Translate this page into:
Prurigo nodularis following the lines of blaschko – A case of superimposed segmental manifestation
Corresponding author: Dr. Shyam Bhanushankar Verma, Nirvan Skin Clinic, Vadodara, India. skindiaverma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Verma SB, Vasani R. Prurigo nodularis following the lines of blaschko – A case of superimposed segmental manifestation. Indian J Dermatol Venereol Leprol. 2024;90:652-3. doi: 10.25259/IJDVL_87_2023
Dear Editor,
A 72-year-old man, a known case of adult-onset atopic dermatitis for 10 years presented to one of us (SV) with intensely pruritic papulonodular lesions on the extensor aspects of the upper extremities and the back for the past nine weeks. He was on regular follow-ups for the past 10 years, and the disease activity was controlled with emollients, topical corticosteroids, and antihistamines. There was no defined trigger for the current aggravation. The patient was hypertensive on atenolol and aspirin for 15 years.
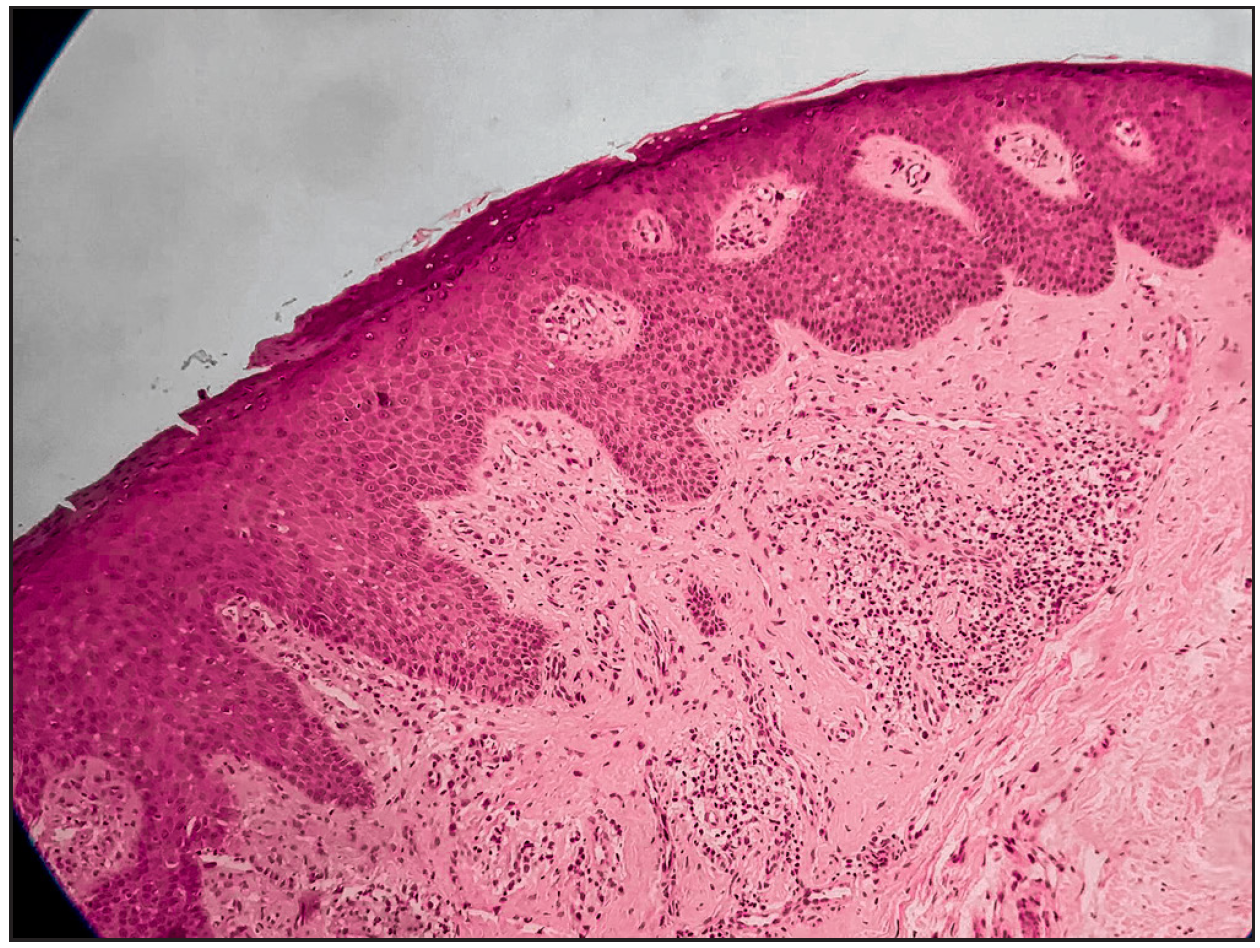
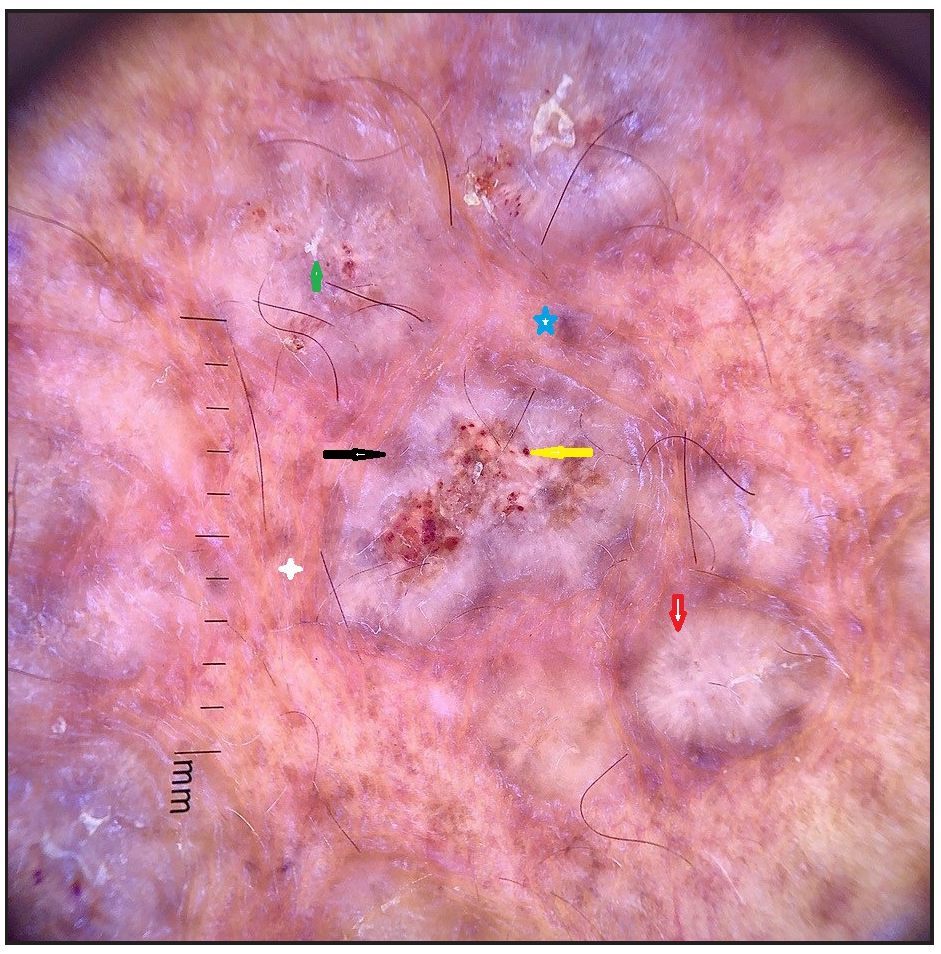
Cutaneous examination revealed strikingly linear, bilaterally symmetrical, papulonodular lesions following the lines of Blaschko over the extensor aspect of both upper arms to just above the wrists [Figure 1a]. Papulonodular lesions were scattered diffusely over the back, sparing the butterfly area and both upper thighs [Figure 1b]. Close examination revealed multiple reddish brown, firm, coalescing papules, some with superficial excoriations and perilesional erythema gradually increasing in number and size in subsequent visits [Figure 1c]. A thorough hematological, biochemical, and imaging screening revealed no systemic illness. Serum IgE level was 410IU/ml. Histopathology [Figure 2a] and dermoscopy [Figure 2b] were consistent with the diagnosis of prurigo nodularis. He was treated with topical clobetasol propionate cream once a day for three weeks with occlusion and then without, for further two weeks, with an emollient cream applied several times a day, levocetirizine 5 mg in the morning and hydroxyzine 25 mg at night. The importance of strict avoidance of scratching and rubbing was emphasized. However, the lesions recurred after a brief period of improvement. The patient was then given oral cyclosporine at 4 mg/kg, improving the itch and the severity of lesions in two months. Significant flattening of lesions with hyperpigmentation was seen after four months [Figure. 3], and the drug was tapered gradually in the next two months. The patient is in remission with regular application of emollients and mometasone cream on weekends.

