Translate this page into:
Proliferating trichilemmal cyst with nodal enlargement mimicking metastatic squamous cell carcinoma
2 Department of Surgical Oncology, Dr. Ram Manohar Lohia Institute of Medical Sciences, Gomti Nagar, Lucknow, India
Correspondence Address:
Kiran Preet Malhotra
Department of Pathology, Dr. Ram Manohar Lohia Institute of Medical Sciences, Gomti Nagar, Lucknow
India
| How to cite this article: Malhotra KP, Shukla S, Singhal A, Husain N. Proliferating trichilemmal cyst with nodal enlargement mimicking metastatic squamous cell carcinoma. Indian J Dermatol Venereol Leprol 2015;81:418-420 |
Sir,
Proliferating trichilemmal cysts (PTCs) are dermal or subcutaneous lesions which generally have a grotesque clinical presentation and clinically mimic squamous cell carcinoma (SCC). Recently, we encountered a tumour presenting as a large scalp mass associated with a cervical lymph node, thus suggesting a malignant aetiology. Careful histologic assessment led to the correct diagnosis.
A 30-year-old female presented with a large 5cm sized exophytic ulcerated lesion on the scalp, of 6 months duration. Several smaller ′satellite lesions′ were also noticed, surrounding the lesion [Figure - 1]. Clinical examination also revealed a firm, left upper cervical lymph node measuring 2 × 1 cm. The clinical probability of squamous cell carcinoma of the scalp with metastasis to the cervical lymph node was considered. The lesion was excised with 1 cm circumferential margins. The cervical lymph node and one of the smaller nodules (clinically suspected to be sebaceous cysts), were also resected.
 |
| Figure 1: The exophytic ulcerated scalp lesion. Several smaller nodules (arrows) (trichilemmal cysts) are also present in the vicinity |
The cut surface revealed a unilocular thick-walled cyst filled with pultaceous material. Microscopically, it was a well-circumscribed dermal lesion composed of multiple variable-sized lobules of squamous epithelium with focal palisading of the peripheral layer [Figure - 2]a. The epithelium in the center of the lobules revealed abrupt keratinization to eosinophilic amorphous keratin along with the presence of several squamous eddies [Figure - 2]b. Foreign body giant cell reaction was noted in the surrounding dermis. Atypia or mitoses were not appreciable. The smaller lesion was microscopically a trichilemmal cyst with a thin wall of squamous cells without a granular layer and a central cavity filled with amorphous keratin [Figure - 3]a. Histomorphology of the lymph node showed granulomas comprising epithelioid histiocytes and lymphocytes, some with central caseous necrosis and interspersed Langhans′ giant cells. Ziehl Neelson staining did not reveal acid-fast bacilli. No tumor was evident in the lymph node [Figure - 3]b.
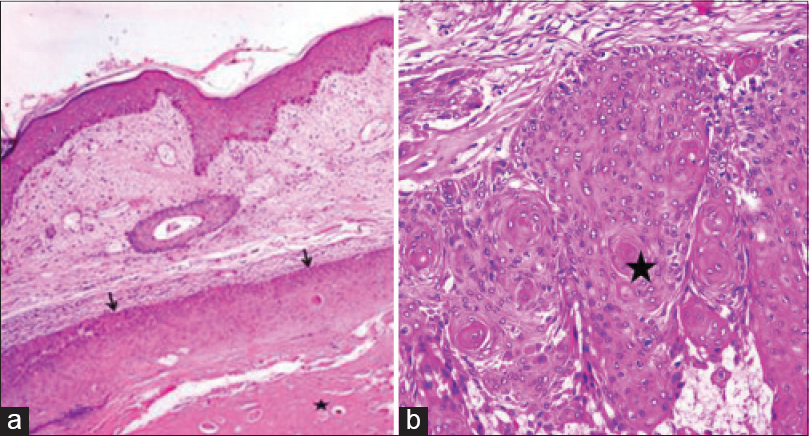 |
| Figure 2: (a) Unremarkable epidermis and a subcutaneous lesion with well-demarcated upper border (arrows) and central keratin crater (asterisk) are seen (Hematoxylin and Eosin, ×100); (b) Wall of the cyst showing lobules of squamous cells with no appreciable atypia or mitotic activity. Several squamous eddies are present (asterisk) (Hematoxylin and Eosin, ×200) |
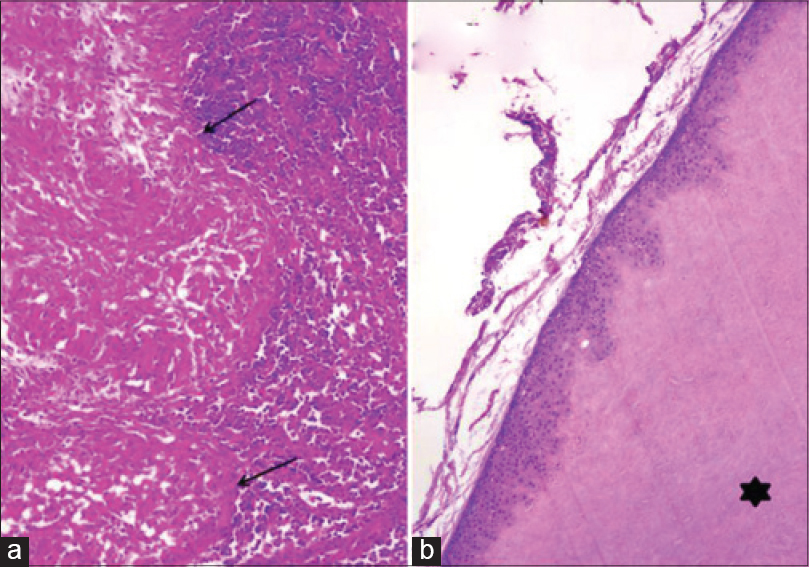 |
| Figure 3: (a) Section of the lymph node showing several epithelioid granulomas (arrows) (Hematoxylin and Eosin, ×200); (b) The smaller nodule shows a trichilemmal cyst with a thin wall devoid of granular layer and amorphous keratin content (asterisk) (Hematoxylin and Eosin, ×100) |
Microscopically, the evidence of trichilemmal keratinization in a cyst with exuberant proliferation of its wall raised the diagnostic possibilities of squamous cell carcinoma and proliferating trichilemmal cyst of benign or borderline type. Circumscription of the lesion with presence of trichilemmal keratinization and the lack of invasive foci, dysplasia or increased mitosis helped clinch the diagnosis of benign proliferating trichilemmal cyst. The granulomatous lymphadenitis was presumed to be of tubercular etiology in an Indian patient, despite a failure to demonstrate bacilli in the tissue.
