Translate this page into:
Recurrent spontaneous forehead ecchymoses with headache: A distinctly curious phenomenon
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Kanika Sahni
Department of Dermatology and Venereology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029
India
| How to cite this article: Gupta V, Agrawal S, Abhishek G N, Agarwal S, Sahni K. Recurrent spontaneous forehead ecchymoses with headache: A distinctly curious phenomenon. Indian J Dermatol Venereol Leprol 2020;86:289-291 |
Sir,
Spontaneous facial ecchymoses in association with headache termed as “spontaneous extracranial hemorrhagic phenomena”(SEHP) are rarely reported. Herein we present two patients with these features.
Case 1
A 31-year-old, otherwise healthy, female presented to us in May 2017 with one year history of recurrent episodes of right-sided moderate-to-severe headaches temporally associated with ecchymotic patches on ipsilateral temporal forehead. There were one to two episodes of headache every month, lasting for 30 to 60 minutes, without aura, photophobia or nausea. The patient reported appearance of asymptomatic reddish macules over her right forehead with the onset of headache which would subside in a week without any sequelae [Figure - 1]. Her complete blood count and coagulation profile were normal. Skin biopsy was unremarkable except for a few dilated capillaries. A non-contrast computed tomographic scan of head was normal. She was referred to the neurology department for management of her headache but was lost to follow-up.
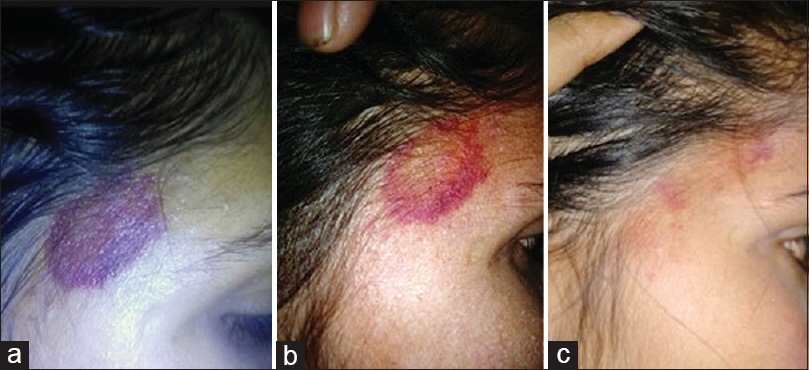 |
| Figure 1: Patient 1: Photographs (clicked by patient's smartphone at home) showing evolution of ecchymosis on the right temporal forehead day (a) 3 of its appearance, (b) 5 of its appearance, (c) 6 of its appearance |
Case 2
A 37-year-old female consulted us in December 2018 for multiple episodes of spontaneous ecchymoses affecting her bilateral temporal and preauricular regions [Figure - 2] simultaneously for the last 6 months. She had a chronic low-grade dull generalized headache for the last one year, with 2 to 3 episodes of severe throbbing headache every month lasting for a few hours. The severe headache episodes were not localized to any side, were not associated with nausea, vomiting, lacrimation, rhinorrhea, or visual or sensory aura, and did not have any triggers. The ecchymotic episodes temporally coincided with only her severe headache episodes, occurring 12 to 24 hours after the headache onset and resolved over the next 7 to 10 days. Her past medical and family history was not significant. Neurological and ophthalmological evaluations were normal. Her hemogram, thyroid stimulating hormone level, prothrombin time and magnetic resonance imaging of the brain did not reveal any abnormality. Skin biopsy from the ecchymotic areas showed a “bland” red blood cell extravasation in the dermis [Figure - 3]. A diagnosis of “unclassified headache disorder” was made by the neurologist, and she was treated with oral amitriptyline 25 mg daily, and a combination of naproxen and domperidone was prescribed for the more severe headache episodes. There was significant improvement in her low-grade chronic headache along with reduction in the intensity and frequency of severe episodes. However, she continued to have ecchymoses, though less severe than before with the episodes of severe headache.
