Translate this page into:
Pseudorheumatoid nodules in a young woman
Corresponding author: Dr. Rachita S Dhurat, Department of Dermatology, Venereology and Leprosy, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, Maharashtra, India. rachitadhurat@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Kowe P, Golwad PM, Srivatsa K R P, Dhurat R S. Pseudorheumatoid nodules in a young woman. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1543_2024
Dear Editor,
Asymptomatic, skin-coloured nodules, typically located over bony prominences, can present a clinical challenge when they appear without other systemic signs. In such cases, a comprehensive biochemical and histopathological evaluation becomes crucial for reaching a definitive diagnosis.
A 27-year-old woman presented with asymptomatic skin lesions on both her knuckles and elbows for four months. Initially small, the lesions had gradually increased in size.papules gradually enlarged to their then-current size. On cutaneous examination, well-defined, skin-coloured to erythematous, non-tender, non-pruritic, smooth-surfaced nodules measuring approximately 3-4 mm, were noted on the bilateral dorsal interphalangeal joints of the index and middle fingers, as well as on both elbows [Figures 1a and 1b]. These nodules were not fixed to the underlying tissue. There were no other mucocutaneous findings or joint abnormalities. Polarised dermoscopy using a 3 Gen DermLite DL4 (CA, USA) at 10x magnification revealed structureless yellow-white areas at the centre, linear vessels, a whitish-brown background, and peripheral white scales [Figure 1c]. Systemic examination was unremarkable.

- Skin-coloured, smooth-surfaced, asymptomatic nodules over the dorsum of the bilateral hand.

- Skin-coloured nodule over bilateral elbow joints.
![Dermoscopy showing yellow-white area in the centre (red arrow), blurred vessels (black arrow), whitish-brown area in the background (blue arrow) and peripheral white scale [DermLite DL4, 10x magnification, polarised mode].](/content/126/2025/0/1/img/IJDVL_1543_2024-g3.png)
- Dermoscopy showing yellow-white area in the centre (red arrow), blurred vessels (black arrow), whitish-brown area in the background (blue arrow) and peripheral white scale [DermLite DL4, 10x magnification, polarised mode].
The nodule over the right finger dorsum was excised and sent for histopathological analysis. A well-circumscribed inflammatory infiltrate involving the deep dermis and subcutaneous tissue was seen. This infiltrate was composed predominantly of histiocytes, epithelioid cells and lymphocytes in a palisading pattern. There were areas of degenerated collagen (eosinophilic fibrous material) at the centre [Figures 2a-2c]. Alcian blue staining for mucin was negative. Her rheumatoid factor, anti-cyclic citrullinated peptide (CCP) antibodies, anti-nuclear antibodies were negative and hand joint X-rays (lateral and oblique view) were normal. Based on the clinical presentation and histopathological findings, a final diagnosis of pseudorheumatoid nodule (deep granuloma annulare) was made. The patient was treated with intralesional triamcinolone acetonide 5 mg/mL, administered at four-week intervals with good improvement in two doses [Figures 3a and 3b].
![Well-circumscribed inflammatory infiltrate in the deep dermis and upper subcutaneous tissue [Haematoxylin & eosin, 40x].](/content/126/2025/0/1/img/IJDVL_1543_2024-g4.png)
- Well-circumscribed inflammatory infiltrate in the deep dermis and upper subcutaneous tissue [Haematoxylin & eosin, 40x].
![Areas of altered collagen in the centre (eosinophilic material) (blue arrows) surrounded by palisading of the inflammatory cell (black arrow) [Haematoxylin & eosin, 100x].](/content/126/2025/0/1/img/IJDVL_1543_2024-g5.png)
- Areas of altered collagen in the centre (eosinophilic material) (blue arrows) surrounded by palisading of the inflammatory cell (black arrow) [Haematoxylin & eosin, 100x].
![Fibrinous degeneration of collagen (blue arrows) surrounded by palisading of histiocytes [Haematoxylin & eosin, 400x].](/content/126/2025/0/1/img/IJDVL_1543_2024-g6.png)
- Fibrinous degeneration of collagen (blue arrows) surrounded by palisading of histiocytes [Haematoxylin & eosin, 400x].
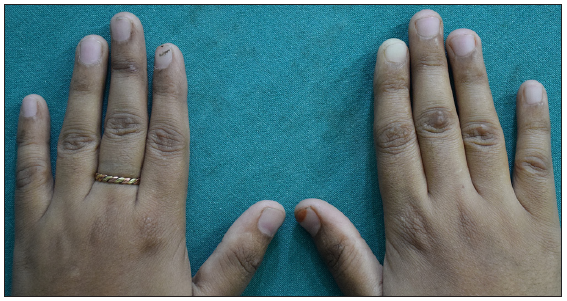
- Post-treatment images of the dorsum of both hands.

