Translate this page into:
Refining criteria for diagnosis of cutaneous infections caused by herpes viruses through correlation of morphology with molecular pathology
2 Division of Molecular Pathology, Dermatologikum, Hamburg, Germany
Correspondence Address:
Almut B�er
Dermatologikum, Hamburg, Stephansplatz 5, 20354, Hamburg
Germany
| How to cite this article: B�er A, Herder N, Bl�dorn-Schlicht N, Steinkraus V, Falk TM. Refining criteria for diagnosis of cutaneous infections caused by herpes viruses through correlation of morphology with molecular pathology. Indian J Dermatol Venereol Leprol 2006;72:270-275 |
Abstract
BACKGROUND: Infections of the skin by herpes viruses do not always present themselves in typical fashion. Early diagnosis, however, is crucial for appropriate treatment. Polymerase chain reaction (PCR) allows diagnosis and differential diagnosis of herpes virus infections, but the method is not yet available in large parts of the world, where diagnosis is made based on morphology alone. AIM: To refine criteria for the diagnosis of herpes virus infections of the skin by way of correlation of clinical and histopathologic findings with results of PCR studies. METHODS: We studied 75 clinically diagnosed patients of "zoster," "varicella," and "herpes simplex", to correlate clinical and histopathological findings with results of PCR studies on paraffin embedded biopsy specimens. RESULTS: Clinical suspicion of infection by herpes viruses was confirmed by histopathology in 37% of the cases and by PCR studies in 65% of the cases. Zoster was frequently misdiagnosed as infection with herpes simplex viruses (30%). When diagnostic signs of herpes virus infection were encountered histopathologically, PCR confirmed the diagnosis in 94%. By way of correlation with results of PCR studies, initial lesions of herpes virus infections could be identified to have a distinctive histopathological pattern. Herpetic folliculitis appeared to be a rather common finding in zoster, it occurring in 28% of the cases. CONCLUSION: We conclude that correlation of clinical and histopathological features with results of PCR studies on one and the same paraffin embedded specimen permits identification of characteristic morphologic patterns and helps to refine criteria for diagnosis both clinically and histopathologically.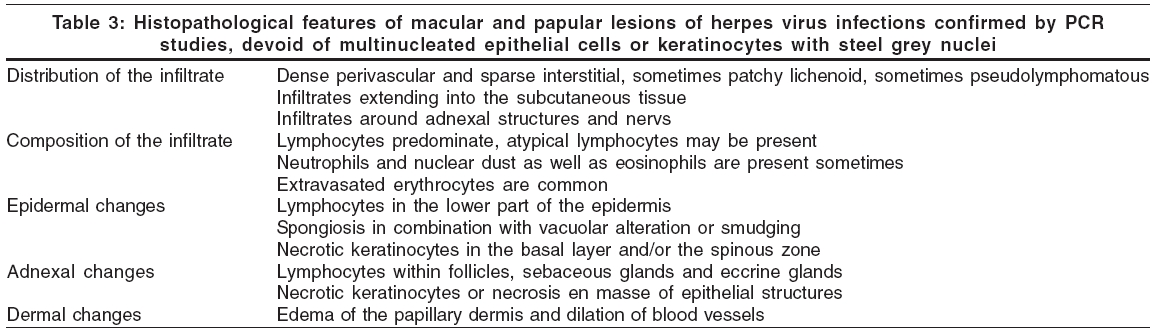
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Introduction
Infections of the skin by herpes viruses do not always present themselves in typical fashion.[1],[2],[3] Especially at the outset of an eruption, when lesions are macules, papules and plaques, diagnosis is often difficult. Conventional microscopy has been used routinely to confirm infection by herpes viruses, but sometimes, typical signs such as multinucleated epithelial cells or keratinocytes with steel grey nuclei may not be encountered in a specimen. In more recent years, the benefits of routine PCR techniques for differential diagnosis of herpetic infection has been increasingly appreciated.[2],[4],[5],[6] In large parts of the world, however, colleagues do not have access to PCR techniques and there is still a need to improve criteria for morphologic diagnosis.
Hence we undertook this study to refine criteria for diagnosis of herpes virus infections of the skin by way of correlation of clinical and histopathological findings with results of PCR studies.
METHODS
We recruited 75 patients in whom the diagnosis or differential diagnosis offered by the clinician included herpes simplex, varicella or herpes zoster and in whom a biopsy specimen was taken for confirmation, because doubts existed about the correctness of the clinical diagnosis.
