Translate this page into:
Retrospective study of spectrum of cutaneous lymphoma presenting to dermatology
Correspondence Address:
Bhavana R Doshi
C/O Uday Khopkar, Department of Dermatology, Seth G. S. Medical College and K. E. M. Hospital, Parel, Mumbai - 400 012
India
| How to cite this article: Doshi BR, Khopkar US. Retrospective study of spectrum of cutaneous lymphoma presenting to dermatology. Indian J Dermatol Venereol Leprol 2011;77:512-515 |
Sir,
Skin is the second most common extranodal site of lymphoma after the gastrointestinal tract. Primary cutaneous lymphoma refers to those cutaneous T-cell lymphomas (CTCLs) and cutaneous B-cell lymphomas (CBCLs) that present in the skin with no evidence of extracutaneous disease at the time of diagnosis. Incidence of primary cutaneous lymphoma has been estimated to be 1:100,000 according to the WHO. [1] Cutaneous lymphomas clinically present as patches, plaques, papules, and nodules along with histologically distinct features.
Till date, there is not much data available on the epidemiology of cutaneous lymphomas in India since the majority of cases of cutaneous lymphomas have been published as case reports. Hence, we decided to undertake this study to determine the epidemiological profile of cutaneous lymphomas in our tertiary care institute which is also a dermatopathology referral center.
A retrospective analysis of the histopathological records of 20,130 biopsies seen in the dermatopathology referral practice, over a 5-year period ranging from January 2004 to December 2008 was done, of which 141 cases were diagnosed as primary cutaneous lymphomas as per the European Organization for the Research and Treatment of Cancer (EORTC) and WHO classification. [2] The histopathology specimens were routine hematoxylin and eosin stained biopsy sections. Clinicopathological co-relation was done whenever patients were available. Patients of all ages with primary cutaneous lymphoma diagnosed clinically and histopathologically were included. All cases with doubtful diagnosis and those of systemic lymphoma with cutaneous involvement were excluded from the study. Immunophenotyping of the biopsy specimen was done whenever possible due to resource constraints.
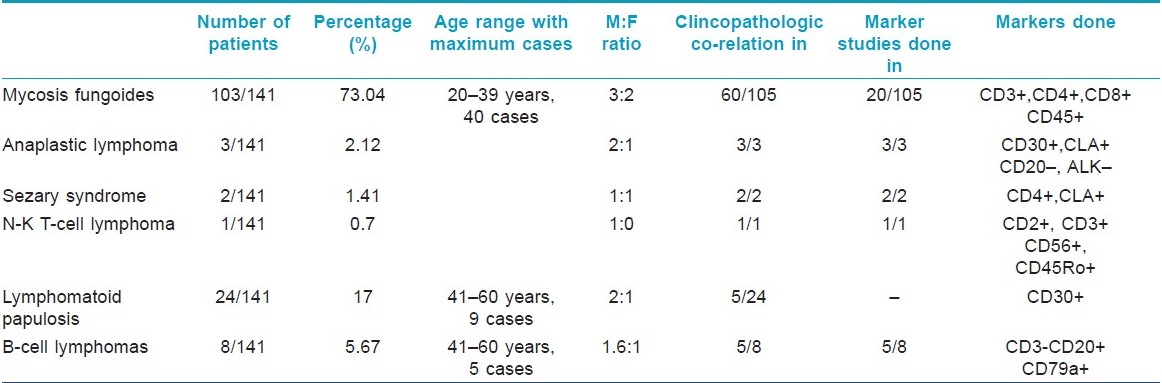
The frequency of occurrence of cutaneous lymphomas was found to be 0.7 per 100 biopsy specimens. (141/20,130). Total number of patients analyzed in this study were 141, which constituted 90 males (63.82%) and 51 females (36.17%). The male-to-female ratio was 1.76:1. The spectrum of cases which presented to us is enlisted in [Table - 1]. There were (133/141) 94.32% of patients with T-cell lymphoma of which mycosis fungoides [Figure - 1] was the most common cutaneous lymphoma constituting (103/141) 73.04% of cases.
