Translate this page into:
REM syndrome
2 Department of Pathology, Dr. R.P. Govt. Medical College, Kangra (Tanda)-176 001, Himachal Pradesh, India
Correspondence Address:
Vikram K Mahajan
Department of Dermatology, Venereology and Leprosy, Dr. R.P. Govt. Medical College, Kangra (Tanda)-176 001, Himachal Pradesh
India
| How to cite this article: Mahajan VK, Sharma S, Sharma NL. REM syndrome. Indian J Dermatol Venereol Leprol 2011;77:188-189 |
A 51-years-old, HIV-negative male presented with asymptomatic, progressive, net-like erythema over neck of three years duration. Cutaneous examination showed reticular erythematous, minimally infiltrated lesions with isolated fine telangiectasias involving the sides and front of the neck and over suprasternal area [Figure - 1]. They blanched incompletely on pressure. The face and extremities were spared. The patient was a forester working outdoors in the sun for long hours. There was no history of prior drug intake. Systemic/ophthalmic examination and laboratory investigations including complete blood counts, serum biochemistry, antinuclear antibodies, thyroid functions, serum electrophoresis, urinalysis, chest X-ray and abdominal ultrasonography were essentially normal. Histology [Figure - 2] showed thin flattened epidermis, few dilated vessels and minimal perivascular mononuclear cell infiltrate comprising lymphocytes and few hystiocytes, separation of dermal collagen bundles with homogenous material in the upper and mid dermis that stained positive for mucin with alcian blue. Direct immunofluorescence test was not performed due to expense. With the diagnosis of REM syndrome, he was advised to avoid undue sun exposure and prescribed hydroxychloroquine 200 mg twice daily. A recent follow up revealed that the lesions had resolved completely about two months after this treatment.
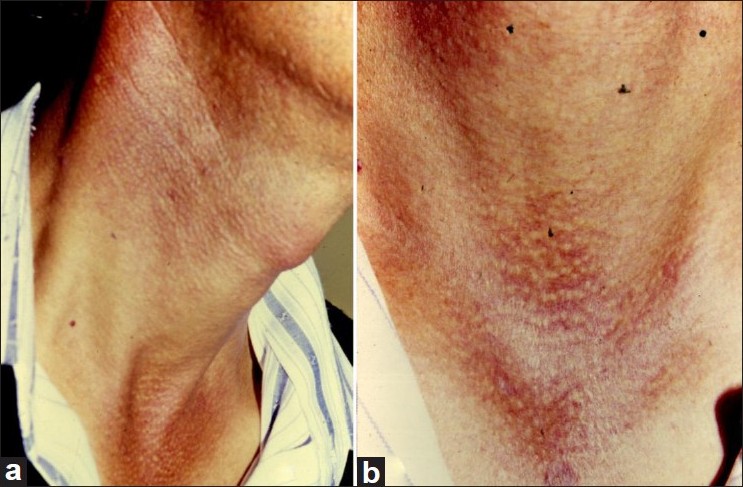 |
| Figure 1: (a) Reticulate erythema with minimal infiltration and isolated fine telangiectasias over the sides and front of the neck, and suprasternal area. (b) Close-up view of reticulate erythema, isolated telangiectasias and mucinous flesh colored papular lesions in suprasternal area. The black spots are artifacts |
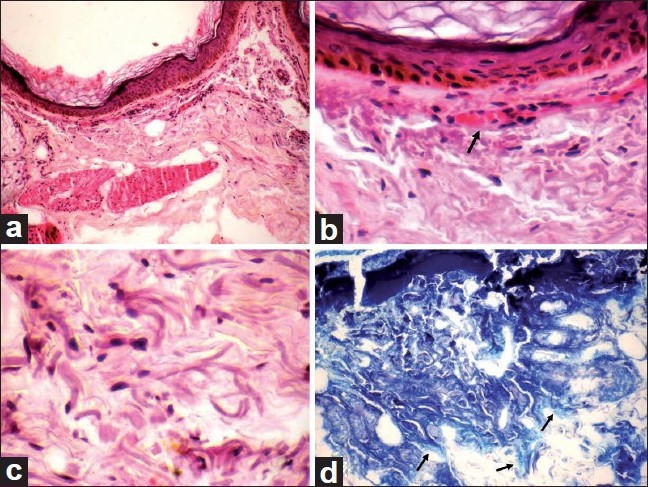 |
| Figure 2: (a) Thin flattened epidermis, separated collagen bundles and minimal cellular infiltrate (H and E, �4). (b) Dilated vessels (arrow), minimal perivascular mononuclear cell infiltrate comprising lymphocytes and few hystiocytes (H and E, ×10 ). (c) Fenestrations in the dermal collagen bundles (H and E, ×40). (d) Arrows indicate homogenously stained mucin in the upper and mid dermis (Alcian blue, ×40) |
REM syndrome, also known as reticular erythematous mucinosis or plaque-like cutaneous mucinosis, is a rare disorder that affects patients of all ages and both sexes but described cases have been mostly middle-aged females. The characteristic asymptomatic reticulate erythematous lesion, sometimes with minimally infiltrated papules and telangiectasias, symmetrically involves the central part of the chest particularly the sternum, neck, upper back and, rarely breasts and abdomen. Pruritus or involvement of face and limbs is extremely rare. Characteristic histologic features include perivascular or perifollicular mononuclear cell infiltrate and increased dermal mucin deposition while direct immunofluorescence is variable. Its etiology is unknown, but evidently sunlight is an important factor in its pathogenesis. Its relation with lupus erythematosus-like disease spectrum is unclear; both share features of photo-aggravation, few clinico-pathologic characters and good response to antimalarial drugs. The co-existing diseases like hyper-/hypothyroidism, Hashimoto′s disease, discoid lupus erythematosus and diabetes mellitus indicate that it is perhaps a disorder of immune regulation. Other occasional associations include myopathy, polyneuropathy, breast and colon cancers, thrombocytopenic purpura, use of anovulatory drugs, paraproteinemia, uveitis and HIV infection. Topical steroids are not useful, but antimalarials are almost invariably effective. More recently, pulsed-dye laser, UV-A1 radiation, topical pimecrolimus or tacrolimus, alone or in combination, have been used successfully. Sun protection can be advocated to prevent progression.
Fulltext Views
5,275
PDF downloads
4,154





