Translate this page into:
Proximal nail fold-lunula double punch technique: A less invasive method for sampling nail matrix without nail avulsion
Correspondence Address:
Hyun Jeong Park
Department of Dermatology, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, 62 Yeouido-dong, Youngdeungpo-ku, Seoul, 150-713
Korea
| How to cite this article: Kim JE, Ahn HS, Cheon MS, Lee KJ, Cho BK, Park HJ. Proximal nail fold-lunula double punch technique: A less invasive method for sampling nail matrix without nail avulsion. Indian J Dermatol Venereol Leprol 2011;77:346-348 |
Sir,
Nail matrix disorders are common in dermatological practice. Their clinical manifestations include leukonychia, melanonychia, Beau′s line, trachyonychia, nail lichen planus, et al. [1],[2] Nevertheless, nail biopsy and histopathology have received little attention in the dermatologic literature. This may result from patients′ apprehension, such as pain from the procedure, a risk of scarring or morphologic change of the nail after nail surgeries, and the physicians′ unconcern for many different nail diseases and lack of experience about pathologic findings of nail diseases. [3],[4],[5]
The nail plate is generated by the nail matrix [Figure - 1]. The proximal nail matrix produces the lower layer of the nail plate and the distal nail matrix, namely lunula, produces the upper layer of the nail plate. Therefore, biopsies of the proximal nail matrix and lunula are essential in cases of nail matrix disorders.
Dermatologists have traditionally taken the nail matrix tissue by exposing the nail matrix after incising the proximal nail fold. [1],[2],[3],[4],[5] Although this has offered much more histopathological information to dermatologists and shown a high success rate in achieving a diagnosis, it has many disadvantages. First, the method is a complex one which needs expert skills of the operator because it needs several steps until exposure of the nail matrix, so called cul-de-sac. Second, because of the anesthesia which needs much amount of local anesthetic, the patients surely suffer from harsh pain during injection. Third, the traditional nail matrix biopsy leads to decrease in the size of the nail plate, eventually. Therefore, the patient may undergo cosmetic problems. Finally, a long period of wound healing is necessary and a postoperative scar may result.
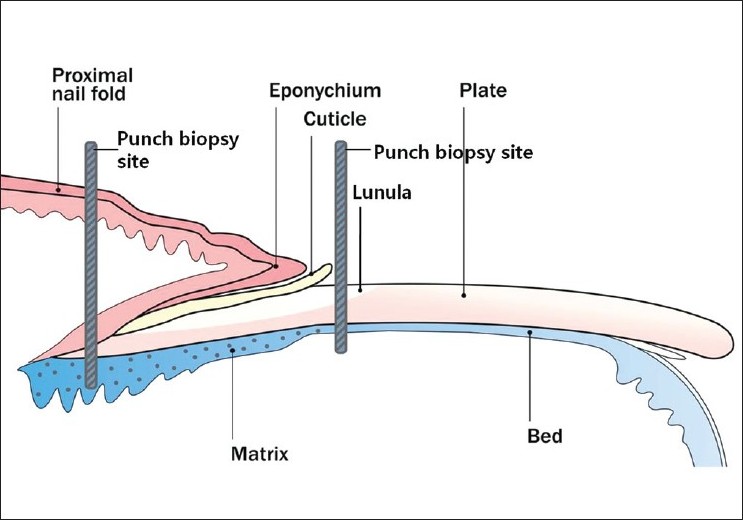 |
| Figure 1: Anatomy of the nail apparatus and schematic drawing of the biopsy sites for the proximal nail fold-lunula double punch technique |
Hence, we introduce a simple but informative method for patients with nail matrix disorders [Figure - 2]. After achieving local anesthesia that does not need lots of anesthetic as compared to the conventional method, we performed two 2-mm punch biopsies on the proximal nail fold for taking proximal nail matrix tissue. Considering the individual difference of the location of the nail matrix, we chose two different punch biopsy sites from the proximal nail fold. The 2-mm punch was advanced down to the nail matrix until the physician got the feeling of touching bone. Then, we punched through the nail plate of lunula to the underlying tissue using a 2-mm punch to obtain the distal nail matrix. Without suturing, a simple dressing with topical antibiotics was needed for three to five days. The advantages of our technique are: it is less painful, has a rapid healing time, there is almost no risk of scarring and morphological change.
