Translate this page into:
Primary localized cutaneous nodular amyloidosis on areola
Corresponding author: Dr. Wei-Ming Wang, Department of Dermatology, Tri-Service General Hospital, National Defense Medical Center, Taipei City, Taiwan. ades0431@ms38.hinet.net
-
Received: ,
Accepted: ,
How to cite this article: Liu S, Hung C, Gao H, Chiang C, Chen C, Chen Y. Primary localized cutaneous nodular amyloidosis on areola. Indian J Dermatol Venereol Leprol 2022;88:653-5.
Sir,
Primary localized cutaneous nodular amyloidosis is a rare disorder in which amyloid light-chain deposits within the skin without any systemic involvement. Primary localized cutaneous nodular amyloidosis most commonly affects the acral region, followed by the face and trunk. We herein report a unique case of primary localized cutaneous nodular amyloidosis, located on the nipple-areolar complex.
A 57-year-old female presented with an asymptomatic enlarging skin lesion on her left breast which was noticed two months back. She also gave history of fibrocystic change of bilateral breasts for 10 years. On physical examination, the skin lesion appeared as a well-demarcated, reddish-orange, polygonal, waxy plaque on her left areola with a similar but smaller plaque at the centre of the left nipple [Figure 1a]. Polarized contact dermoscopy showed several yellowish-orange globules on a milky-red background, with some arborizing vessels at the periphery [Figure 1b]. An incisional biopsy was performed. Histopathology revealed abundant deposition of pale eosinophilic amorphous material separated by clefts and accompanied by a sparse lymphoplasmacytic infiltrate in the upper dermis [Figure 2a]. The deposited material showed positive staining with Congo-red stain and showed apple-green birefringence on polarized microscopy [Figure 2b]. It was also stained with Thioflavin S and showed immunoreactivity to kappa and lambda light chains.

- Well-demarcated, reddish orange, polygonal, flat and waxy plaques on left areola and the center of nipple
