Translate this page into:
Progressive cribriform and zosteriform hyperpigmentation
Correspondence Address:
Anupam Das
Building - "PRERANA" 19, Phoolbagan, Kolkata - 700 086, West Bengal
India
| How to cite this article: Das A, Bandyopadhyay D, Mishra V, Gharami RC. Progressive cribriform and zosteriform hyperpigmentation. Indian J Dermatol Venereol Leprol 2015;81:321-323 |
Sir,
Progressive cribriform and zosteriform hyperpigmentation (PCZH) refers to an asymptomatic dermatosis characterized by pigmented macules arranged in whorls and streaks in a Blaschkoid pattern.
An otherwise healthy 14-year-old girl presented to the dermatology outpatient department of Medical College and Hospital, Kolkata with a two-year history of asymptomatic dark patches confined to the right half of her torso. Brownish macules with a cribriform configuration extended linearly from the right flank to the front of the abdomen reaching the pubic area. Similar lesions were also present over the supero-lateral quadrant of her right breast. There were slight depressions at places [Figure - 1]a and b. Examination of her hair, nails, and mucosae did not reveal any abnormality. The lesions had first appeared over the flank, 2 years earlier, and had gradually progressed in linear fashion to their present extent. There was no history of trauma, inflammation, or use of any topical application on the involved areas prior to development of the lesions. Past medical history and family history were non-contributory. Our clinical differential diagnoses included lichen planus pigmentosus, verrucous epidermal nevus, reticulate pigmentary disorder, and linear and whorled nevoid hypermelanosis.
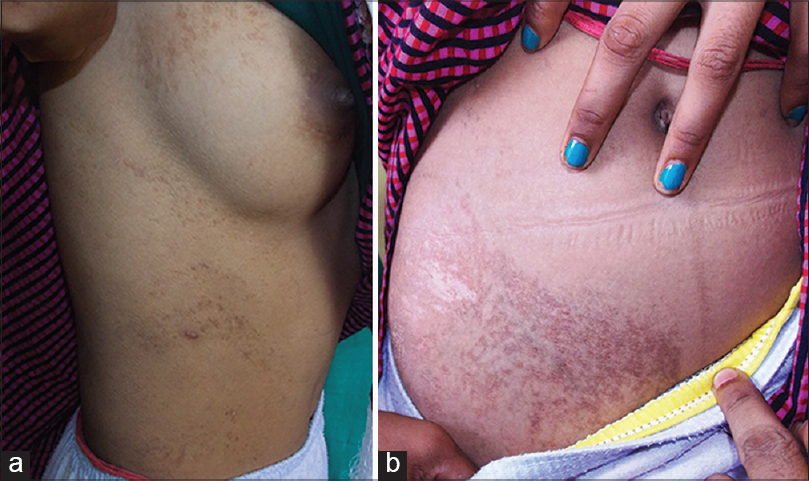 |
| Figure 1: (a) Cribriform linear brownish pigmentation extending from flank to front of abdomen. Note lesions over breast. (b) The lesions reaching the pubic area |
A skin biopsy from a representative abdominal lesion revealed elongated epidermal rete ridges with hypermelanisation of the basal layer. Some of the rete ridges were interwoven. Melanophages, pigment incontinence, and dermal inflammatory infiltrate were not seen. Also, nevus cells were completely absent [Figure - 2]. The absence of basal layer degeneration and interface dermatitis ruled out lichen planus. Epidermal nevus could be reliably excluded due to the lack of characteristic epidermal changes. Based on clinicopathological correlation, we made a diagnosis of progressive cribriform and zosteriform hyperpigmentation.