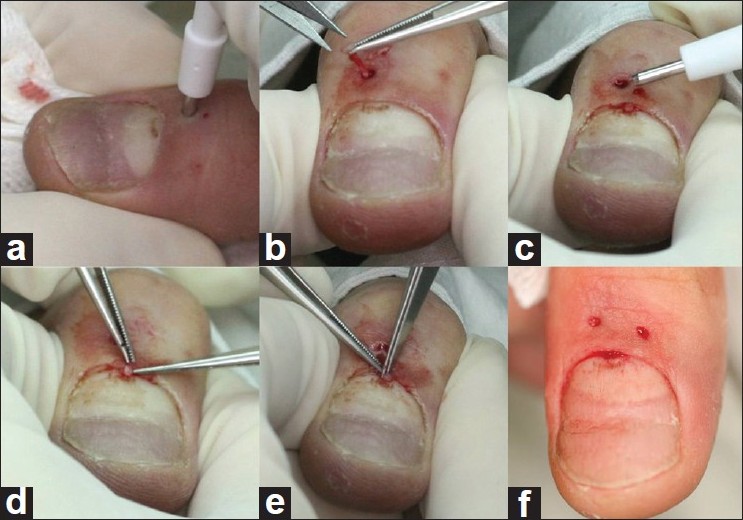 |
| Figure 2: Serial photographs of the proximal nail fold-lunula double punch technique. (a) The first punch biopsy is performed on the proximal nail fold through the nail matrix. (b) The specimen of the proximal nail matrix is obtained with careful manipulation. (c) The second punch biopsy is performed on the lunula. (d), (e) The specimen of the distal matrix is taken with a pair of forceps and a scissor. (f) The image of completion of the biopsy |
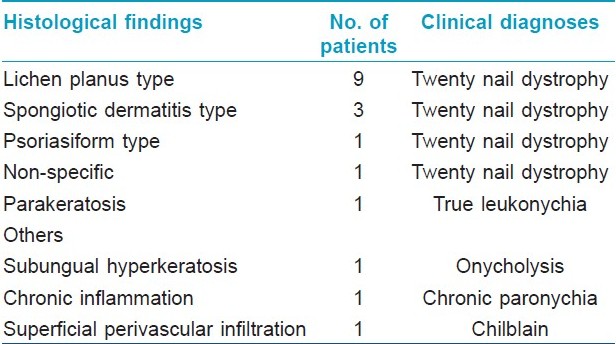
We adapted this simple technique for 18 patients which yielded the satisfactory results without exposing nail matrix. As a result we found that 17 out of 18 nail specimens contained the nail matrix (94.4%). Almost histological findings were consistent with clinical diagnoses. The method especially benefited to classify twenty-nail dystrophy into several histological types [Table - 1]. It shows a relatively high success rate in achieving a diagnosis, considering that 2-mm specimens are prone to crush injury during handling and are hard to interpret. However, matrix tissue was sometimes missing in tissue specimens because of its fragility and size. Thus we are developing an advanced technique to reduce the loss of tissue. Another limitation is that it is not suitable to be applied to a malignancy such as acral lentiginous melanoma because blind technique may not capture the atypical area of the lesion, correctly. In general, malignant lesions may be clinically distinguish from other benign lesions by using other devices such as dermoscopy, clinicians can choose more invasive and conventional technique to the doubtful cases. Therefore, our less invasive technique could be widely applicable to various benign nail disorders especially involving the nail matrix, like twenty-nail dystrophy and median nail dystrophy, and it can provide histopathologic information of whole nail tissues. The dorsal portion of the proximal nail fold, ventral part of the proximal nail fold, and the proximal nail matrix are sequentially shown in the specimen from the proximal nail fold [[Figure - 3]a]. The specimen from the lunula shows the distal nail matrix just beneath the nail plate [[Figure - 3]b].
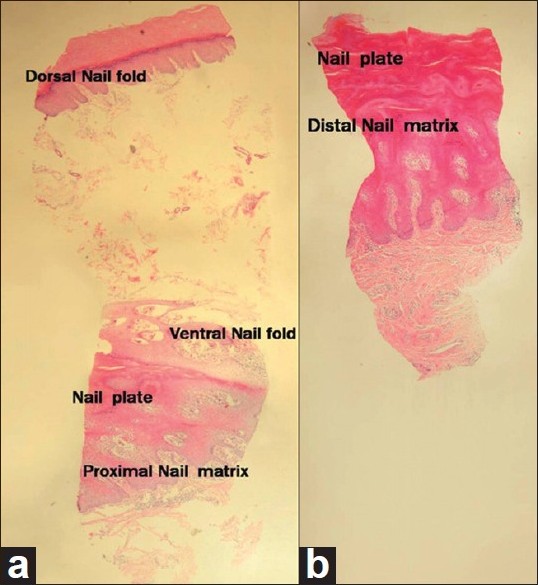 |
| Figure 3: An example of a nail biopsy specimen from a patient diagnosed with lichen planus through the proximal nail fold-lunula double punch technique. (a) Histopathologic findings of the proximal nail fold. Dorsal portion of the proximal nail fold, ventral part of the proximal nail fold, and proximal nail matrix are sequentially shown (H and E, ×40). (b) Histologic section from the lunula specimen. The specimen of the distal nail matrix shows hypergranulosis and acanthosis of the epidermis with lichenoid lymphocytic infiltration in the upper dermis (HandE, ×40) |
Since early 2009, we have got useful histopathologic findings from patients with various nail disorders through this technique. So far, no complications concerning the procedure have occurred and the physicians and the patients are all satisfied.
In summary, the proximal nail fold-lunula double punch technique is both, a physician- and patient-friendly diagnostic tool. This enables the physician to take nail biopsies more easily and to detect more histopathologic findings of inflammatory nail disorders in the future.
Acknowledgment
This work was supported by the SRC/ERC program of MOST/KOSEF (R11-2005-017-05003-0) and Basic research program through the NRF funded by the Ministry of Education, Science and Technology (2010-0002431).
| 1. |
Baran R, Dawber RP, de Berker DA, Haneke E, Tosi A. Baran and Dawber's Diseases of the nails and their management. Iowa: Blackwell Science; 2001.
[Google Scholar]
|
| 2. |
Cho BK, Kang H, Kim SY, Park YM, Park HJ, Oh ST, et al. Diseases of the nail. Seoul: Seoheung; 2009.
[Google Scholar]
|
| 3. |
Rich P. Nail biopsy: Indications and methods. Dermatol Surg 2001;27:229-34.
[Google Scholar]
|
| 4. |
Grover C, Nanda S, Reddy BS, Chaturvedi KU. Nail biopsy: Assessment of indications and outcome. Dermatol Surg 2005;31:190-4.
[Google Scholar]
|
| 5. |
Grover C, Reddy BS, Uma CK. Diagnosis of nail psoriasis: Importance of biopsy and histopathology. Br J Dermatol 2005;153:1153-8.
[Google Scholar]
|
Fulltext Views
4,464
PDF downloads
2,044





