Translate this page into:
Role of occasional evaluation of the skin in early detection of melanoma in elderly patients
Correspondence Address:
Ausilia Maria Manganoni
Department of Dermatology, University Hospital Spedali Civili, P.le Spedali Civili 1, 25123 Brescia
Italy
| How to cite this article: Manganoni AM, Pavoni L, Sereni E, Farisoglio C, Calzavara-Pinton P. Role of occasional evaluation of the skin in early detection of melanoma in elderly patients. Indian J Dermatol Venereol Leprol 2012;78:664 |
Sir,
Life expectancy has almost doubled over the last century in most industrialized countries and this correlates with an increase in the number of the elderly, defined as individuals aged ≥65. Although the incidence of cutaneous malignant melanoma (CMM) in the younger population appears to be levelling off or decreasing, over the coming decades the number of cases in the elderly will probably continue to rise. [1]
In this study, we sought to evaluate the incidence trend and clinical-histopathological features in different classes of age among CMM patients. Information for the study was obtained from the database owned by the Dermato-Oncologic unit of Spedali Civili of Brescia, Italy. We included data for all patients presenting between January 1980 and July 2011. Patients were divided into two main groups by age (< 65 and ≥ 65). In addition, a further subgroup aged ≥ 80 (called "The very elderly") was identified among ≥ 65. The age and the sex of patients, location of primary tumour, CMM thickness and histological type were recorded. Lesion characteristics were compared by age using the Chi Square analysis and t-Test. A significance level of 0.05 was used for all analysis. Finally, we investigated with linear regression the mean age at CMM diagnosis during the 80s, the 90s and the last ten years at our Unit.
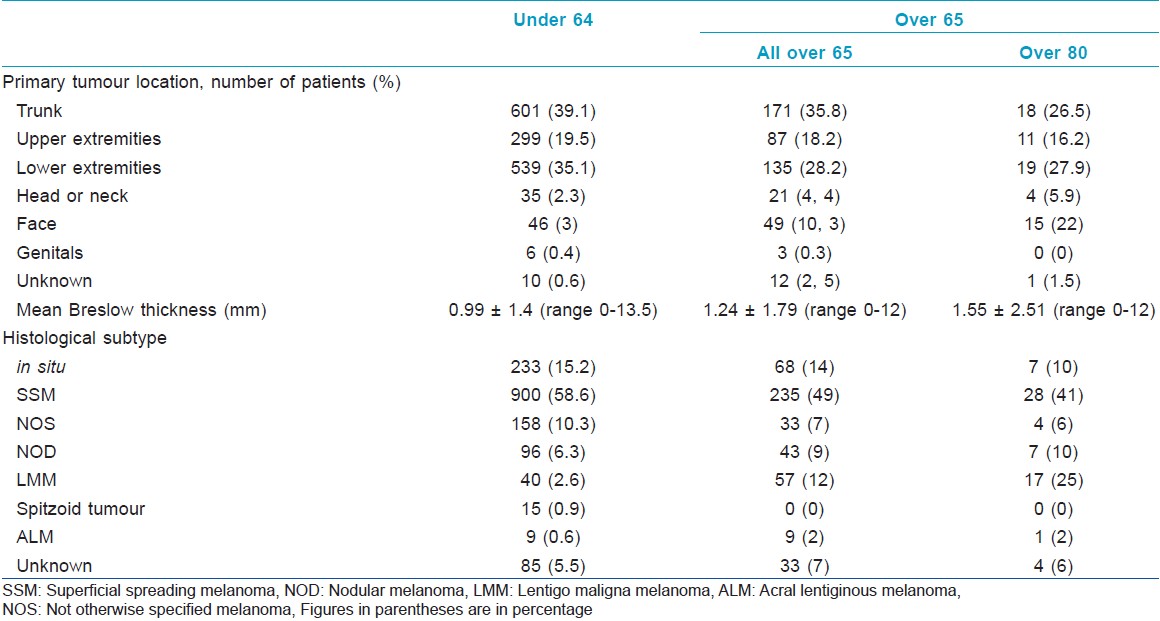
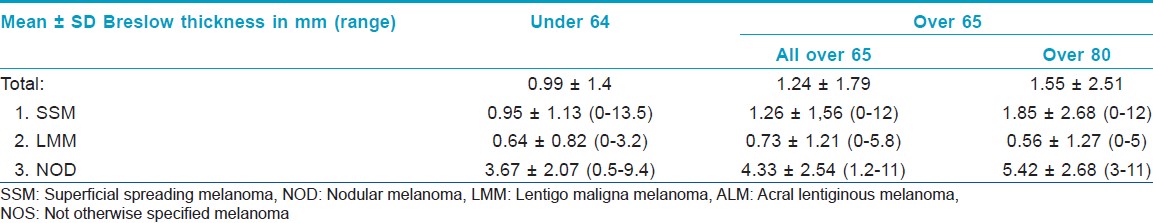
The database included records for 2014 melanoma patients, who comprised 934 men (46%) and 1080 women (54%). The mean age was 50.5 (range 9-94) and patients were followed average 62 months (range 0-348). In about 1536 patients (76%) were aged < 65 years: 678 were males (44%) and 858 females (56%). 478 patients (24%) were aged ≥ 65, 256 were males (54%) and 222 (46%) females. In which, 69 of the elderly (14.43%) were ≥ 80 (3.25% of all patients): 30 were males (43%) and 39 females (57%). [Table - 1] shows that patients aged ≥ 65 were significantly more likely to present with thick lesions than younger patients. CMM was most often found on the trunk of all patients. The incidence of CMM on the arms, leg and genitals was similar for < 65 and ≥65. CMM on the scalp, neck and most of all the face was significantly more common in ≥65 and particularly in the ≥80. Superficial spreading melanoma (SSM) was significantly more common in younger patients, while nodular melanoma (NOD) and Lentigo maligna melanoma (LMM) were more common in older. Thicknesses of the three histological types were similar in the three classes of age [Table - 2].