We reviewed charts for descriptions of lesions and photographs (available for 41 patients) as well as sections cut from 90 biopsy specimens. Sections were assessed by two independent dermatopathologists for findings typical of herpes virus infection such as acantholysis, ballooning, reticular alteration, necrotic keratinocytes, multinucleated epithelial cells, keratinocytes with steel-grey nuclei and margination of the chromatin.
Formalin-fixed paraffin embedded tissue were studied comparatively by polymerase chain reaction (PCR) for HSV-1-, HSV-2 and varicella-zoster-specific DNA. Total DNA was isolated from paraffin-embedded tissue samples following the manufacturer′s instructions (QIAamp DNA Mini Kit; QIAGEN ®). HSV-1-, HSV-2-, and VZV- specific PCR fragments were amplified as follows: HSV-1 primers H1P32/H1M32, genomic region RL 2; HSV-2: primers H2M40/H2P4, genomic region: UL 28; VZV: primers VP22/VM20, genomic region ORF 8.[4] Paraffin blocks without tissue samples served as negative as well as cross contamination controls. In order to check the integrity of DNA sample preparations, negative PCR probes were used to amplify the anterior part (307 bp) of the human cytochrome-b gene using conserved primers L14841 and H15149.[5] To identify unambiguously all three virus types, 9 PCR products were sequenced directly (BigDye Terminator Cycle Sequencing Mix; Applied Biosystems ®). Sequences were further processed using BioEdit version 5.0.9[6] and subsequently analyzed using the NCBI BLAST search.
RESULTS
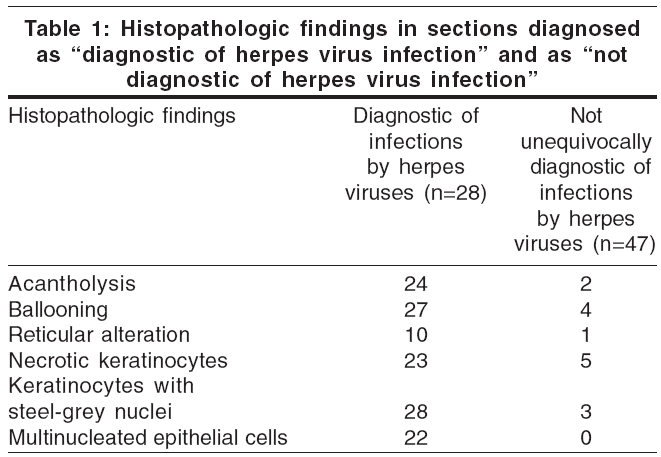
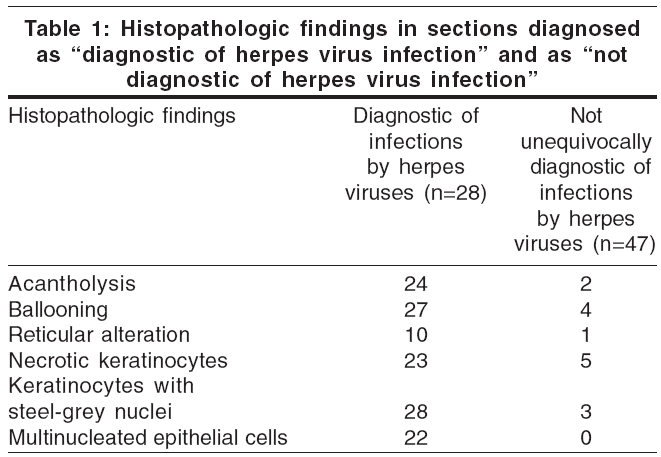
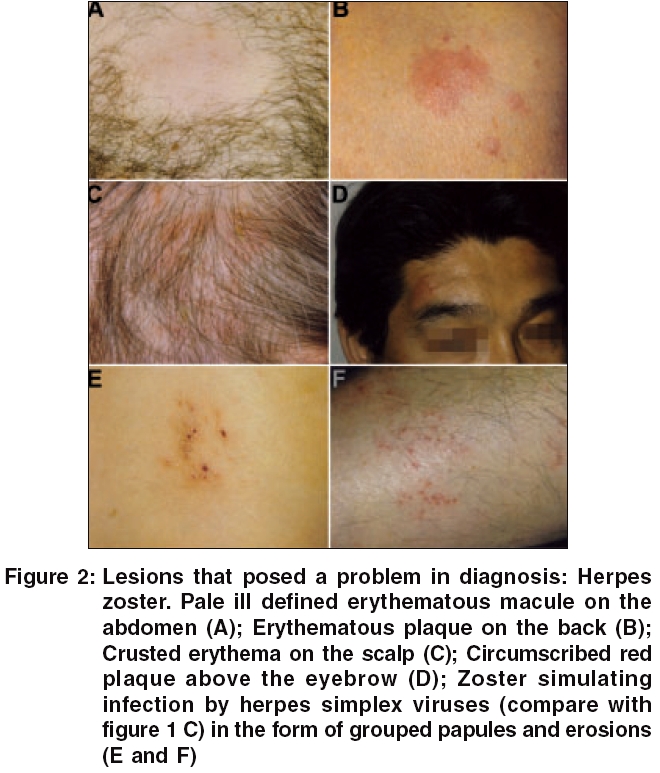
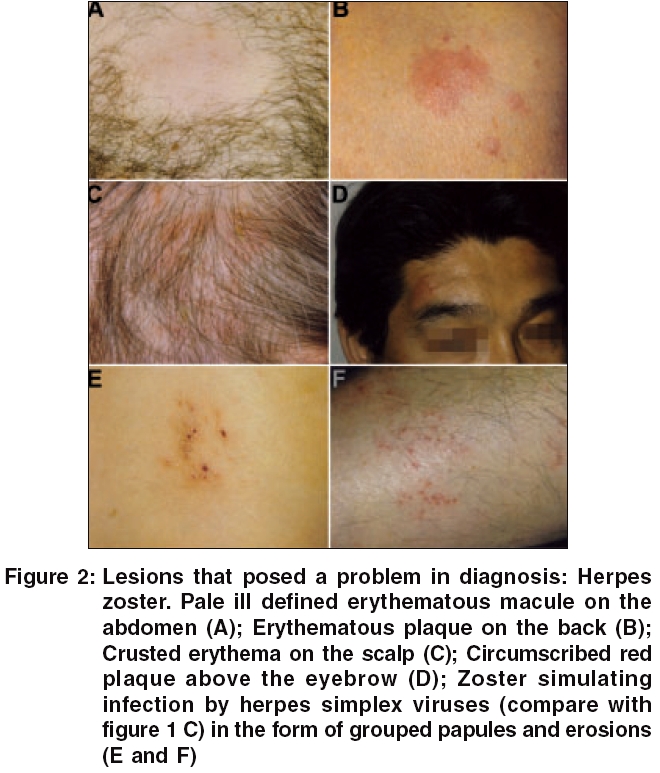
The diagnosis made by the clinician at the time of biopsy was herpes zoster in 32 patients, varicella in 4 patients and herpes simplex in 39 patients. Lesions that posed a problem in diagnosis are pictured in [Figure - 1][Figure - 2][Figure - 3]. The clinical diagnosis of infection by herpes viruses was confirmed by histopathology in only 28 patients. In 47 patients, sections were devoid of signs diagnostic of herpes virus infections. Histopathological findings are given in detail in [Table - 1].
