Translate this page into:
Profile of HIV serodiscordant couples in a tertiary care center
Correspondence Address:
Srihari Sahana
No 26, 3rd Main, NR Colony, Bengaluru - 560 019, Karnataka
India
| How to cite this article: Sahana S, Betkerur J. Profile of HIV serodiscordant couples in a tertiary care center. Indian J Dermatol Venereol Leprol 2019;85:347 |
Abstract
Background: Globally, 36.7 million people are infected with Human Immunodeficiency Virus (HIV). Of these 36.7 million people, 2.1 million are in India. Integrated counseling and testing centers are the cornerstones of early access to prevention and support services. The term “serodiscordant couple” refers to a couple where one partner is HIV-positive and the other HIV-negative.
Aim: To study the serodiscordance rates in a cohort of people attending integrated counseling and testing center.
Materials and Methods: Aretrospective descriptive study of data from integrated counseling and testing center from January 2013 to December 2014 was done.
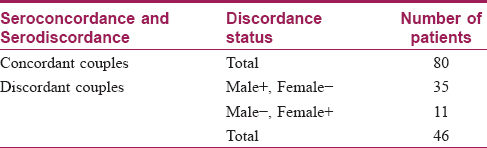
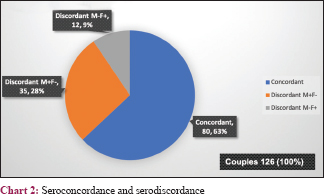
Results: Of the 7489 persons tested, 306 persons were positive for HIV (192 males and 114 females) with a prevalence of 4 percent. Of the 126 couples tested, serodiscordance was found in 46 couples, while 80 couples were seroconcordant. The overall prevalence of HIV serodiscordance was 36.5 percent. Male positive and female negative couples (M+ F−) were 35 (76.0%) and female positive and male negative (F+ M−) were 11 (23.9%). Discordant M+ F− couples were significantly higher than discordant F+ M− couples (P < 0.001). Most participants were aged between 21 and 40 years. The average age of men was 41.91 years and that of women was 34.21 years. The average age difference between life partners was 7.7 years. Significant association was seen between age and gender, as females were found to be younger (P value = 0.001).
Limitation: Information regarding years of married life, number of sex partners or sexual behavior pre- and post-detection were not collected. Thus, our data present only the magnitude of serodiscordance in a cohort but does not analyze the other predictors of serodiscordance.
Conclusion: Serodiscordant relationships occur more commonly in India than is presumed. Our study highlights the profile of serodiscordant couples in this part of the country. Effective measures to prevent transmission of HIV within a serodiscordant relationship are necessary steps in halting the HIV epidemic.
Introduction
A chronic disorder can become a powerful third member in any dyadic family relationship. Presently, there are 36.7 million people globally living with HIV. New HIV infections have fallen by 6% since 2010. In 2011, the estimated number of people living with HIV/acquired immune deficiency syndrome in India was 2.1 million. The prevalence of HIV in adults at the national level has continued its steady decline from an estimated peak of 0.38% in 2001–2003 to 0.34% in 2007 and 0.28% in 2012 to 0.26% in 2015.[1] Prevention strategies under the National AIDS Control Program were instrumental in reducing the annual new HIV infections among the adult population from 2.74 lakhs in 2006 to 1.16 lakhs in 2011, an overall reduction of around 57 percent.[2] The term “serodiscordant couple” refers to a couple where one partner is HIV-positive and the other HIV-negative. In couples where one person is living with HIV and the other is HIV-negative, the HIV-negative partner is at continuous risk for infection.[3] It has been observed in some studies in Africa that the prevalence of HIV serodiscordance in couples is high, being more than 60% among married/cohabiting couples.[4] Heterosexual contact is responsible for 87.4% of all HIV transmissions in India.[5] The risk of HIV transmission between HIV serodiscordant couples is highly variable and reflects an interplay between biological, genetic and immunological factors along with various sociobehavioral factors.[5] This risk is higher where antiretroviral therapy is not universally available.[6],[7],[8],[9] In mature epidemics, there is evidence to show that HIV serodiscordant couples contribute significantly to new HIV transmission.[8],[9],[10],[11],[12] Early access to diagnosis, employing prevention strategies and providing support services through integrated counseling and testing centers are all key measures required to halt this epidemic.