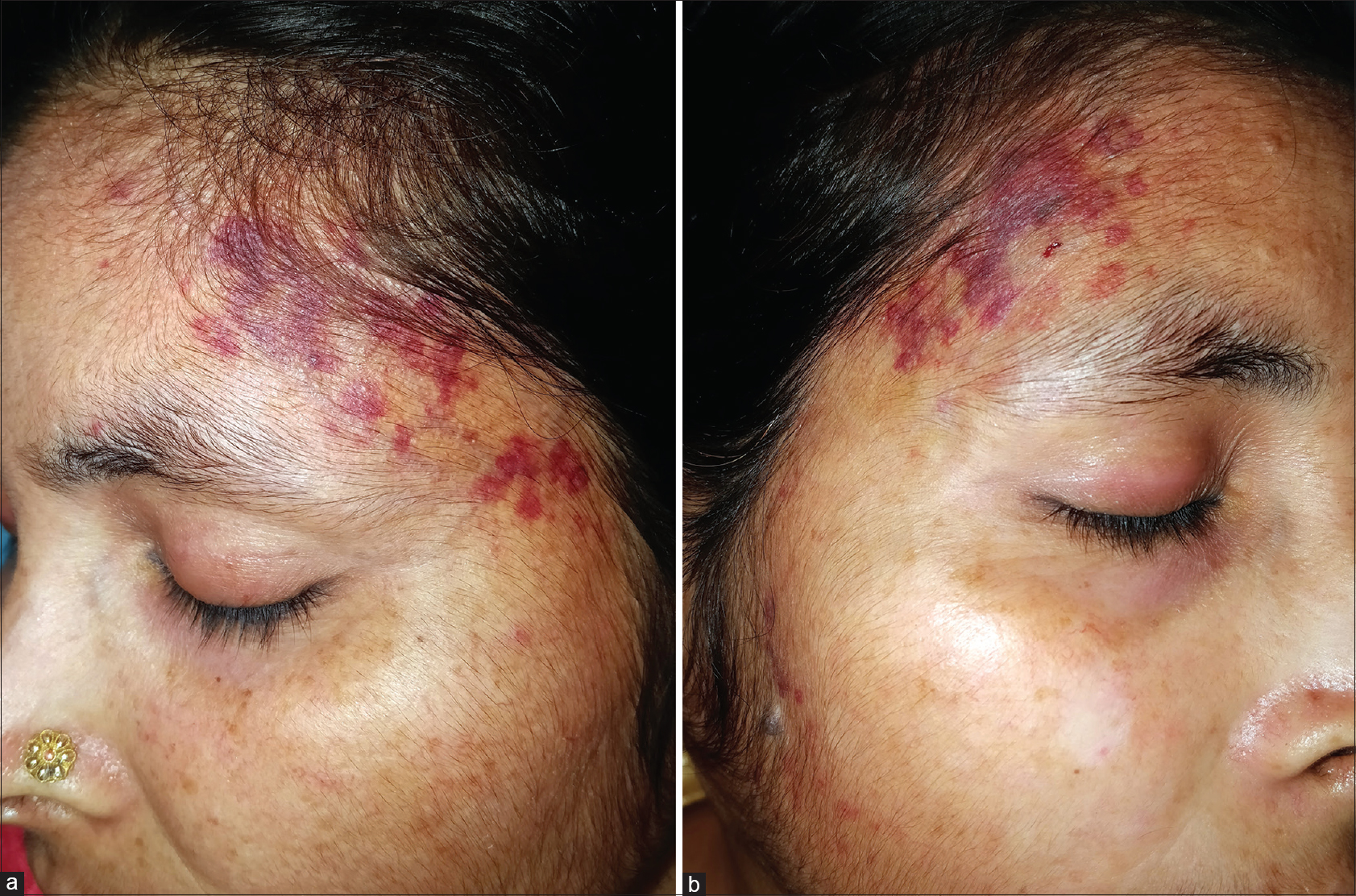 |
| Figure 2: Patient 2 showing ecchymoses on the bilateral temporal forehead extending to the preauricular area on day 3 of headache a) Left side, b) Right side |
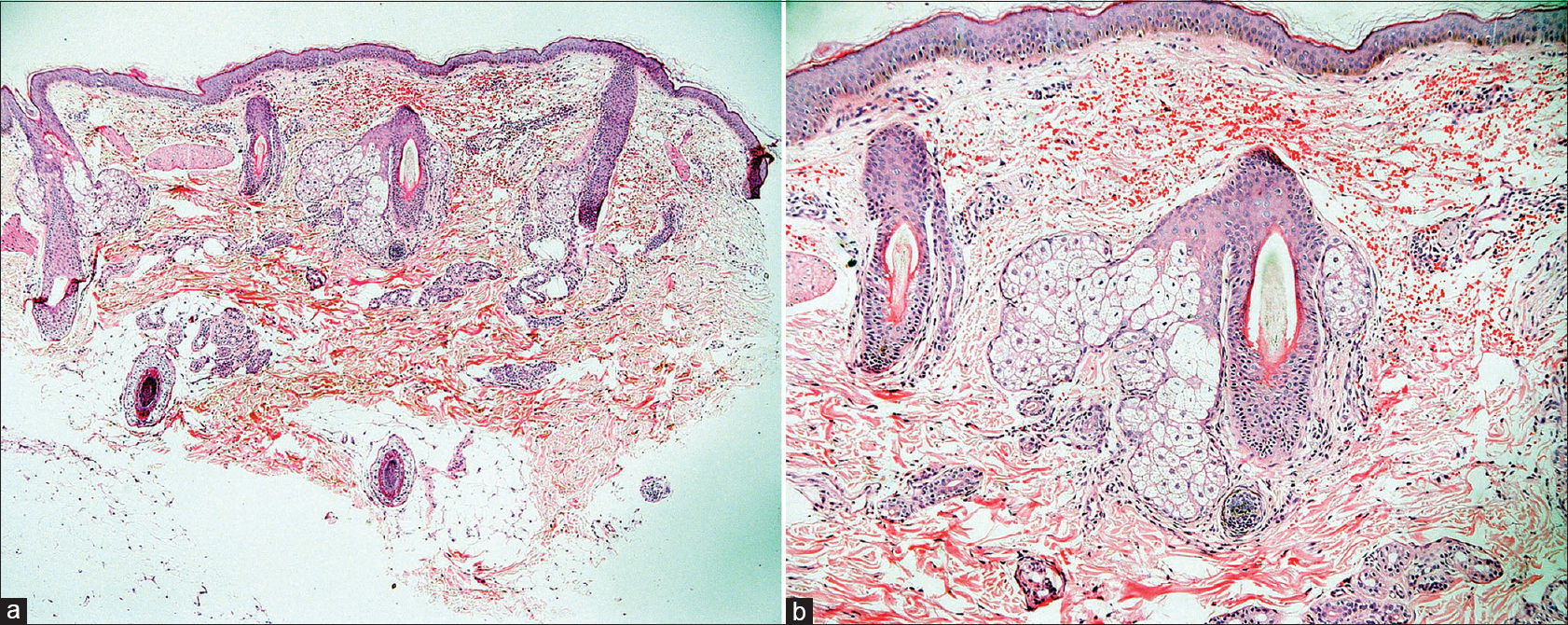 |
| Figure 3: Skin biopsy showing erythrocyte extravasation in the dermis, with the absence of vessel damage or inflammatory infiltrate (H and E) a) 40×, b) 100× |
SEHP are poorly characterized and largely unrecognized. Some headaches such as migraine and trigeminal autonomic cephalalgias are known to be associated with autonomic and vasomotor features, such as lacrimation and conjunctival injection, resulting from activation of trigeminal-autonomic reflex causing sterile neurogenic inflammation. Though the pathogenic basis is not clear, SEHP may also occur due to a similar process resulting in an increased parasympathetic outflow to the head and neck vasculature.[1],[2],[3] Bleeding can occur not only into the skin (ecchymoses) but also from the nose (epistaxis) or through the sweat glands (hematohidrosis). A systematic review identified 105 cases with this phenomenon, of which 41 had ecchymoses.[3] Usually, the ecchymosis occurs on the ipsilateral side of headache but can be bilateral as well. Common sites include temporal, periorbital, conjunctival, buccal, preauricular and glabellar areas. The first episode of hemorrhage usually happens after a median of 1.5 (range 0–3) years after the onset of headache. Ecchymoses and severe episodes of headache coincide temporally with ecchymosis manifesting a few (median 21) hours after the onset of headache. Most of the reports are in the setting of trigeminal autonomic cephalalgias (87%) or migraine (33%). Females are roughly three times more frequently affected than males. The median age of presentation is 46 years, which is slightly higher than that of our cases. Long-term follow-up data is not available for majority of these patients, however it appears that the condition may resolve on its own, though some may continue to have recurrent episodes.[3]
