Translate this page into:
Primary cutaneous diffuse large B cell lymphoma, leg type
2 Department of Pathology, MGIMS, Sewagram, Maharastra, India
3 Department of Surgery, MGIMS, Sewagram, Maharastra, India
Correspondence Address:
Atul Dongre
Department of Dermatology, MGIMS, Sewagram - 442 102, Maharastra
India
| How to cite this article: Dongre A, Kar S, Gondse S, Gangane N, Mehra BK. Primary cutaneous diffuse large B cell lymphoma, leg type. Indian J Dermatol Venereol Leprol 2011;77:212-214 |
Sir,
Primary cutaneous diffuse large B-cell lymphoma, leg type, is a non-Hodgkin lymphoma of intermediate behavior. [1] The estimated 5-year survival according to World Health Organization-European Organization for Research and Treatment of Cancer (WHO-EORTC) classification is about 55%. [2]th
A 78-year-old male presented with asymptomatic, slowly enlarging nodular lesion since 1 year on the left forearm. He had no history of night sweat, fever or weight loss. Clinical examination revealed a large, erythematous, shiny, non-tender, soft to firm nodule of approximate size 6 cm Χ 5 cm on the anterio-lateral aspect of the left forearm [Figure - 1]. A few satellite papules were noted in the vicinity of the nodule. There was no significant lymphadenopathy. His systemic examination and routine hemogram was normal. Enzyme-linked immunosorbent assay (ELISA) test for HIV was non-reactive.
 |
| Figure 1: Large, lobulated, shiny erythematous nodule with few satellite lesions on the forearm |
Punch biopsy taken from the papules showed dense, diffuse infiltration of abnormal large cells occupying the entire dermis with extension to subcutaneous tissue [Figure - 2]. The infiltrate was mixed in nature with predominance of centroblasts and immunoblasts [Figure - 3]. Immunohistochemical markers were positive for CD20 [Figure - 4], CD79a, Bcl-2, and negative for Bcl-6. There was no systemic involvement on ultrasonography and computerized tomography (CT) scan. Bone marrow studies revealed no abnormality. Thus, as there was no systemic involvement, a diagnosis of primary cutaneous diffuse large B-cell lymphoma (PCLBCL), leg type, was confirmed. As the lesions were few in number, a surgical excision was done. After a period of 7 months, he presented with similar kind of new lesion involving the face, left knee [Figure - 5] and lateral part of left elbow. Once again, he was thoroughly investigated for extracutaneous involvement but it did not reveal anything.
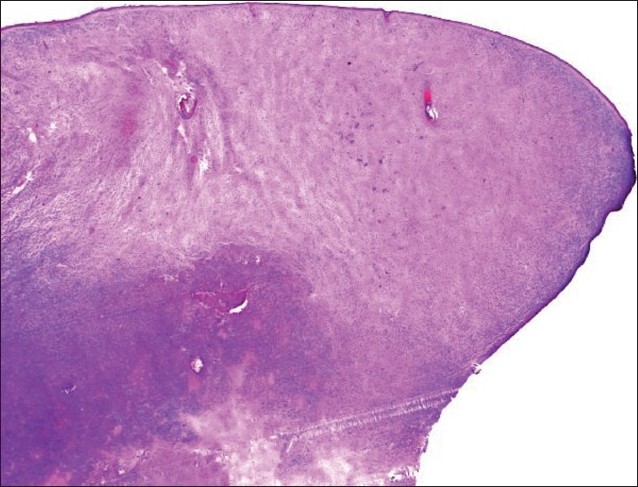 |
| Figure 2: Dense and diffuse infiltrate in the entire dermis along with extension to subcutaneous tissue (H and E, �25) |
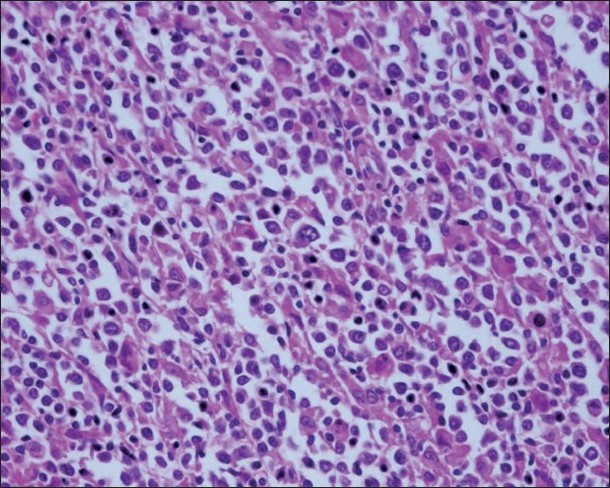 |
| Figure 3: Mixed cellular infiltrate with predominance of blast cells (H and E, ×400) |
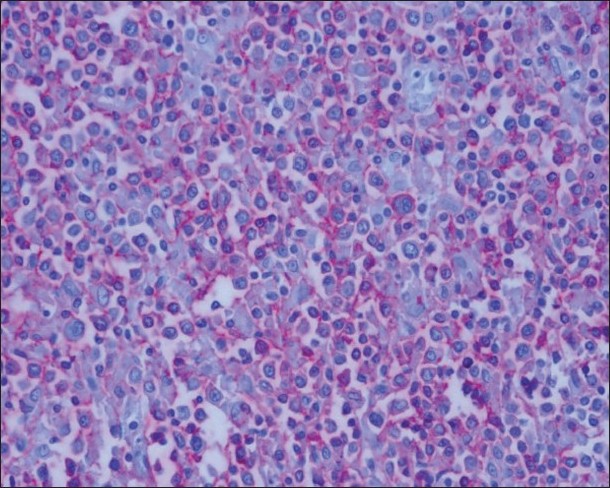 |
| Figure 4: Positive staining for CD20 (a B-cell marker) |
 |
| Figure 5: New lesion on right leg |
Considering the recurrence and multiple lesions, CHOP regimen consisting of cyclophosphamide, hydroxydaunorubicin, oncovin and prednisolone was started of which results are awaited.
