Translate this page into:
Recurrent unilateral angiolymphoid hyperplasia with eosinophilia in pregnancy
2 Department of Dermatology, Venereology and Leprosy, Government Medical College, Nizamabad, Telangana, India
Correspondence Address:
Sudha Rani Chintagunta
Plot No. 5, Jupiter Colony, Kakaguda, Kharkhana, Secunderabad, Telangana
India
| How to cite this article: Damarla SV, Chintagunta SR, Arakkal GK. Recurrent unilateral angiolymphoid hyperplasia with eosinophilia in pregnancy. Indian J Dermatol Venereol Leprol 2018;84:325-327 |
Sir,
Angiolymphoid hyperplasia with eosinophilia is a benign vasoproliferative disorder of unknown etiology involving the skin and subcutaneous tissue. Synonyms include inflammatory angiomatous nodule, pseudopyogenic granuloma, intravenous atypical vascular proliferation, histiocytoid hemangioma and epitheloid hemangioma. It is characterized by solitary or multiple, reddish brown intradermal or subcutaneous papules and/or nodules. The most common sites involved are the head and neck, particularly the region around the ears, forehead or scalp.[1] Rarely, it is reported on the hand, shoulder, breast, tongue, eyelid, orbit, conjunctiva, penis and scrotum. Extracutaneous involvement includes oral mucosa, lacrimal gland, parotid gland, mandible, heart, liver, spleen, colon, bone and blood vessels. Etiology is not exactly known; several factors including insect bite, infections, trauma, immunologic factors and hyperestrogenic states are implicated in the pathogenesis. Though the relationship between pregnancy and angiolymphoid hyperplasia with eosinophilia is not exactly established, hyperestrogenic states and increased level of estrogen and progesterone receptors in the lesions during pregnancy has been reported. Estrogens may also have an indirect role without any overexpression of estrogen and progesterone receptors.[1] Very few cases of pregnancy-related angiolymphoid hyperplasia with eosinophilia have been reported in the literature.[1],[2],[3],[4],[5] We report a case of recurrent unilateral angiolymphoid hyperplasia with eosinophilia involving the entire left upper extremity, axilla and trunk in three successive pregnancies.
A 28-year-old woman, P3L3, presented with multiple angiomatous growths on the left upper limb for a duration of 8 months. The lesions started as asymptomatic, dark-colored papules on the left hand that gradually increased in size and number covering the entire limb. Thepatient had similar lesions during her first and second pregnancy which started during second trimester. Few lesions regressed spontaneously postpartum and the persisting lesions were removed by electrosurgery. Thepatient developed similar lesions during her third pregnancy which were persistent for 8 months. Cutaneous examination revealed multiple, discrete, erythematous papulonodules on the left upper limb with some lesions in the left axilla and back, unilateral in distribution. Size of the lesions varied from 1 to 6 cm. Crusting was seen in some lesions [Figure - 1], hyperpigmented tender plaques were present on the left forearm [Figure - 2] and left palm. General and systemic examinations were unremarkable. A differential diagnosis of angiokeratoma, pyogenic granuloma, angiolymphoid hyperplasia with eosinophilia and Kimura's disease were considered.
 |
| Figure 1: Multiple angiomatous papules and nodules involving the axilla, upper arm and fore arm |
 |
| Figure 2: Multiple angiomatous papules and nodules and pigmented plaques on the fore arm and hand |
Two skin biopsies of sizes 0.3 and 0.5 cm were taken from papule and plaque type lesions, respectively. Sections studied from the papule showed keratinized stratified squamous epithelium and angiomatous tissue composed of lobules of small capillary stroma with extensive eosinophilic infiltration [Figure - 3]. Sections from the plaque lesion showed dermal tissue revealing proliferation of small- to medium-sized blood vessels. Also seen was extensive perivascular inflammatory cell infiltrate composed mainly of lymphocytes and eosinophils suggestive of angiolymphoid hyperplasia with eosinophilia [Figure - 4].