 |
| Figure 1: Multiple ill-defined hypopigmented patches of mycosis fungoides over the arm along with classic erythematous plaque of mycosis fungoides. Biopsy from an erythematous plaque shows psoriasiform hyperplasia and collection of atypical epidermotropic lymphocytes forming Pautrier's microabscess (H and E, ×10) |
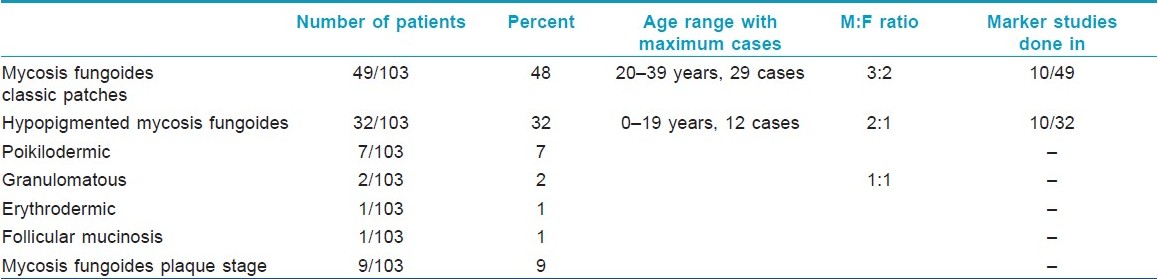
In the mycosis fungoides group, of the total 103 cases, the age of distribution ranged from 7 years to 81 years. The most common age group of involvement in patients with mycosis fungoides, excluding the hypopigmented variant was 20-39 years, constituting 29 cases, followed by 22 patients in the age range of 40-59 years. The most common age group of involvement among patients with hypopigmented variant was 0-19 years, constituting 12/32 patients, followed by 11/32 patients in the 20-39 years age group. The clinical spectrum of mycosis fungoides is highlighted in [Table - 2]. Immunohistochemistry revealed a predominant CD4+ epidermotropic atypical lymphocytic infiltrate in 10 cases having classic patches of mycosis fungoides. Out of the 10 patients of hypopigmented mycosis fungoides in whom immunohistochemistry was done, 80% (8/10) patients showed a predominant CD8+ lymphocytic epidermotropic infiltrate versus CD4+ epidermotropic infiltrate. Two patients who had both classic as well as hypopigmented patches showed the absence of both CD4+ as well as CD8+ epidermotropic infiltrate. Sιzary syndrome was observed in 2/141 cases with positive marker studies in both the cases.
Lymphomatoid papulosis was found in (24/141) 17% of patients. The age of patients ranged between 10 and 67 years. The commonest age group of involvement was between 40 and 59 years seen in 10 cases and (3/141) 2.12% of cases of anaplastic large T-cell lymphoma (ALCL) [Figure - 2] were seen. A single rare case of NK-T-cell lymphoma (0.7%) was also seen.
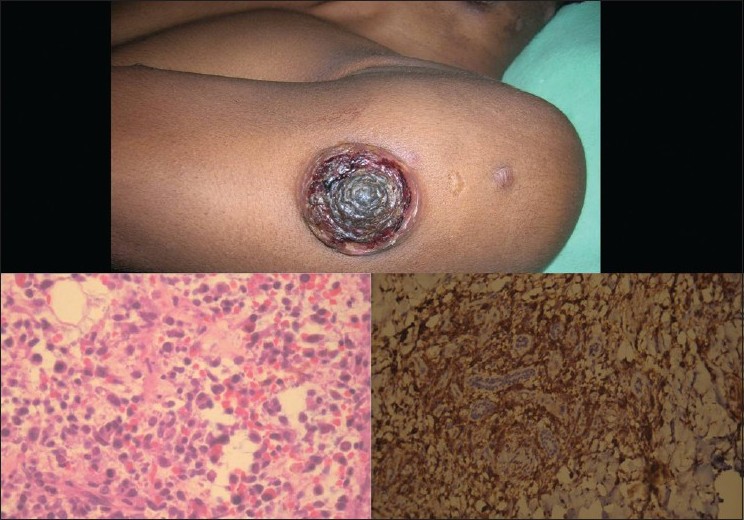 |
| Figure 2: Erythematous noduloulcerative lesion in a case of primary large anaplastic T-cell lymphoma. Biopsy showing diffuse infiltrate by large atypical lymphocytes and plasma cells in a case of anaplastic large T-cell lymphoma (H and E, ×40) along with CD30 positive cells staining brown on immunohistochemistry (H and E, ×20) |
Cutaneous B-cell lymphoma (CBCL) constituted (8/141) 5.67% of the total cases with marker studies done in 5/8 cases. Of the 8 cases, 6 were males and 2 were females. The male-to-female ratio was 3:1 with age of patients ranging from 30 to 66 years. The common age group of involvement was in the age range of 40-59 years with four cases.