- Post-treatment images of both elbow joints.
Pseudorheumatoid nodules refer to nodules in the reticular dermis and subcutaneous tissue that resemble the histological features of rheumatoid nodules but can form in the absence of rheumatoid arthritis (RA) or other collagen vascular diseases like systemic lupus erythematosus, systemic sclerosis, etc.1 These nodules are believed to represent a deep form of granuloma annulare (GA), particularly the subcutaneous or nodular variant, due to the presence of palisading granulomas mainly in the deep dermis and subcutis.1 Most cases occur in children and young adults and typically have a favourable prognosis.2-4 The condition commonly affects the lower legs and scalp in children, often resolving spontaneously, though recurrence at the same site and the development of new nodules are frequent.3,4 Pseudorheumatoid nodules are rare in young women, but when they do occur, they typically involve the interphalangeal joints and elbows.1,3
The exact cause of pseudorheumatoid nodules remains unclear. There are several potential triggers, including insect bites, infections (such as Borrelia, Herpes, Streptococcus, and Epstein-Barr virus), phototherapy, trauma, surgery and medications like methotrexate and other disease-modifying antirheumatic drugs.4 Evidence suggests that these triggers elicit an immunological response in the form of a delayed-type hypersensitivity reaction regulated by T-lymphocytes, which results in a panniculitis-type inflammatory response resulting in granuloma formation.4 Pseudorheumatoid nodules may be confused with similar appearing entities clinically and can pose a dilemma in diagnosis. These can be differentiated based on certain characteristics [Table 1].5 Histologically, subcutaneous GA nodules show a predominance of large histiocytes surrounding mucin and altered collagen. However, the presence of mucin is not a prerequisite for diagnosis, which is why subcutaneous GA and rheumatoid nodules are often histologically indistinguishable., Hence the term, “pseudorheumatoid.”1 Rheumatoid nodules, which are extra-articular manifestations of RA, may precede the onset of rheumatoid disease, and testing for rheumatoid factor and anti-CCP antibodies can assist in early RA diagnosis.6
| Patient characteristics | Rheumatoid nodule | Pseudorheumatoid nodule | Rheumatic fever nodules5 |
|---|---|---|---|
| Age | Middle age | Typically, in children, rare in adults | Children (5 to 15 years) |
| Sex | Male > Female | Female > Males | Equal predisposition |
| Association | Rheumatoid arthritis, collagen vascular diseases. | No associations | Rheumatic fever. The presence of these nodules indicates the involvement of cardiac valves and severe rheumatic heart disease (RHD). |
| Arrangement | Asymmetrical | Symmetrical | - |
| Site | Areas of repetitive trauma-like fingers, heels, back of forearms | Scalp, palm, buttocks | Elbows, knees, scalp, knuckles, ankles, spine (mainly periarticular). |
| RA factor | Positive | Negative | Negative |
| Histopathology | Central fibrinoid necrosis, fibrin aggregates, palisading mononuclear cells, perivascular lymphocytic infiltration. Mucin may be present. | Central fibrinoid collagen degeneration, palisading histiocytes. Mucin may be present. | Central necrosis, no palisading of histiocyte, perivascular lymphocytic, neutrophilic infiltration with vessel wall thickening. No mucin deposition. |
| Treatment | Treatment of underlying rheumatoid arthritis will resolve these nodules. |
Intralesional corticosteroids are most effective. Others include surgical excision, cryotherapy, isotretinoin, potassium iodide, clorambucil, dapsone, rifampicin, ofloxacin, minocycline, etc. Recurrence is common. |
Treatment of underlying rheumatic fever. |
On dermoscopy, GA presents with blurry vessels and a pinkish-red background, followed by areas of white, yellow, or orange.7 In our patient, the yellow-white areas likely correspond to the palisading granulomas, while the central structureless white areas may indicate sclerosis due to altered collagen, as seen in histopathology. Among the available treatments, intralesional corticosteroids are considered a first-line and effective therapy wherever feasible. However, recurrences are common. This approach is preferred over topical steroids, as the drug is delivered directly to the target site, reducing time to resolution.8 Other treatment options include surgical excision, cryotherapy, dapsone, chlorambucil, isotretinoin and potassium iodide.2,4 A recent report of subcutaneous GA treated with a three-month regimen of rifampicin, ofloxacin, and minocycline showed no improvement.2
In conclusion, pseudorheumatoid nodules in adults are a distinct clinical and pathological entity that may be mistaken for rheumatoid nodules. Given the rarity of this condition, a careful clinicopathological correlation is essential for accurate diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Noninfectious granulomas. In: Elder DE, ed. Levers’s Histopathology of the Skin (11th edition). Philadelphia: Wolter Kluwer; 2015. p. :865-76.
- [Google Scholar]
- Pseudorheumatoid nodule: A variant of granuloma annulare? Dermatol Online J. 2020;26
- [CrossRef] [Google Scholar]
- Pseudorheumatoid nodules in adults. Am J Dermatopathol. 2005;27:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous granuloma annulare. Acta Dermatovenerol Croat. 2017;25:292-4.
- [PubMed] [Google Scholar]
- Acute rheumatic fever: A review of essential cutaneous and histological findings. Cureus. 2021;13:e12577.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous manifestations of rheumatoid arthritis: Diagnosis and treatment. J Pers Med. 2023;13:1479.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermoscopy of granuloma annulare: A clinical and histological correlation study. Dermatology. 2017;233:74-9.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous granuloma annulare: A systematic review of a rare and underdiagnosed disease. Int J Dermatol. 2024;64:246-55.
- [CrossRef] [PubMed] [Google Scholar]





