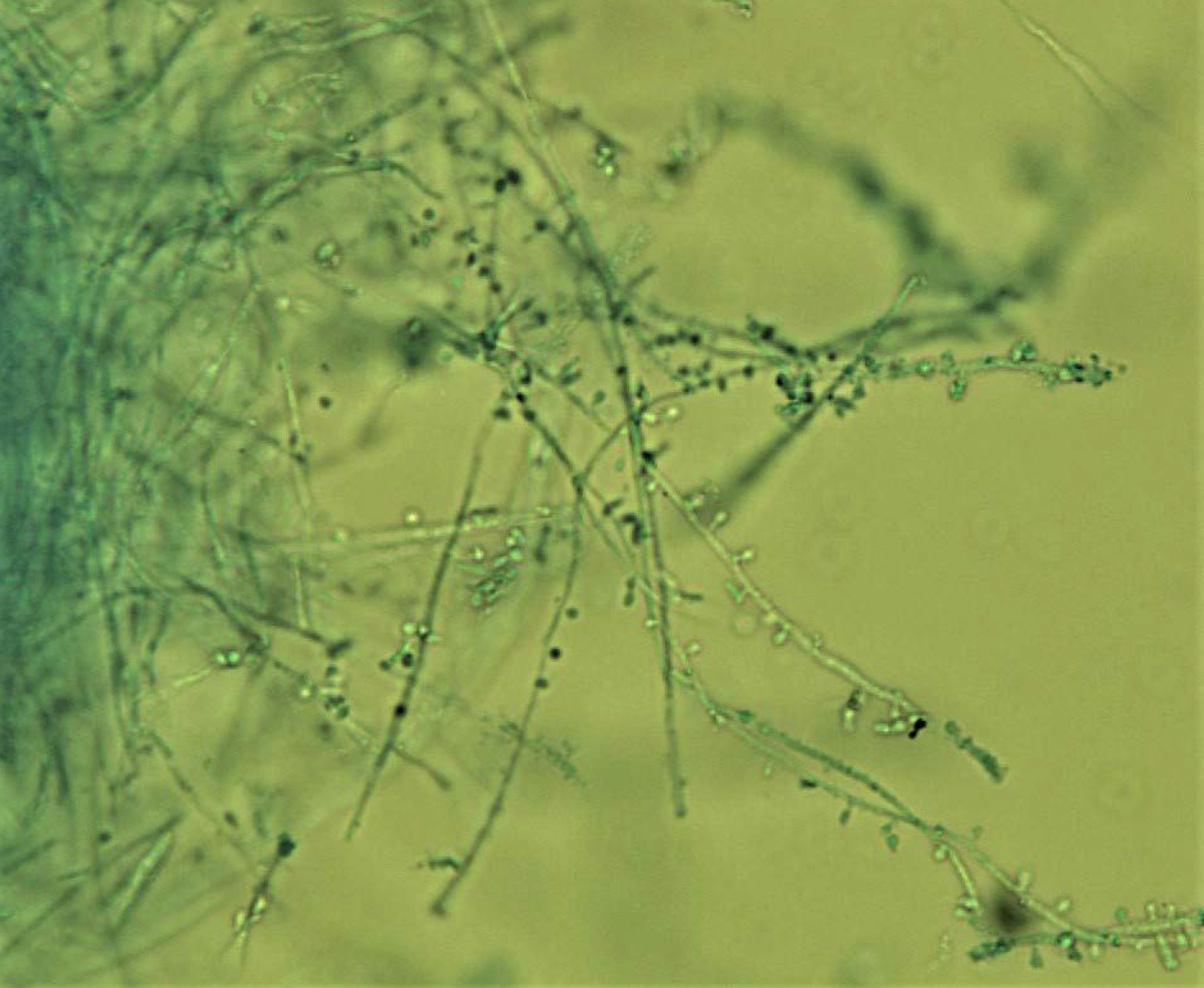
- LPCB mount showing growth of Trichophyton rubrum (Fine septate hyaline hyphae with alternately arranged tear drop-shaped microconidia)
Discussion
Onychomycosis (OM) constitutes the most common nail infection (40–50% of onychopathies). In our study, 300 diabetic patients were screened and 102 of these fulfilled the diagnostic criteria for OM, which translates to a prevalence of 34%. There is only one similar study from North India conducted in 2002 that reported a prevalence of 17% among 400 diabetics as compared to 6.8% in the control group. 5
Globally, a multicentric study from Canada and USA, (1998) reported the prevalence of OM to be 26% in 550 diabetic patients. 8 On the contrary, a study from Cameroon (2016), reported a much higher prevalence of OM (50.7%). Among diabetics 9 in studies from Turkey 10 and Denmark, 11 the prevalence of OM in diabetic patients has been reported to be 34.9% and 22%, respectively. Hence, the prevalence has been very variable probably depending on the geographical locations, timeline and diagnostic criteria used for OM.