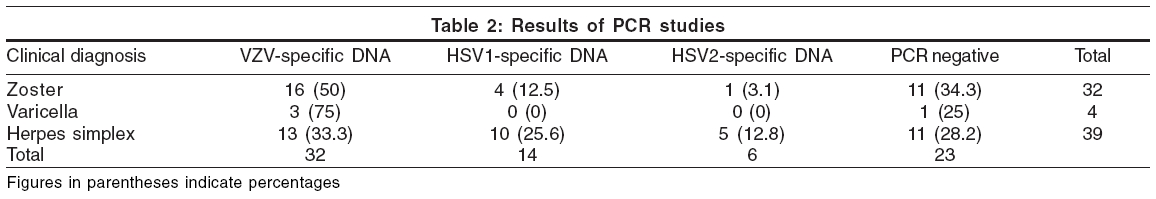
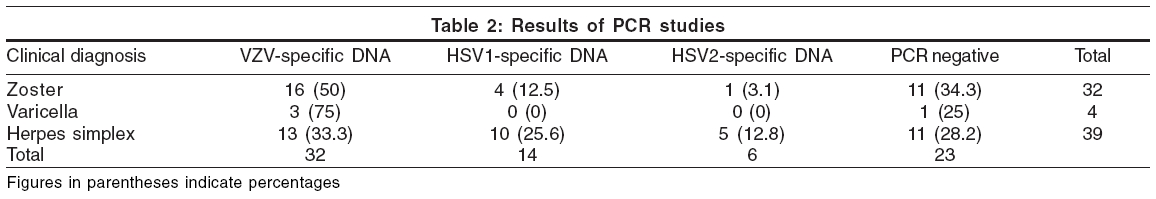
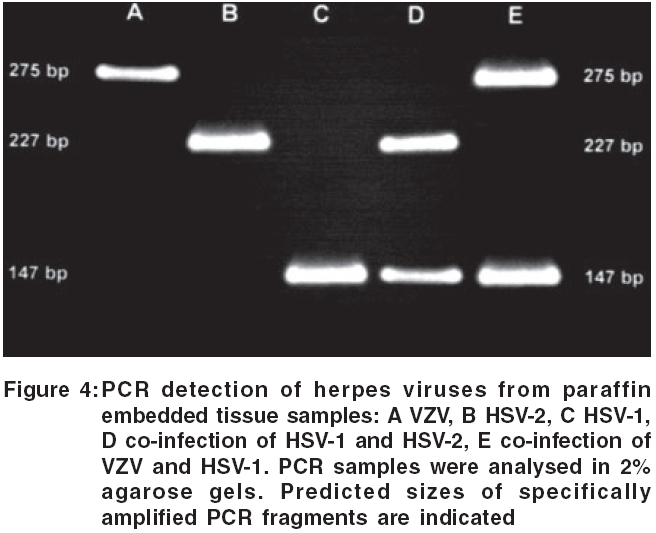
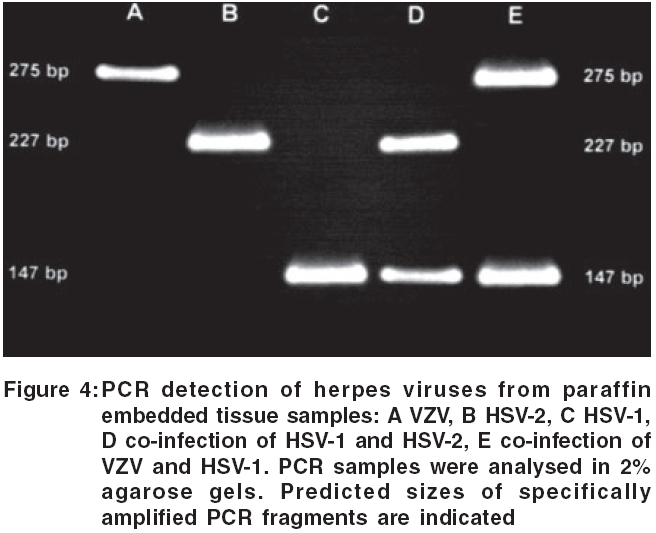
The diagnosis made by the clinician was confirmed by the results of PCR studies in 52 patients. In 13 of 39 patients who were diagnosed clinically as herpes simplex, PCR analyses revealed the presence of varicella-zoster-specific DNA. Results of PCR studies are shown in [Figure - 4] and listed in detail in [Table - 2].