The initial wide local excision was considered adequate for the diagnosis of benign proliferating trichilemmal cyst. No further surgical intervention was undertaken. Antitubercular therapy was initiated for a period of 6 months in view of the tubercular lymph node, with which the node regressed. No new scalp lesions appeared over a 1 year follow-up period.
Proliferating trichilemmal cysts are adnexal tumors variously termed as pilar tumor of the scalp, proliferating trichilemmal cyst, proliferating epidermoid cyst, proliferating tricholemmal cystic squamous cell carcinoma. [2],[4] These lesions are generally preceded by trauma or infection. They most commonly occur on the scalp, [1] the other sites being neck, trunk, groin, limbs, upper lip and buttocks. Multiple lesions have also been documented. [1],[2] They show trichilemmal keratinization without the formation of keratohyaline globules, akin to that seen in the outer root sheath of hair. [3]
Squamous cell carcinoma closely mimics proliferating trichilemmal cyst both clinically and on histology. Both lesions can occur on the scalp, in elderly patients, can acquire a grotesque appearance and can ulcerate. A clinically helpful clue to the presence of the latter is the concomitant presence of single or multiple indolent trichilemmal cysts in the vicinity of the lesion, from which the former is often seen to arise. [3] These were also seen in our case. Histologically, presence of trichilemmal keratinization, lack of anaplasia, presence of a non-infiltrative palisaded border, and absence of a premalignant epidermal lesion distinguish it from squamous cell carcinoma. Proliferating trichilemmal cysts show immunohistochemical staining for AE13 and AE14 antibodies directed at pilar-type keratin 1 and 5 polypeptides, respectively, while squamous cell carcinomas do not stain for these markers. [4]
These lesions have been categorized into Group I (benign), Group II (low-grade malignant), and Group III (high-grade malignant), depending on the presence of local infiltration and cytologic grade. [4],[5] Applying this classification, the present case belongs to Group I. Benign lesions are cosmetic problems and need resection to establish benignity. Borderline lesions may recur and require wide excision and follow-up. Malignant lesions metastasize in about 25% cases and may fare worse than squamous cell carcinoma of the skin. Wide margin clearance and long-term clinical surveillance are mandatory. [4]
Proliferating trichilemmal cysts are rare enigmatic lesions masquerading clinically as squamous cell carcinoma. Their correct recognition has an impact on treatment, outcome, and prognosis [2],[4],[5] and can prevent a therapeutic misadventure.
| 1. |
Erdem H, Yildirim U, Uzunlar AK, Sahiner C, Ozcelik D, TopluG. Posttraumatic giant proliferating trichilemmal cysts on the parietal region of the scalp. Indian J Dermatol Venereol Leprol 2011;77:707-9.
[Google Scholar]
|
| 2. |
Garg PK, Dangi A, Khurana N, Hadke NS. Malignant proliferating trichilemmal cyst: A case report with review of literature. Malays J Pathol 2009;31:71-6.
[Google Scholar]
|
| 3. |
Sethi S, Singh UR. Proliferating trichilemmal cyst: Report of two cases, one benign and the other malignant. J Dermatol 2002;29:214-20.
[Google Scholar]
|
| 4. |
Ye J, Nappi O, Swanson PE, Patterson JW, Wick MR. Proliferating pilar tumors A clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J ClinPathol 2004;122:566-74.
[Google Scholar]
|
| 5. |
Sharma R, Verma P, Yadav P, Sharma S. Proliferating trichilemmal tumor of scalp: Benign or malignant, A Dilemma.J CutanAesthet Surg 2012;5:213-5.
[Google Scholar]
|
Fulltext Views
2,778
PDF downloads
1,601