The risk of OM is 2.25 times higher in males as compared to females which may be attributed to the trend of wearing occlusive shoes and potential trauma during outdoor sports. This higher male prevalence has also been reported by Dogra et al. 5 (1.4:1), Gupta et al. 8 (M: F = 2.06:1), Yadav et al. 12 (7.4:1) and Garg et al. 13 (2.7:1). Patients with age > 60 years were three times at a higher risk than younger population (<40 years). Factors like multiple co-morbidities, intake of various medications, increased susceptibility to infections, poor foot care, and reduced health care-seeking behaviour may be contributory in old-age patients.
The BMI was found to be a significant risk factor for OM in our study; possibly because patients with a higher BMI are more prone to have a sedentary lifestyle. However, BMI as a risk factor has not been reported in other studies.
A statistically significant correlation (P = 0.014, r = 0.14) was found between the severity of nail involvement (number of nails involved) and the glycemic control (HbA1c levels). This is the first study correlating the severity of nail involvement with HbA1c.
In our study, a combination of diagnostic tests for OM showed an enhanced positivity as compared to the individual one. Very few studies have used histopathology with PAS and onychoscopy as modalities for the diagnosis of OM in diabetic patients. A combination of DME and onychoscopy was positive in all but one patient (99%), followed by DME and histopathology (97%). Although histopathology is expensive and time-consuming, its sensitivity has been reported to be more than DME with KOH and culture in various studies. 14 , 15
Limitations
As cases were recruited from a hospital setting, there could be chances of Berksonian bias. Hence, community screening may be advisable in diabetic patients for the early detection of OM.
Conclusion
The prevalence of OM is high in patients with diabetes, especially in males. It can be diagnosed with higher certainty using a combination of investigations. Onychomycosis tends to be more severe in patients with poor glycemic control. It is important to diagnose OM early in order to treat and prevent potential complications.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Onychomycosis of toenails: Orthopaedic and podiatric considerations. Australas J Dermatol. 2002;43:105-12.
- [CrossRef] [PubMed] [Google Scholar]
- The nondermatophyte molds: Emerging as leading cause of onychomycosis in south-east Rajasthan. Indian Dermatol Online J. 2015;6:92-7.
- [CrossRef] [PubMed] [Google Scholar]
- Toenail onychomycosis in diabetic patients: Issues and management. Am J Clin Dermatol. 2009;10:211-20.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetes and impaired glucose tolerance. In: Gan D, ed. Diabetes atlas. International Diabetes Federation (5th ed). Belgium: International Diabetes Federation; 2011. p. :15-103.
- [Google Scholar]
- Epidemiology of onychomycosis in patients with diabetes mellitus in India. Int J Dermatol. 2002;41:647-51.
- [CrossRef] [PubMed] [Google Scholar]
- Nail dermoscopy (onychoscopy) findings in the diagnosis of primary onychomycosis: A cross-sectional study. Indian J Dermatol Venereol Leprol. 2020;86:341-349.
- [CrossRef] [PubMed] [Google Scholar]
- Dendritic pattern: Unique onychoscopic feature in endonyx. J Am Acad Dermatol. 2019;81:e89-90.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and epidemiology of toenail onychomycosis in diabetic subjects: A multicentre survey. Br J Dermatol. 1998;139:665-71.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomycosis in diabetic patients in Fako Division of Cameroon: Prevalence, causative agents, associated factors and antifungal sensitivity patterns. BMC Res Notes. 2016;9:494.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of tinea pedis and onychomycosis frequency in diabetes mellitus patients with diabetes complications and foot ulcers. A cross sectional – observational study. Pakistan J Med Sci. 1969;32:891-5.
- [Google Scholar]
- Prevalence of toe nail onychomycosis in diabetic patients. Acta Derm Venereol. 2006;86:425-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinico-mycological study of dermatophyte toenail onychomycosis in New Delhi, India. Indian J Dermatol. 2015;60:153-8.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomycosis in central India: A clinicoetiologic correlation. Int J Dermatol. 2004;43:498-502.
- [CrossRef] [PubMed] [Google Scholar]
- Histopathological examination of nail clippings using PAS staining (HPE-PAS): Gold standard in diagnosis of Onychomycosis. Mycoses. 2015;58:27-32.
- [CrossRef] [PubMed] [Google Scholar]
- New reasons for histopathological nail-clipping examination in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol. 2011;25:235-7.
- [CrossRef] [PubMed] [Google Scholar]