-
Bilaterally symmetrical, linearly distributed, individual, and coalescing papules with perilesional erythema in Blaschkoid distribution on the extensor aspect of the forearm extending to the arm.

-
Excoriated papulonodular lesions on an eczematous base involving the back and sparing the butterfly area of the back.

-
Closer picture of multiple reddish brown, firm, coalescing papules, some with superficial excoriations and perilesional erythema, demonstrating the Blaschkoid distribution on the upper arm.
-
H& E- 100x - Acanthotic epidermis with hyperkeratosis and focal parakeratosis. Dermis shows mild fibrosis, thickened collagen bundles, and admixed perivascular lymphocytic infiltrate.
-
Polarised mode of dermoscopy. (Dermlite DL3Gen, USA). Annotations Red arrow – peripheral white striations giving white starburst pattern, Yellow arrow and Green arrow - scale, Black arrow - perilesional hyperpigmentation, White star – telangiectasia and atrophy, Blue star – blue grey globule.

-
Significantly resolved and flattened lesions with post-inflammatory hyperpigmentation.
Skin disorders with a polygenic background sometimes show a pronounced linear/segmental or Blaschkoid distribution. That may present as an isolated disorder or be superimposed on less severe, disseminated, symmetrically distributed lesions of the same disorder. These Blaschkoid lesions represent a counterpart of type 2 segmental mosaicism of monogenic skin diseases, and the phenomenon is referred to as ‘superimposed segmental manifestation‘. 1 It is explained by the loss of heterozygosity concerning one of the genes during the precocious stage of development, causing the clonal outgrowth of a population of cells that increases the predisposition to atopic dermatitis. It has been described earlier with atopic dermatitis and other conditions 2 such as dermatomyositis, psoriasis, lichen planus, lichen planopilaris, and vitiligo.
In the present case, the aggravation of atopic dermatitis in a Blaschkoid pattern on the upper extremities, manifesting as pruriginous nodules 3 with similar lesions scattered elsewhere, is an example of superimposed segmental manifestation. The non-response to conservative treatment with topical clobetasol and emollients necessitating oral immunosuppressive therapy confirms that such presentations can be notoriously refractory to treatment. 4 Patients like ours offer an opportunity to identify intraindividual genetic variations marking loci involved in the pathogenesis of atopic dermatitis, eventually leading to targeted treatment.2
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Superimposed segmental manifestation of polygenic skin disorders. J Am Acad Dermatol. 2007;57:690-9.
- [CrossRef] [PubMed] [Google Scholar]
- Superimposed type 2 segmental atopic dermatitis: Case series and review of the literature. ClinExp Dermatol. 2022;47:1703-6.
- [Google Scholar]
- EADV European prurigo project: expert consensus on the definition, classification and terminology of chronic prurigo. J EurAcad Dermatol Venereol. 2018;32:1059-65.
- [Google Scholar]
- A linear lesion in a child with atopic dermatitis: Not a coincidence. Clin Case Rep. 2019;7:1667-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