Aims and objectives
The aim of this project was to study the discordance rates in a cohort of people attending integrated counseling and testing center at JSS Hospital, Mysuru, Karnataka, India.
Methods
In this retrospective study, we included all people tested for HIV in integrated counseling and testing center of JSS Hospital, Mysuru, from January 2013 to December 2014. Demographic details and history of marital status, serostatus of the couple, death of or separation from spouse if any (with reason) were all documented. The partner reporting first was considered as the index case. The cases were antiretroviral therapy naïve at the time of enrolment. The partner was counseled for examination and assessment of HIV status. Patients whose complete details were not available were contacted and the details were recorded. The spouses and children of these cases were tested to determine their HIV status.
Statistical methods
The collected data were entered into a Microsoft Excel spreadsheet. Identifying information was not recorded. Data was analyzed using SPSS software (version 16). Cramer's test was applied to find out the association between rows and columns of tabulated results of the study. Quantitative data was statistically presented using mean and standard deviation. A value of P ≤ 0.05 was considered statistically significant.
Observations
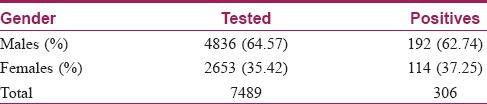
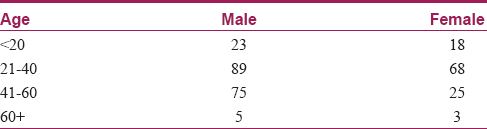
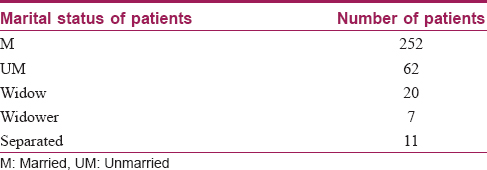
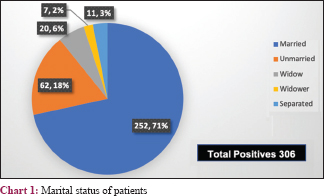
A total of 7489 cases were tested with 306 cases being positive. Of them, 192 were males and 114 were females with a prevalence of 4.0% [Table - 1]. Most participants were aged between 21 and 40 years. Average age for men was 41.91 and women 34.21 years. The average age difference between partners was 7.7 years [Table - 2]. There were 126 couples, all of whom were living together. Of these, 46 were serodiscordant and 80 seroconcordant, with a total of 206 testing positive. There were another 100 positives, of whom 27 were widowed (20 widows and 7 widowers) and 11 separated; all were seroconcordant with their spouses who died due to HIV (P < 0.001) [Table - 3] and [Chart 1]. The remaining 62 were unmarried. The overall prevalence of HIV serodiscordance was 30.0 percent. M+ F− was 35 (76.0%) and F+ M− was 11 (23.9%) [Table - 4] and [Chart 2]. Younger women were more significantly affected (P value = 0.001). Discordant M+ F− couples were significantly more in number than discordant F+ M− couples (P < 0.001). The children of the 126 couples were tested and 37 were found to be HIV positive.