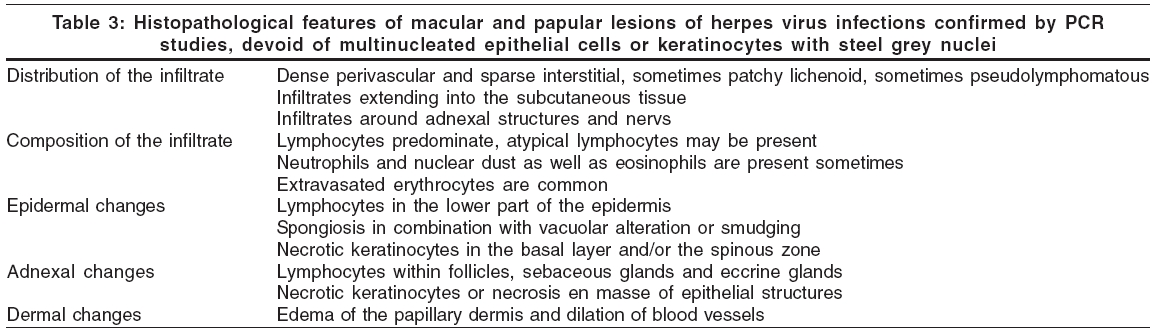
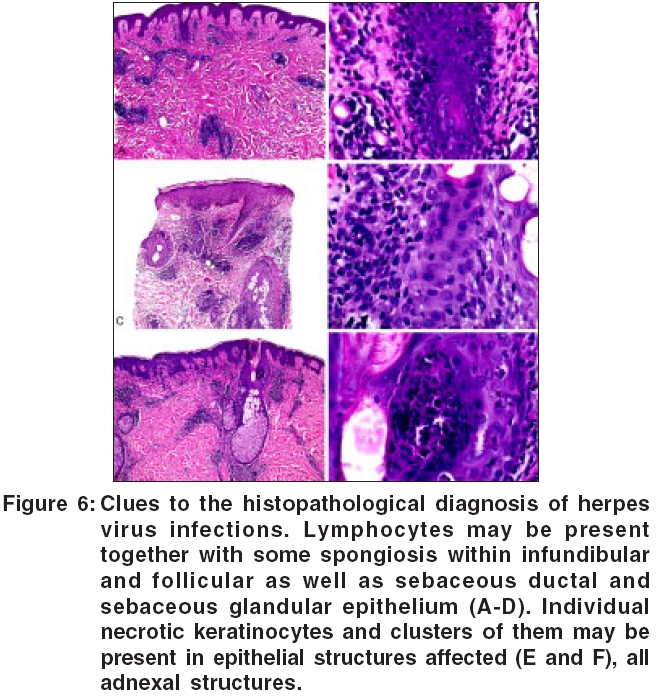
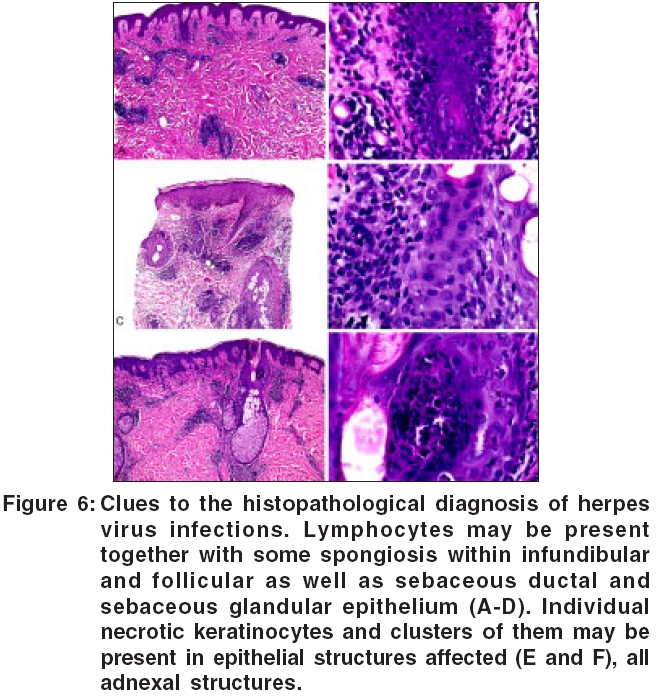
In 26 of 28 patients who had histopathological findings diagnostic of herpes virus infection, PCR was positive for herpes virus-specific DNA. In sections diagnosed as "not unequivocally diagnostic," PCR was positive for herpes virus-specific DNA in 18 cases. Twelve of these cases were very similar, the vast majority of them being VZV positive (10/12). Typical features are listed in [Table - 3]. Clues to the diagnosis histopathologic of herpes virus infections, when signs regarded to be diagnostic are absent, are pictured in [Figure - 5].
Involvement of follicular and sebaceous lobular epithelium was seen in 9 of 49 specimens, all of them being VZV positive.
DISCUSSION
Infections of the skin by herpes viruses may pose a problem in diagnosis both clinically and histopathologically.[1],[2],[3] Studies on large groups of patients about morphologic findings in herpes virus infections are rare and unusual features of herpetic infections have been published almost exclusively in the form of case reports.[1],[2],[3],[7],[8] Today, PCR studies allow diagnosis and differential diagnosis of herpes virus infections with near surety.[9],[10],[11] PCR for herpes viruses is highly sensitive and easy to perform from blister fluid or fresh as well as from paraffin-embedded biopsy specimens. It is much more reliable than immunostain or in-situ hybridization and, when established in a laboratory, even less expensive. It also enables to differentiate, with surety, between HSV I, HSV II and VZV infections.[9],[10],[11] False positive results by way of cross contamination can be prevented by negative controls being performed routinely with every second probe.