Primary cutaneous B-cell lymphomas are now considered as a distinctive entity with overall better prognosis. Earlier, large B-cell lymphoma, leg type, was amidst classification controversies. In EORTC classification, it was designated as primary cutaneous large B-cell lymphoma, leg type, while WHO classified it as diffuse large B-cell lymphoma. The current WHO-EORTC consensus classification (2005) considers two different types of PCLBCL, viz., PCLBCL, leg type, and PCLBCL others. [2] In recent few years, association between hepatitis C virus infection and non-Hodgkin′s diffuse large B-cell lymphoma has been documented by many studies. Viguier et al. have documented such association in primary cutaneous lymphoma. [3] Also, an association between Borrelia burgdorferi infection and various types of cutaneous B-cell lymphomas is noted in some studies. One case report mentions clinical remission following antibiotic therapy for Borrelia in a case of multilesional primary cutaneous large B-cell lymphoma.
PCLBCL, leg type, characteristically occurs in elderly above 70 years of age as erythematous or brown-colored plaques or nodules on legs with female preponderance. However, there are a few reports mentioning its occurrence also in males. [4] Though in approximately 60-70% of cases it occurs on leg, cutaneous involvement other than leg, affecting face, trunk, neck and extremities has been reported. [4] Rarely, it may mimic chronic venous ulcer on leg. In our case, lesion first appeared on the forearm, and when recurrence occurred, leg was affected. Extracutaneous involvement after a few years of the onset of disease can occur. A case involving CNS has been reported.
Microscopically, PCLBCL shows diffuse infiltrate with predominance of centroblasts and immunoblasts. B-cell markers like CD20 and CD79a are expressed by neoplastic cells. Bcl-2 protein is positive in almost all the cases. [5] Some tumors may be positive for Bcl-6. Primary cutaneous follicular center cell lymphoma (PCFCL) with diffuse growth pattern may mimic PCLBCL. Characteristically, PCFCLs do not express Bcl-2 protein or show faint Bcl-2 staining in a minority of tumor cells and unlike PCFCL, most PCLBCL, leg types, express MUM-1/IRF4 protein.
Solitary or grouped lesions can be managed with radiotherapy followed by surgical excision. For multiple widespread lesions, systemic chemotherapy is required. Rituximab (an anti-CD20 antibody), with or without combination with CHOP regimen, has been successfully used for treatment. [6] Liposomal anthracycline is also effective. A single case report has documented usefulness of intralesional interferon alpha 2 in a patient.
EORTC classification considers PCLBCL, leg types, as intermediate prognosis. Compared to other primary cutaneous B-cell lymphomas like marginal zone or follicular center cell, the prognosis of PCLBCL, leg types, is worse. Relapse after treatment and spread to extracutaneous sites are known to occur and are common.
Acknowledgement
We are grateful to Dr. Almut Boer, Dermatologicum, Hamburg, Germany, for her expertise help in histopathological and immunohistochemical analysis of the biopsy specimens.
| 1. |
Vermeer MH, Geelen FA, van Haselen CW, van Voorst Vader PC, Geerts ML, van Vloten WA, et al. Primary cutaneous large B-cell lymphomas of the legs: A distinct type of cutaneous B-cell lymphoma with an intermediate prognosis. Arch Dermatol 1996;132:1304-8.
[Google Scholar]
|
| 2. |
Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-85.
[Google Scholar]
|
| 3. |
Viguier M, Rivet J, Agbalika F, Kerviler E, Brice P, Dubertret L, et al. B-cell lymphomas involving the skin associated with hepatitis C virus infection. Int J Dermatol 2002;41:577-82.
[Google Scholar]
|
| 4. |
Belousova IE, Vanecek T, Skreg SV, Rodionov AN, Samtsov AV, Kazakov DV. Unusual clinicopathological presentation of primary cutaneous diffuse large B-cell lymphoma, leg type, with multiple nodules and widespread garland-like lesions. Am J Dermatopathol 2009;31:370-4.
[Google Scholar]
|
| 5. |
Hoefnagel JJ, Vermeer MH, Jansen PM, Fleuren GJ, Meijer CJ, Willemze R. Bcl-2, Bcl-6 and CD10 expression in cutaneous B-cell lymphoma: further support for a follicle centre cell origin and differential diagnostic significance. Br J Dermatol 2003;149:1183-91.
[Google Scholar]
|
| 6. |
Guyot A, Ortonne N, Valeyrie-Allanore L, Bagot M. Combined treatment with rituximab and anthracycline-containing chemotherapy for primary cutaneous large B-cell lymphomas, leg type, in elderly patients. Arch Dermatol 2010;146:89-91.
[Google Scholar]
|
Fulltext Views
3,323
PDF downloads
1,668