Discussion
Acquired immune deficiency syndrome has been a health problem of great importance. Being known since long and having no complete cure makes it even more challenging.[13] India has about 2.1 million people living with HIV. Heterosexual contact (87.4%) is the major route of transmission.[5] In a study by Kilembe et al., the highest prevalence was among participants who were between 25 and 34 years of age.[14] Most of our participants were aged between 21 and 40 years (P < 0.001.). However, the average age for men was 41.91 and that for women was 34.21 years. The average age difference between partners was 7.7 years. Data from National AIDS Control Organization (NACO) suggest feminization of the HIV epidemic in India with 39% of cases in females.[1] In our study, 114 (37.2%) females and 192 (62.7%) males were seropositive. Significant association was seen between age and gender as females were found to be younger (P < 0.001). A serodiscordant couple is a couple in which one partner is HIV-positive, whereas the other is HIV-negative. There is a high serodiscordance rate among married couples, and it is higher among men than among women.[3] The overall prevalence of HIV sero-discordance was 30.0 percent. In a study by Kairania et al., out of 337 couples tested, 293 were HIV-discordant, among whom 192 (65.5%) male partners and 101 (34.5%) female partners were HIV-infected.[15] This is consistent with observations in our study. The male/female difference (76.0 vs 23.9%), was significant (P < 0.001). The HIV-negative partner is neither “immunized” nor protected against HIV infection. He/she is always at a risk of getting infected with HIV in future.[13] Various socio-behavioral factors along with biological, genetic and immunological factors play a role in the risk of HIV transmission between HIV serodiscordant couples. HIV transmission among discordant couples ranges from 5.0 to 16.7 per 100 person - years, which is 5–17 times higher than the incidence among HIV negative couples.[15] The annual risk of transmission of HIV from an infected partner to an uninfected partner in a serodiscordant state is around 20–25 percent.[16] In our study only one female who was negative in a discordant relationship before counseling became positive during the follow-up and in a 10-year period only two discordant couples had become concordant. In a hitherto seroconcordant couple, the male partner is more likely to be the index case in most cases and infect his female partner.[3] This idea is supported by the higher number of widows (20) compared with widowers in our study, given that all were seroconcordant with their spouses.
Avoiding transmission to the seronegative partner is of paramount importance in case of serodiscordant couples. The high number of female spouses at risk of exposure emphasizes the need for continued and increased measures to prevent transmission such as information, education and communication programs to prevent HIV transmission among couples.[3]
Various programs such as voluntary counseling and testing, condom promotion and risk reduction counseling, needle exchange programs, opiate substitution therapy, male circumcision, immediate antiretroviral therapy irrespective of CD4 count, pre-exposure prophylaxis and vaginal microbicides can reduce the risk to 3–7 percent.[17] Less than 10% of HIV seropositive individuals know their partners status and only about 20% of HIV discordant couples know that they are living in a discordant relationship.[15] The HIV-positive partner should receive care and treatment services for his or her own health and to reduce the risk of transmission to the HIV-negative partner. Serodiscordant couples who are aware of each other's HIV status will be able to adhere to safe sexual practices, treatment and prevention of mother-to-child transmission interventions and give each other emotional support. By consistently practicing safer sex such as using male and female condoms, it is possible for couples to stay serodiscordant indefinitely.[18]
In our study, 37 children were found to be HIV-positive. Seropositive couples try to conceive even after knowing their status because of societal pressure. HIV-positive females with discordant partners face even greater problems as they have to take care of themselves, conceive, enter prevention of mother-to-child transmission programs, take care of the positive child and also bear the social stigmata.
Conclusion
Serodiscordant relationships occur more commonly than presumed. Our study highlights the profile of serodiscordant couples in a cohort in southern India. The high prevalence of sero-discordance emphasizes the importance of couple/partner testing. Effective measures to prevent transmission to the HIV negative partner will help in halting the HIV epidemic. Information, education and communication programs, promoting condoms use, early antiretroviral therapy to HIV-positive partner and pre-exposure prophylaxis will reduce transmission. Long-term follow-up of couples is required to assess the effectiveness of this strategy.
Limitation
Information regarding years of married life, number of sex partners or sexual behavior pre- and post-detection were not collected. Thus, our data present only the magnitude of serodiscordance in a cohort but does not analyze the other predictors of serodiscordance.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
National Institute of Medical Statistics. India HIV Estimations 2015, Technical Report. National AIDS Control Organisation. Indian Council of Medical Research (Department of Health Research). Ministry of Health & Family Welfare, Government of India; 2015.
[Google Scholar]
|
| 2. |
Department of AIDS Control, National AIDS Control Organization. Annual Report 2013-14. Ministry of Health & Family Welfare, Government of India. [Last accessed on 2015 Aug 27]. aidsdatahub.org.
[Google Scholar]
|
| 3. |
Van Tam V, Cuong DD, Alfven T, Phuc HD, Chuc NT, Hoa NP, et al. HIV sero-discordance among married HIV patients initiating anti-retroviral therapy in northern Vietnam. AIDS Res Ther 2016;13:39.