Our study demonstrates that in more than one third of all patients the clinical diagnosis of herpes virus infection was wrong and those cases were identified by both, histopathological and PCR techniques. Zoster was misdiagnosed as HSV infection in 30% of the cases. Clinicians had difficulties to make a diagnosis on clinical grounds alone when tiny vesicles were absent. Zoster was misdiagnosed frequently when lesions were macular and papular only. Incomplete segmental distribution of lesions was also responsible for zoster being misdiagnosed as HSV infection. Ulcers are often diagnosed clinically as herpes virus infections, even though they rarely are caused by those viruses.
Histopathologically, the most consistent findings of herpes virus infections are steel grey nuclei, followed by ballooning, acantholysis, multinucleated epithelial cells and necrotic keratinocytes. Findings encountered in macular and papular lesions of herpes virus infections may also be diagnosed with near surety, namely, when a superficial and deep, perivascular and periadnexal infiltrate of lymphocytes is encountered, lymphocytes also being present in epithelial structures accompanied by spongiosis combined with vacuolar alteration and a few necrotric keratinocytes. Acute onset of the eruptions is demonstrated by basket woven orthokeratosis, extravasated erythrocytes especially in the papillary dermis and edema of the papillary dermis.
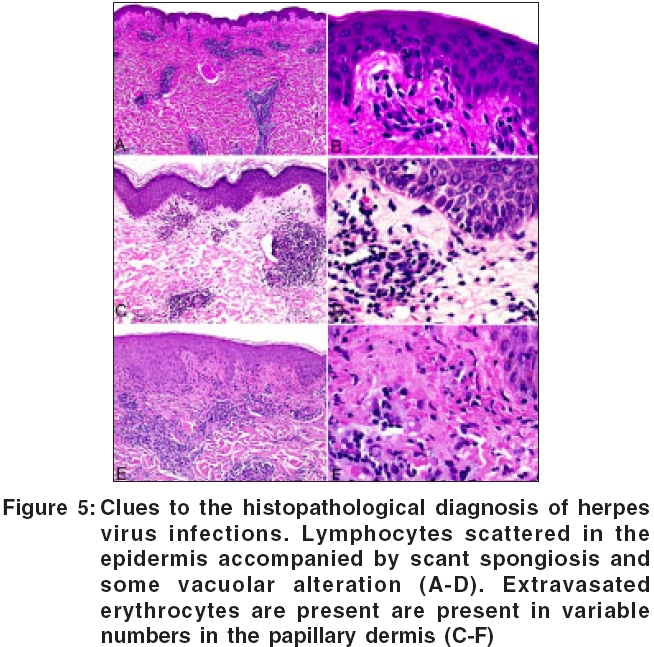
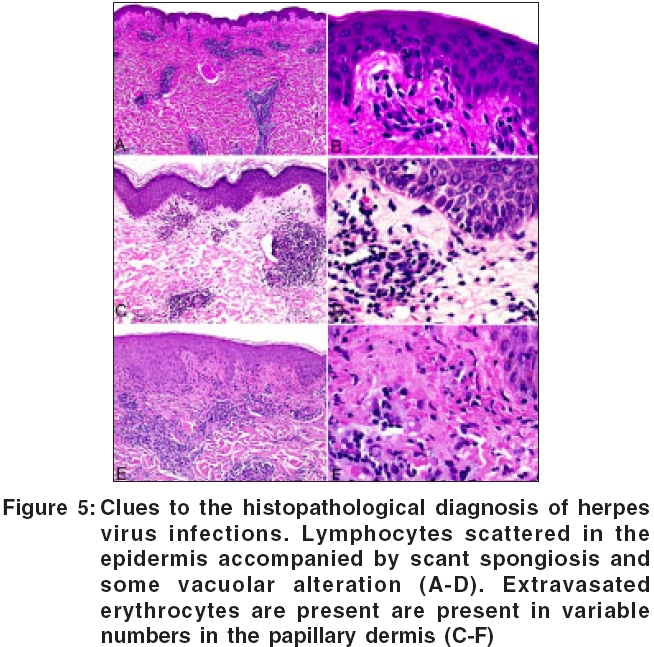
Frank herpetic folliculitis was a common finding in zoster, occurring in 28% of the cases, whereas it was not encountered in infections with herpes simplex viruses. In accordance with observations made recently by Walsh and coworkers,[12] our studies indicated that prominent involvement of follicular and sebaceous structures is seen much more commonly in varicella zoster infections than in herpes simplex virus infections.