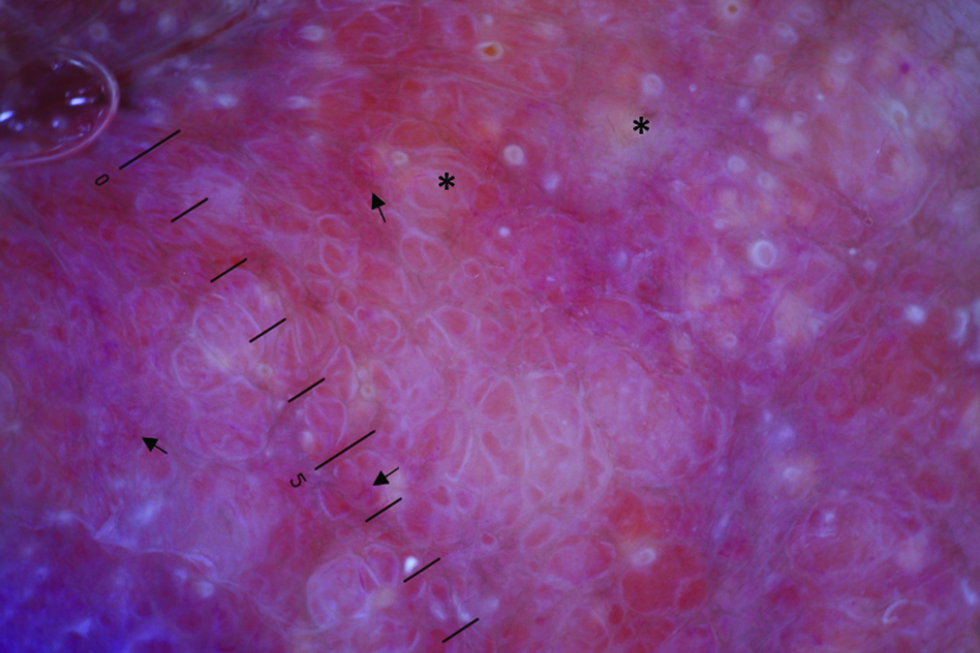
- Dermatoscopy showed several yellowish-orange globules (asterisks) on a milky-red background with some arborizing vessels (arrows) at the periphery (Non-polarized Heine Delta 20 dermatoscope; original magnification: x 10)
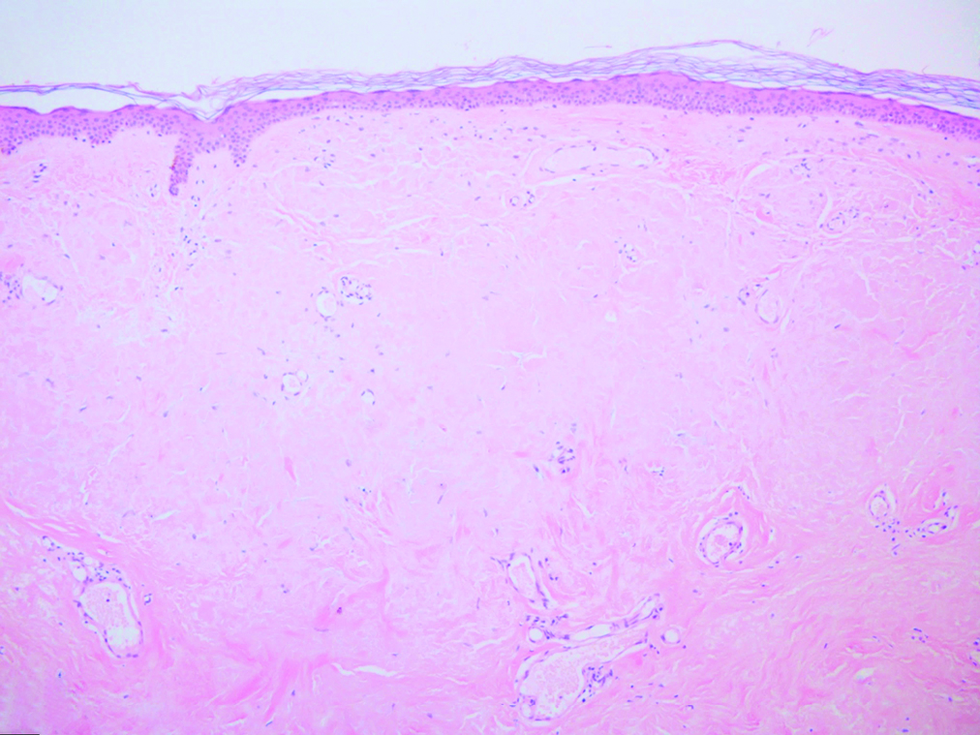
- Abundant deposition of pale eosinophilic amorphous material separated by clefts in the upper dermis (H&E; original magnification: x 100)
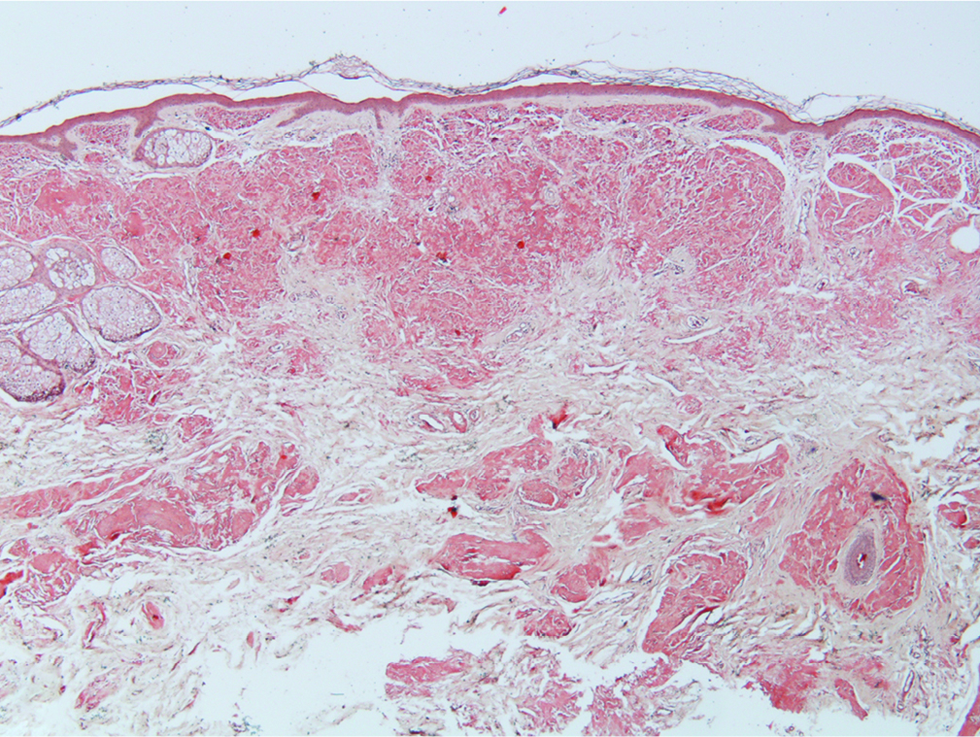
- The deposited material stained positively with Congo-red (Congo-red stain; original magnification: x 40)
A series of examinations to survey systemic involvement of amyloid light-chain amyloidosis was conducted, including a complete blood cell count with differential count, serum and urine protein electrophoresis, serum immunoglobulins and free light chains levels, which were all within normal limits. Serum creatinine was 0.5 mg/dL and alanine transaminase was 16 U/L. Electrocardiography showed sinus rhythm without abnormal findings.
Based on the histopathologic findings and laboratory studies, the diagnosis of primary localized cutaneous nodular amyloidosis was confirmed. Surgical removal of the tumour was done and no recurrence was noticed during 1-year follow-up.
Primary localized cutaneous nodular amyloidosis, the rarest subtype of cutaneous amyloidosis, is characterised clinically by solitary or multiple waxy yellowish nodules or plaques. Most of the cases of primary localized cutaneous nodular amyloidosis were found over extremities. We found only two previous reports of breast amyloidosis in the literature.1,2 However, the lesions in those cases were located in the subcutaneous tissue of the breast and were detected by the patient or imaging studies. In contrast, our case is a visible skin lesion on the nipple and areola. Dermoscopy which reveals orange-yellowish areas in cutaneous nodular amyloidosis,3 may aid dermatologists in the initial differential diagnosis.