 |
| Figure 3: Congested endothelial-lined vessels with scattered eosinophils (H and E, ×10) |
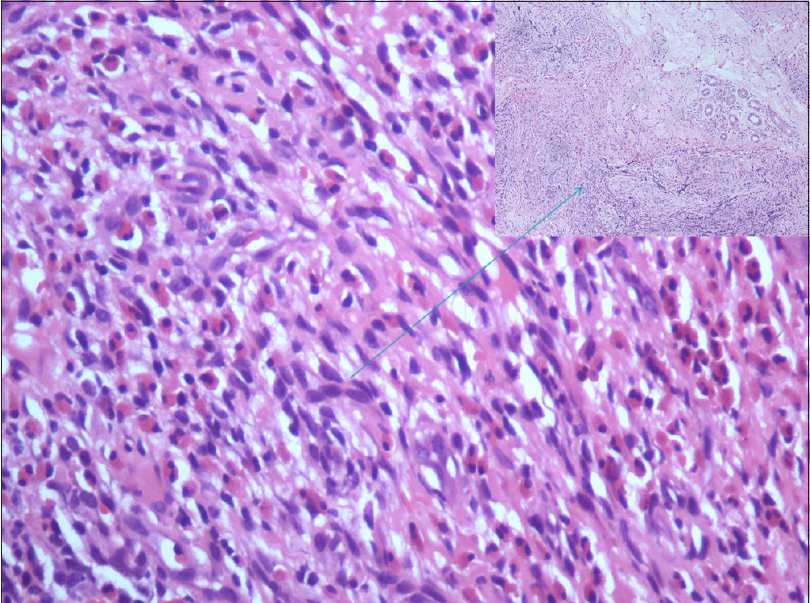 |
| Figure 4: Eosinophil-rich infiltrate with prominent vessels (H and E, ×20) |
In angiolymphoid hyperplasia with eosinophilia, clinical and histological patterns vary depending on the age of the lesion. In early or actively growing stage, the vascular component predominates, whereas in later stage, lymphocytes become more prominent. In the early stage, vessels are immature with prominent epithelioid endothelial cells and in the later stage, the lymphoid infiltrate predominates, so the endothelial cells lining the maturing vessels become smaller and less epithelioid.[1]
Kimura's disease is a chronic inflammatory disease that usually involves deep subcutaneous tissue and lymph nodes of the head and neck region. Clinically, it presents as large subcutaneous nodules and plaques with overlying normal skin with peripheral blood eosinophilia. Histology shows florid lymphoid follicles with germinal center formation, eosinophilic infiltrate, eosinophilic microabscesses and fibrosis. Neoangiogenesis with plump endothelial cells are generally absent which is a hallmark feature in angiolymphoid hyperplasia with eosinophilia.
Pyogenic granuloma consists of tight aggregates of capillary-sized vessels that grow in a lobulated fashion in a fibromyxoid stroma and eosinophils are absent.
Clinically, angiolymphoid hyperplasia with eosinophilia plaques can mimic Kimura's disease and nodules with crusting can be confused with pyogenic granuloma. In this case, a diagnosis of angiolymphoid hyperplasia with eosinophilia was made based on the histopathology.
Angiolymphoid hyperplasia with eosinophilia is a reactive inflammatory lesion involving skin and subcutaneous tissue characterized by solitary or multiple, red to brown papules or nodules. In general, the lesions are localized and unilateral in distribution. The lesions are intradermal or subcutaneous, but may involve deep soft tissues and vessels. Therapeutic options include surgical excision, ablative laser therapy, cryotherapy, intralesional radiofrequency, topical or intralesional corticosteroids, isotretinoin, oral propranolol, topical timolol, topical imiquimod, tacrolimus, interferon alfa-2a and anti-interleukin 5 antibody (mepolizumab).
Our case clinically presented with two types of lesions: angiomatous papulonodules (dermal involvement) which is a common feature of angiolymphoid hyperplasia with eosinophilia and few erythematous to bluish, tender plaques (subcutaneous process) on the palm and forearm, mimicking Kimura's disease. Histology of the papule mimicked pyogenic granuloma, the associated eosinophil-rich infiltrate differentiating it from pyogenic granuloma, whereas histopathology of plaque lesion was suggestive of angiolymphoid hyperplasia with eosinophilia.
Only very few cases of pregnancy-related angiolymphoid hyperplasia with eosinophilia have been reported in the literature.[1],[2],[3],[4],[5] Literature search showed about 20 cases from India so far and four cases were related to pregnancy. It can develop during pregnancy [1],[2],[3],[5] or the existing lesions may increase in number or size during pregnancy.[4] Spontaneous complete or partial regression is reported in the postpartum period; in our case the lesions were persistent even 8 months after delivery. Pregnancy is considered as a predisposing factor for increased vascular proliferation based on clinical data favoring the role of estrogen in angiolymphoid hyperplasia with eosinophilia.[1] In our case, though the distribution was unilateral, it was not localized, with multiple lesions involving the entire left upper extremity, axilla and trunk, with morphological variation in presentation (papules, nodules and plaques) and recurrence in three successive pregnancies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for the images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Olsen TG, Helwig EB. Angiolymphoid hyperplasia with eosinophilia. A clinicopathologic study of 116 patients. J Am Acad Dermatol 1985;12:781-96.
[Google Scholar]
|
| 2. |
Zarrin-Khameh N, Spoden JE, Tran RM. Angiolymphoid hyperplasia with eosinophilia associated with pregnancy: A case report and review of the literature. Arch Pathol Lab Med 2005;129:1168-71.
[Google Scholar]
|
| 3. |
Hollo P, Marschalko M, Sikos G, Harsing J, Horvath A. Angiolymphoid hyperplasia with eosinophilia in pregnancy. J Eur Acad Dermatol Venereol 2005;19:645-6.
[Google Scholar]
|
| 4. |
Ceyhan AM, Akkaya VB, Yildirium M, Karahan N. A case of angiolymphoid hyperplasia with eosinophilia aggravated during pregnancy. Balkan Med J 2011;28:319-21.
[Google Scholar]
|
| 5. |
Haritha K, Satya S, Rao GR, Durga Prasad BK, Chowdary AP. Angiolymphoid hyperplasia with eosinophilia during pregnancy: A study of three cases with a brief review of literature. J NTR Univ Health Sci 2016;5:295-8.
[Google Scholar]
|
Fulltext Views
3,417
PDF downloads
2,356