[Google Scholar]
|
| 4. |
Ngilangwa DP, Ochako R, Mboya BA, Noronha RH, Mgomella GS. Prevalence and predictors of HIV sero-discordance among cohabiting couples tested in Northern Tanzania. Pan Afr Med J 2015;22:275.
[Google Scholar]
|
| 5. |
Marfatia YS, Naik E, Singhal P, Naswa S. Profile of HIV seroconcordant/discordant couples a clinic based study at Vadodara, India. Indian J Sex Transm Dis AIDS 2013;34:5-9.
[Google Scholar]
|
| 6. |
Mujugira A, Baeten JM, Donnell D, Ndase P, Mugo NR, Barnes L, et al. Characteristics of HIV-1 serodiscordant couples enrolled in a clinical trial of antiretroviral pre-exposure prophylaxis for HIV-1 prevention. PLoS One 2011;6:e25828.
[Google Scholar]
|
| 7. |
Carpenter LM, Kamali A, Ruberantwari A, Malamba SS, Whitworth JA. Rates of HIV-1 transmission within marriage in rural Uganda in relation to the HIV sero-status of the partners. AIDS 1999;13:1083-9.
[Google Scholar]
|
| 8. |
Parikh SA. The political economy of marriage and HIV: The ABC approach, “safe” infidelity, and managing moral risk in Uganda. Am J Public Health 2007;97:1198-208.
[Google Scholar]
|
| 9. |
Guthrie BL, de Bruyn G, Farquhar C. HIV-1-discordant couples in sub-Saharan Africa: Explanations and implications for high rates of discordancy. Curr HIV Res 2007;5:416-29.
[Google Scholar]
|
| 10. |
Kaiser R, Bunnell R, Hightower A, Kim AA, Cherutich P, Mwangi M, et al. Factors associated with HIV infection in married or cohabitating couples in Kenya: Results from a nationally representative study. PLoS One 2011;6:e17842.
[Google Scholar]
|
| 11. |
Rispel LC, Cloete A, Metcalf CA, Moody K, Caswell G. 'It [HIV] is part of the relationship': Exploring communication among HIV-serodiscordant couples in South Africa and Tanzania. Cult Health Sex 2012;14:257-68.
[Google Scholar]
|
| 12. |
King R, Wamai N, Khana K, Johansson E, Lindkvist P, Bunnell R. “Maybe his blood is still strong”: A qualitative study among HIV-sero-discordant couples on ART in rural Uganda. BMC Public Health 2012;12:801.
[Google Scholar]
|
| 13. |
de Amorim CM, Szapiro AM. Analysing the risk problem in couples living in serodiscordance situation. Sci Public Health 2008;13:1859-68.
[Google Scholar]
|
| 14. |
Kilembe W, Wall KM, Mokgoro M, Mwaanga A, Dissen E, Kamusoko M, et al. Implementation of couples' voluntary HIV counseling and testing services in Durban, South Africa. BMC Public Health 2015;15:601.
[Google Scholar]
|
| 15. |
Kairania R, Gray RH, Kiwanuka N, Makumbi F, Sewankambo NK, Serwadda D, et al. Disclosure of HIV results among discordant couples in Rakai, Uganda: A facilitated couple counselling approach. AIDS Care 2010;22:1041-51.
[Google Scholar]
|
| 16. |
Recommendations for a Public Health Approach. Guidance on Couples HIV Testing and Counselling Including Antiretroviral Therapy for Treatment and Prevention in Sero-Discordant Couples. World Health Organization; April, 2012. Geneva, Switzerland. [Last accessed on 2015 Aug 27]. http://www.who.int/hiv/pub/guidelines/9789241501972/en.
[Google Scholar]
|
| 17. |
Solomon SS, Solomon S. HIV serodiscordant relationships in India: Translating science to practice. Indian J Med Res 2011;134:904-11.
[Google Scholar]
|
| 18. |
Bunnell RE, Nassozi J, Marum E, Mubangizi J, Malamba S, Dillon B, et al. Living with discordance: Knowledge, challenges, and prevention strategies of HIV-discordant couples in Uganda. AIDS Care 2005;17:999-1012.
[Google Scholar]
|
Fulltext Views
2,324
PDF downloads
1,193