Primary localized cutaneous nodular amyloidosis is caused by dermal deposition of amyloid fibrils derived from immunoglobulin light-chain, which is produced by local monoclonally-expanded plasma cells in the skin. Primary localized cutaneous nodular amyloidosis is clinically and histologically indistinguishable from cutaneous lesions of primary systemic amyloidosis, which is also composed of light-chain amyloid protein. The risk of progression of primary localized cutaneous nodular amyloidosis to systemic amyloidosis could hardly be estimated due to the rarity of primary localized cutaneous nodular amyloidosis, but was reported within the range of 7–50% in some case series.4 Therefore, it is crucial to perform systemic evaluation and long-term follow-up for patients with primary localized cutaneous nodular amyloidosis.
Various treatment modalities have been proposed, including surgical excision, dermabrasion, laser therapy, electrodesiccation and curettage, intralesional steroid injection and cryosurgery.
In conclusion, we report a case of primary localized cutaneous amyloidosis with a unique location and also highlight the importance of using dermoscopy in guiding clinical suspicion of amyloidosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Amyloidosis of the breast: Predominantly AL type and over half have concurrent breast hematologic disorders. Mod Pathol. 2013;26:232-8.
- [CrossRef] [PubMed] [Google Scholar]
- Localized primary breast amyloidosis and 1-year changes in imaging: A case report. Radiol Case Rep. 2020;15:2637-2640.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A unique dermoscopy pattern of primary cutaneous nodular amyloidosis mimicking a granulomatous disease. J Am Acad Dermatol. 2016;74:e9-e10.
- [CrossRef] [PubMed] [Google Scholar]
- Nodular localized primary cutaneous amyloidosis: A long-term follow-up study. Br J Dermatol. 2001;145:105-9.
- [CrossRef] [PubMed] [Google Scholar]