In the decade 1980-1989, the mean age at melanoma diagnosis was 47.5 ± 18.58 and the 26% of patients were elder. In the decade 1990-1999, the mean age was 49.12 ± 16.91 and the elderly were 19% of patients. From 2000 to 2011 the elderly were 27%, and linear regression analysis showed a marginally significant increase in the mean ages at CMM diagnosis [Figure - 1].
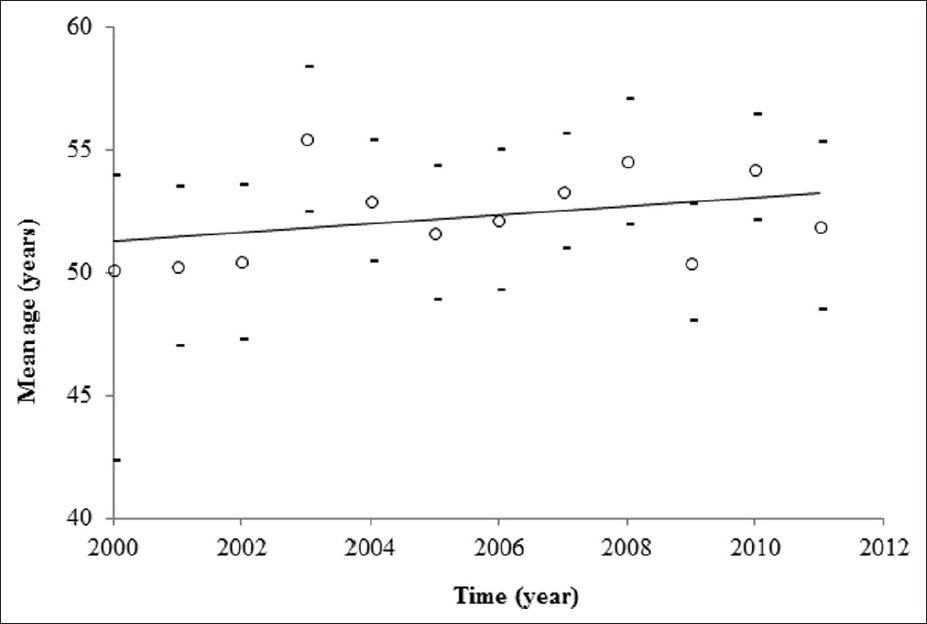 |
| Figure 1: Mean age at melanoma diagnosis from 2000 to 2011 |
Previous studies have shown a link between age and the main prognostic factors, such as Breslow thickness, Clark level, ulceration, mitotic activity, and regression. [2],[3] In our study, the most common histological type was SSM in both younger and older patients, occurring commonly on intermittently sun-exposed skin. Elderly patients were characterized by a higher proportion of LMM, which typically appeared on long-term sun-exposed areas, and of NOD: age and NOD were strongly associated with presentation of thick lesion, because NOD frequently occurred as a rapidly growing, exophytic nodule. [4] In addition, older people are often less observant to changes on their skin: this is probably due to deteriorated vision, low awareness of CMM risk, minor possibility of access to medical specialists, social isolation, depression, or co-morbidities and fraility. [2] Although in our study an increase in Breslow thickness in elderly patients, and especially in the subgroup of the very elderly, was identified, it was lower than reported in the literature. Therefore, we can assume that in our district the collaboration between the general practitioner and dermatologist is still able to guarantee an "early" diagnosis. In fact, we would suggest that the occasional total skin evaluation during a routine medical care could have an important impact on the suspicion of melanoma in elderly patients, and particularly in the very elderly, who are more likely to have multiple physician visits for other comorbidities. An accurate knowledge of the disease manifestation in this class of age would lead to a wider recognition and appropriate treatments.
| 1. |
Tsai S, Balch C, Lange J. Epidemiology and treatment of melanoma in elderly patients. Nat Rev Clin Oncol 2010;7:148- 52.
[Google Scholar]
|
| 2. |
Lasithiotakis K, Leiter U, Meier F, Eigentler T, Metzler G, Moehrle M, et al. Age and gender are significant independent predictors of survival in primary cutaneous melanoma. Cancer 2008;112:1795-804.
[Google Scholar]
|
| 3. |
Piérard-Franchimont C, Piérard GE. Melanoma of older subjects. Rev Med Liege 2011;66:34-40.
[Google Scholar]
|
| 4. |
Manganoni AM, Farisoglio C, Gavazzoni F, Facchetti F, Zanotti F, Calzavara-Pinton P. Nodular melanomas associated with nevi. J Am Acad Dermatol 2010;63:e97.
[Google Scholar]
|
Fulltext Views
1,269
PDF downloads
2,547