Not many studies have been done on the epidemiology of cutaneous lymphoma in India except for the study done by George et al.,[2] in 33 cases seen over a 10-year period. In our study, we found the frequency of occurrence of mycosis fungoides to be 73%, much higher than the WHO [1] estimate of 44% and that of 51.6% seen in the Indian study by George et al.[2] The incidence of primary cutaneous anaplastic large cell lymphoma seen in 2.1% of cases in our study was nearly similar to that observed by George et al., [2] in 3.2% cases as compared to the 8% estimate projected by the WHO. Sιzary syndrome was seen at a much lower rate of occurrence (1.4%) with respect to the 3% estimate by the WHO and 3.2% by George et al.[2]
A much lower rate of occurrence of B-cell lymphoma (5.6%) was seen in our study, whereas the WHO and the study by George et al. [2] estimated its occurrence to be around 25% and 22.5%, respectively. Lymphomatoid papulosis was seen in 17% in our study which was not mentioned in the study by George et al.[2] However, the findings of our study are not comparable since they used the REAL system of classification which does not include lymphomatoid papulosis.
Clinicopathological co-relation plays an important role in the early detection of lymphomas. This study highlights that T-cell lymphomas are the commonest lymphomas affecting the skin of which mycosis fungoides is the most common lymphoma. Hypopigmented mycosis fungoides which is commonly reported in young dark skin individuals was found to be the newly emerging variant of MF in (32/103) 32% of patients with a predominant CD8+ epidermotropic atypical lymphocytic infiltrate. [3] It is seen to have an increased incidence in the Indian population in the recent years with the common age group involved being the first and second decades in 36% of the cases.
The EORTC classification has an edge over REAL classification [4] since it includes lymphomatoid papulosis along with myeloid and histiocytic neoplasms. A strict follow-up of patients of lymphomatoid papulosis is required considering its potential to evolve into MF/ALCL in 15-20% of cases. [5],[6]
To conclude, since our study was a retrospective study it has its limitations in that what is seen in the laboratory may not be the true incidence in clinical practice. Hence we feel that there is a need for a prospective study with a larger sample size and long-term follow-up to determine the exact epidemiological trends and disease outcome in our country and immunophenotyping should be done for further classifying lymphomas whenever possible for prognostic implications.
Acknowledgement
The authors like to thank Dr Sumeet Gujral, Associate Professor, Department of Pathology, Tata Memorial Hospital, Mumbai for review of the biopsy sections and Mr Sanjay Jagdale, technician at Tata Memorial Hospital, Mumbai for immunohistochemistry on the biopsy sections.
| 1. |
Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-85.
[Google Scholar]
|
| 2. |
George R, Bhuvana S, Nair S, Lakshmanan J. Clinicopathological profile of cutaneous lymphomas-A 10 year retrospective study from south India. Indian J Cancer 1999;36:109-19.
[Google Scholar]
|
| 3. |
El Shabrawi-Caelen L, Cerroni L, Medeiros LJ, McCalmont TH. Hypopigmented mycosis fungoides: Frequent expression of a CD8+ T-cell phenotype. Am J Surg Pathol 2002;26:450-7.
[Google Scholar]
|
| 4. |
Willemze R, Kerl H, Sterry W, Berti E, Cerroni L, Chimenti S, et al. EORTC classification for primary cutaneous lymphomas: A proposal from the Cutaneous Lymphoma Study Group of the European Organization for Research and Treatment of Cancer. Blood 1997;90:354-71.
[Google Scholar]
|
| 5. |
Sanchez NP, Pittelkow MR, Muller SA, Bank PM, Winkelmann RK. The clinicopathologic spectrum of lymphomatoid papulosis: Study of 31 cases. J Am Acad Dermatol 1983;8:81-94.
[Google Scholar]
|
| 6. |
Brehmer-Andersson E. Mycosis fungoides and its relation to Sezary's syndrome, lymphomatoid papulosis, and primary cutaneous Hodgkin's disease. A clinical, histopathologic and cytologic study of fourteen cases and a critical review of the literature. Acta Derm Venereol Suppl (Stockh) 1976;56:3-142.
[Google Scholar]
|
Fulltext Views
3,077
PDF downloads
1,497