In sum, stereotypical findings such as steel grey nuclei, ballooning, acantholysis, multinucleated epithelial cells and necrotic kerationocytes remain the most reliable histopathological criteria for diagnosis of herpetic infections. If, however, those features are lacking, a histopathologist still may be able to suspect herpetic infection with near surety when the following features are present in a section of tissue: (1) Dense perivascular and sparse interstitial infiltrates of lymphocytes and sometimes patchy lichenoid,
(2) infiltrates extending into the subcutaneous tissue, (3) lymphocytic folliculitis and perifolliculitis,
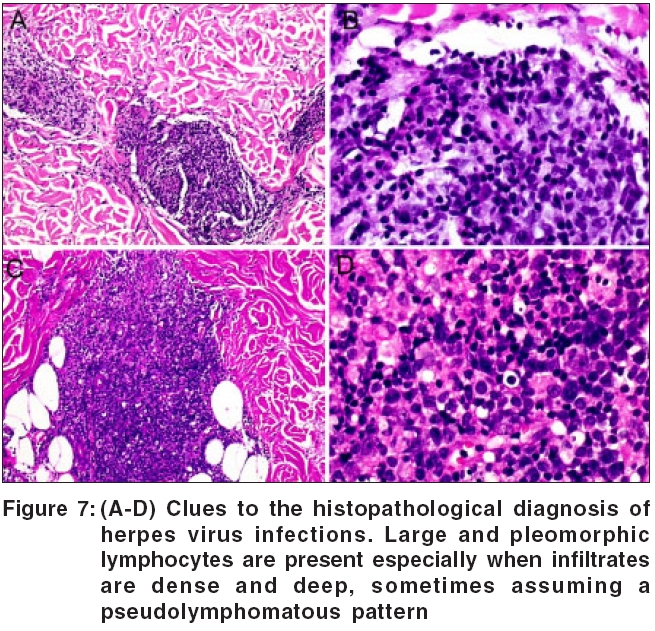
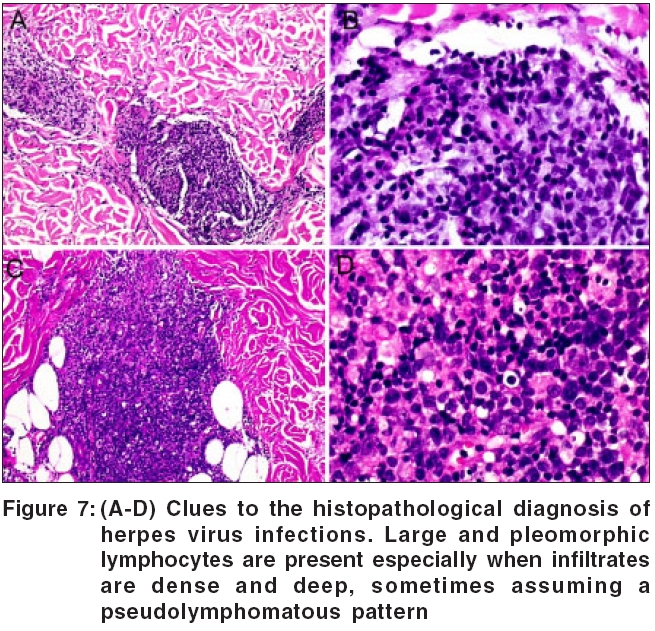
(4) lymphocytes within sebaceous glands, (5) lymphocytes within eccrine glands, (6) lymphocytes in and around nerves, (7) lymphocytes in the lower part of the epidermis, (8) spongiosis in combination with vacuolar alteration or smudging, (9) necrotic keratinocytes in the basal layer and/or the spinous zone, (10) necrotic keratinocytes in follicular epithelium, (11) edema of the papillary dermis and dilation of blood vessels, (12) extravasated erythrocytes, (13) some atypical lymphocytes in the infiltrates, (14) neutrophils and nuclear dust present in the infiltrate [Figure - 6][Figure - 7].