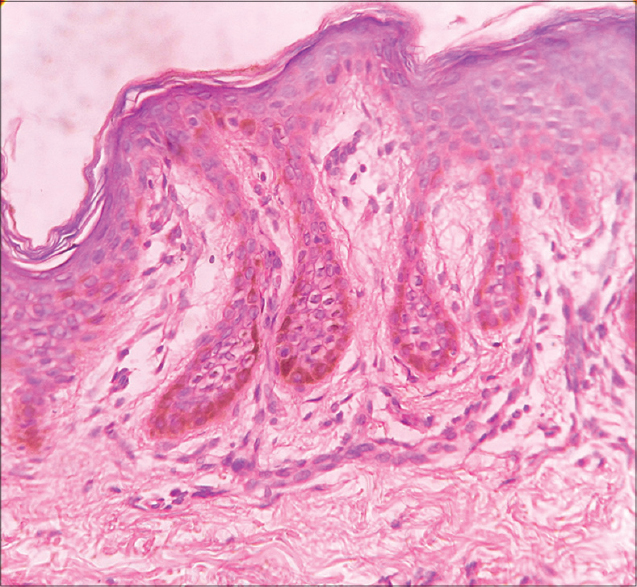 |
| Figure 2: Elongated rete ridges and hypermelanisation of basal layer, (H and E, 40×) |
Rower et al., described progressive cribriform and zosteriform hyperpigmentation in 1978. This distinctive pigmentary dermatosis has five diagnostic criteria: (1) uniformly tan cribriform macular pigmentation in a zosteriform distribution, (2) histology showing an increase in basal layer melanin along with complete absence of nevus cells, (3) absence of history of rash, injury, or inflammation to suggest post-inflammatory hyperpigmentation, (4) onset well after birth with gradual extension, and (5) lack of other associated cutaneous or internal abnormalities. [1],[2] The incidence of progressive cribriform and zosteriform hyperpigmentation is unknown; however, there is no sex predilection. [3] According to a study by Cho et al., the mean age at onset was 14.27 years (the patients included 16 men and 14 women); with the trunk being the most common site of involvement. [4]
The etiopathogenesis of progressive cribriform and zosteriform hyperpigmentation is possibly related to somatic mosaicism that develops during embryogenesis. [5] According to another school of thought, clonal migration and proliferation of embryonic melanoblasts along the lines of Blaschko could be the underlying mechanism behind this condition. Moreover, this explains the characteristic arrangement of lesions. [5],[6] Chromosomal anomalies have been reported, particularly mosaic trisomy 7, 14, 18, 20, 48, and X-chromosome mosaicism. [3]
Clinical differential diagnoses include early epidermal nevi, linear and whorled nevoid hypermelanosis, linear lichen planus, nevoid acanthosis nigricans, non-hypertrichotic variant of Becker′s nevus, third stage of incontinentia pigmenti, focal dermal hypoplasia (Goltz syndrome), X-linked reticulate pigmentary anomaly and X-linked dominant variant of chondrodysplasia punctata. [3],[4] Histologically, the entities can be differentiated from each other. Lack of vesicular and verrucous stages helped us exclude incontinentia pigmenti. In our case, histology of the lesional skin showed an increase in basal layer pigmentation as compared to adjacent normal skin, which was consistent with a diagnosis of progressive cribriform and zosteriform hyperpigmentation. Dermal vascular abnormalities and nevus cells were absent. Thus the diagnosis of progressive cribriform and zosteriform hyperpigmentation was made by exclusion.