Spontaneous ecchymoses can be seen in patients on anticoagulant therapy, certain bleeding diatheses, Gardner Diamond syndrome and primary systemic amyloidosis. Gardner Diamond syndrome, also known as psychogenic purpura, presents as spontaneous painful bruises in adult women, mostly in the setting of an underlying psychiatric illness.[4] Ecchymoses in association with severe headache should also raise the suspicion of a self-injury behavior secondary to headache.[5] However, our patients were otherwise healthy, did not have a psychiatric illness, were not on any medications, experienced ecchymoses only on the forehead and only associated with severe headache episodes, and denied any self-injury behavior, coughing, sneezing or any other Valsalva maneuvers making the other differential diagnoses unlikely. Though most of the reports are from neurology and allied specialties, such patients can present to the dermatologist as well owing to the striking and sometimes alarming skin manifestations. By reporting these two cases, we wish to increase the awareness regarding this rare but distinctive phenomenon among the dermatologists.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Akerman S, Holland PR, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci 2011;12: 570-84.
[Google Scholar]
|
| 2. |
Drummond PD. Mechanisms of autonomic disturbance in the face during and between attacks of cluster headache. Cephalalgia 2006;26: 633-41.
[Google Scholar]
|
| 3. |
Peretz AM, Woldeamanuel YW, Rapoport AM, Cowan RP. Spontaneous extracranial hemorrhagic phenomena in primary headache disorders: A systematic review of published cases. Cephalalgia 2016;36: 1257-67.
[Google Scholar]
|
| 4. |
Thokchom NS, Pradeepa D, Hafi NA, Verma K. Clinical spectrum of autoerythrocyte sensitization syndrome: A series of five cases. Indian Dermatol Online J 2018;9: 110-3.
[Google Scholar]
|
| 5. |
Colman I, Kingsbury M, Sareen J, Bolton J, van Walraven C. Migraine headache and risk of self-harm and suicide: A population-based study in Ontario, Canada. Headache 2016;56: 132-40.
[Google Scholar]
|
Fulltext Views
5,349
PDF downloads
2,227