Diseases to be considered in the differential diagnosis of these manifestations of herpetic infections are lupus erythematosus, polymorphous light eruption, Mucha-Haberman disease, lymphomatoid papulosis, erythema migrans and, less likely, insect bite reactions or drug eruptions. The latter can be excluded because of the rarity of eosinophils in the infiltrate of herpes virus infections. Borreliosis presents with plasma cells in the infiltrate whereas herpetic infections do not, polymorphous light eruption usually presents with more pronounced spongiosis and lupus erythematosus as well as Mucha-Haberman disease with more marked vacuolar alteration than herpetic infections. The presence of mucin in abundance may also help to exclude lupus erythematosus. Exceedingly difficult may be the differentiation from lymphomatoid papulosis because herpes virus infections as well as lymphomatoid papulosis may present as lymphocytic folliculitis and perifolliculitis with atypical lymphocytes. In such cases, clinicopathological correlation and clinical follow up are indispensable for coming to a correct diagnosis.
Studies of correlation of morphology, with methods of molecular pathology deepen our knowledge about the spectrum of manifestations of diseases. They enable us to refine criteria for morphologic diagnosis and help to identify useful morphologic clues to the correct diagnosis. Especially in those parts of the world where ancillary procedures are not available and diagnosis is still made based on morphology alone, observations such as ours will help to decrease misdiagnosis of herpes virus infections.
| 1. |
LeBoit PE, Limova M, Yen TS, Palefsky JM, White CR Jr, Berger TG. Chronic verrucous varicella-zoster virus infection in patients with the acquired immunodeficiency syndrome (AIDS). Histologic and molecular biologic findings. Am J Dermatopathol 1992;14:1-7.
[Google Scholar]
|
| 2. |
Ramel F. [Herpes and skin lesions: What's new?] Pathol Biol (Paris) 2002;50:440-4.
[Google Scholar]
|
| 3. |
Resnik KS, Di Leonardo M. Herpes incognito. Am J Dermatopathol 2000;22:144-50.
[Google Scholar]
|
| 4. |
Markoulatos P, Georgopoulou A, Siafakas N, Plakokefalos E, Tzanakaki G, Kourea-Kremastinou J. Laboratory diagnosis of common herpes virus infections of the central nervous system by a multiplex PCR assay. J Clin Microbiol 2001;39:4426-32.
[Google Scholar]
|
| 5. |
Kocher TD, Thomas WK, Meyer A, Edwards SV, Pδδbo S, Villablanca FX, et al . Dynamics of mitochondrial DNA evolution in animals: Amplification and sequencing with conserved primers. Proc Nat Acad Sci USA 1989;86:6196-200.
[Google Scholar]
|
| 6. |
Hall KT, Stevenson AJ, Goodwin DJ, Gibson PC, Markham AF, Whitehouse A. The activation domain of herpes virus saimiri R protein interacts with the TATA-binding protein. J Virol 1999;73:9756-63.
[Google Scholar]
|
| 7. |
B φer A, Herder N, Bl φdorn-Schlicht N, Falk T. New observation: Herpes incognito is zoster incognito and its pattern histopathologic is distinctive! Dermatopathol Pract Conc 2005;11:4.
[Google Scholar]
|
| 8. |
Foti C, Filotico R, Calvario A, Conserva A, Antelmi A, Angelini G. Relapsing herpes simplex-2 folliculitis in the beard area. Eur J Dermatol 2004;14:421-3.
[Google Scholar]
|
| 9. |
Lilie HM, Wassilew SW, Wolff MH. Early diagnosis of herpes zoster by polymerase chain reaction. J Eur Acad Dermatol Venereol 2002;16:53-7.
[Google Scholar]
|
| 10. |
Beards G, Graham C, Pillay D. Investigation of vesicular rashes for HSV and VZV by PCR. J Med Virol 1998;54:155-7.
[Google Scholar]
|
| 11. |
Rubben A, Baron JM, Grussendorf-Conen EI. Routine detection of herpes simplex virus and varicella zoster virus by polymerase chain reaction reveals that initial herpes zoster is frequently misdiagnosed as herpes simplex. Br J Dermatol 1997;137:259-61.
[Google Scholar]
|
| 12. |
Walsh N, Boutilier R, Shaffelburg M. Exclusive involvement of folliculosebaceous units by herpes: A reflection of early herpes zoster. Am J Dermatopathol 2005;27:189-94.
[Google Scholar]
|
Fulltext Views
8,181
PDF downloads
2,337