Linear and whorled nevoid hypermelanosis (LWNH) and progressive cribriform and zosteriform hyperpigmentation are considered to be part of a spectrum, with minor differences between the two entities. Linear and whorled nevoid hypermelanosis is characterized by diffuse streaks and swirls rather than localized hyperpigmented lesions as in progressive cribriform and zosteriform hyperpigmentation. In addition, linear and whorled nevoid hypermelanosis has an early age of onset with gradual spread during the first 2 years of life with eventual stabilization. The macules may become less prominent with age in some patients. [7] Lesions of progressive cribriform and zosteriform hyperpigmentation are localized, rather than exhibiting diffuse patterns, and can multiply in a few cases. Choi et al., suggested that progressive cribriform and zosteriform hyperpigmentation may be considered to be late onset linear and whorled nevoid hypermelanosis. [2] In fact, the spectrum of progressive cribriform and zosteriform hyperpigmentation-linear and whorled nevoid hypermelanosis includes the following: "zosteriform lentiginous nevus," "zebra-like hyperpigmentation in whorls and streaks," "reticulate hyperpigmentation distributed in a zosteriform fashion," and "reticulate hyperpigmentation of Iijima." Many authors believe that these entities are similar dermatoses with different nomenclature. [8] Thus, a diffuse or localized pattern, association of congenital anomalies and age of onset constitute the key factors in differentiating linear and whorled nevoid hypermelanosis and progressive cribriform and zosteriform hyperpigmentation. The conditions may be associated with skeletal anomalies (scoliosis, body and face asymmetry, pectus excavatum, supinated varus foot), central nervous system diseases (microcephaly, arhinencephaly and epilepsy), congenital heart diseases (ventricular septal defect and tetralogy of Fallot), psychomotor delay, deafness, brachydactyly, nystagmus, anisocoria and bilateral giant cerebral aneurysms. [9],[10]
Our case was unique because she had more than one focus of lesions, which is rare in progressive cribriform and zosteriform hyperpigmentation. In the study conducted by Cho et al., up to four lesions were observed in three patients. [4] Currently, no satisfactory treatment modalities exist for this group of diseases. Topical retinoids and emollients have been tried. A medium depth peel regimen using 70% glycolic acid and 35% trichloroacetic acid (TCA) has been tried in the treatment of linear and whorled nevoid hypermelanosis, with not so promising results. [2]
| 1. |
Rower JM, Carr RD, Lowney ED. Progressive cribriform and zosteriform hyperpigmentation. Arch Dermatol 1978;114:98-9.
[Google Scholar]
|
| 2. |
Choi JC, Yang JH, Park HS, Chun DK. Progressive cribriform and zosteriform hyperpigmentation-the late onset linear and whorled nevoid hypermelanosis. J Eur Acad Dermatol Venereol 2005;19:638-9.
[Google Scholar]
|
| 3. |
Goyal T. Progressive cribriform and zosteriform hyperpigmentation: Where are we at present?. Indian Dermatol Online J 2013;4:264-6.
[Google Scholar]
|
| 4. |
Cho E, Cho SH, Lee JD. Progressive cribriform and zosteriform hyperpigmentation: A clinicopathologic study. Int J Dermatol 2012;51:399-405.
[Google Scholar]
|
| 5. |
Happle R. Mosaicism in human skin-Understanding the patterns and mechanisms. Arch Dermatol 1993;129:1460-70.
[Google Scholar]
|
| 6. |
Taibjee SM, Bennett DC, Moss C. Abnormal pigmentation in hypomelanosis of Ito and pigmentary mosaicism: The role of pigmentary genes. Br J Dermatol 2004;151:269-82.
[Google Scholar]
|
| 7. |
Kalter DC, Griffiths WA, Atherton DJ. Linear and whorled nevoid hypermelanosis. J Am Acad Dermatol 1988;19:1037-44.
[Google Scholar]
|
| 8. |
Schepis C, Alberti A, Siragusa M, Romano C. Progressive cribriform and zosteriform hyperpigmentation: The late-onset feature of linear and whorled nevoid hypermelanosis associated with congenital neurological, skeletal and cutaneous anomalies. Dermatology 1999;199:72-3.
[Google Scholar]
|
| 9. |
Nehal KS, PeBenito R, Orlow SJ. Analysis of 54 cases of hypopigmentation and hyperpigmentation along the lines of Blaschko. Arch Dermatol 1996;132:1167-70.
[Google Scholar]
|
| 10. |
Schepis C, Siragusa M, Alberti A, Cavallari V. Linear and whorled nevoid hypermelanosis in a boy with mental retardation and congenital defects. Int J Dermatol 1996;35:654-5.
[Google Scholar]
|
Fulltext Views
6,736
PDF downloads
2,041





