Translate this page into:
Scaly erythematous plaque on the chest
2 Department of Pathology, KMC, Manipal, India
Correspondence Address:
Vandana Mehta Rai
Department of Skin and STD, Kasturba Medical College, Manipal - 576 104, Karnataka
India
| How to cite this article: Rai VM, Balachandran C, Bhat S, Geetha V. Scaly erythematous plaque on the chest. Indian J Dermatol Venereol Leprol 2007;73:447-448 |
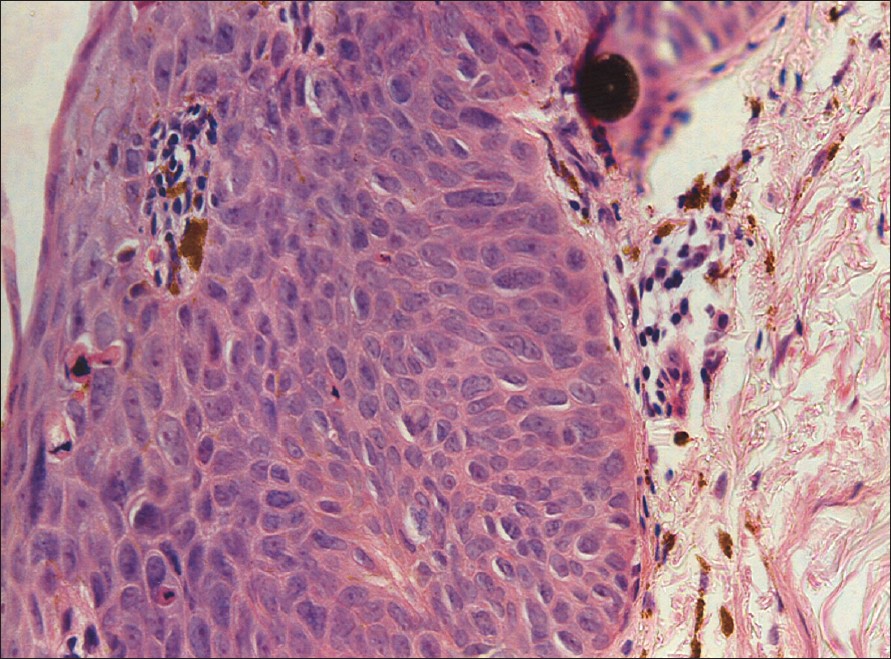 |
| Figure 4: Skin biopsy (H and E stain, X400) |
 |
| Figure 4: Skin biopsy (H and E stain, X400) |
 |
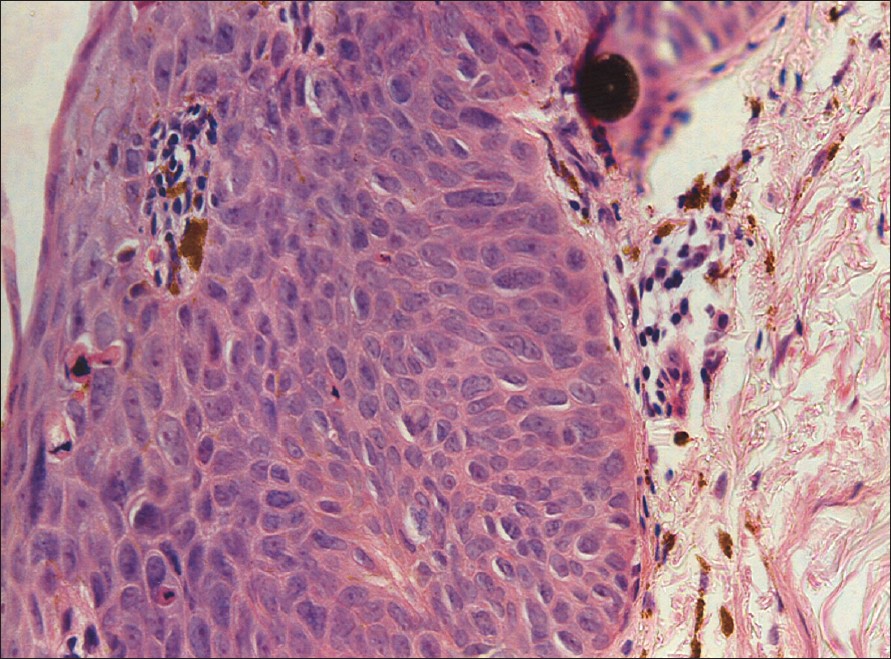
| Figure 3: Skin biopsy (H and E stain, X200) |
 |
| Figure 3: Skin biopsy (H and E stain, X200) |
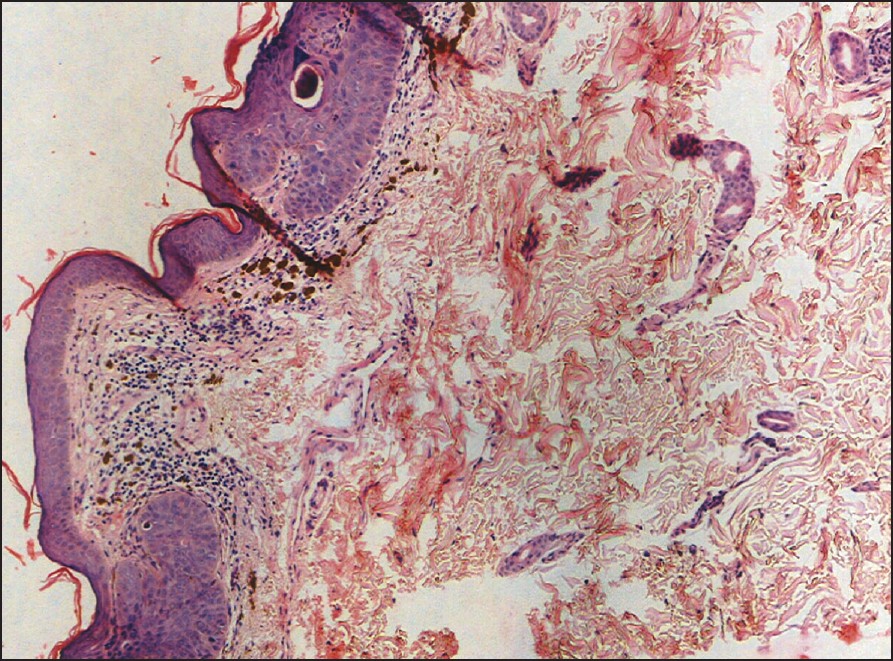 |
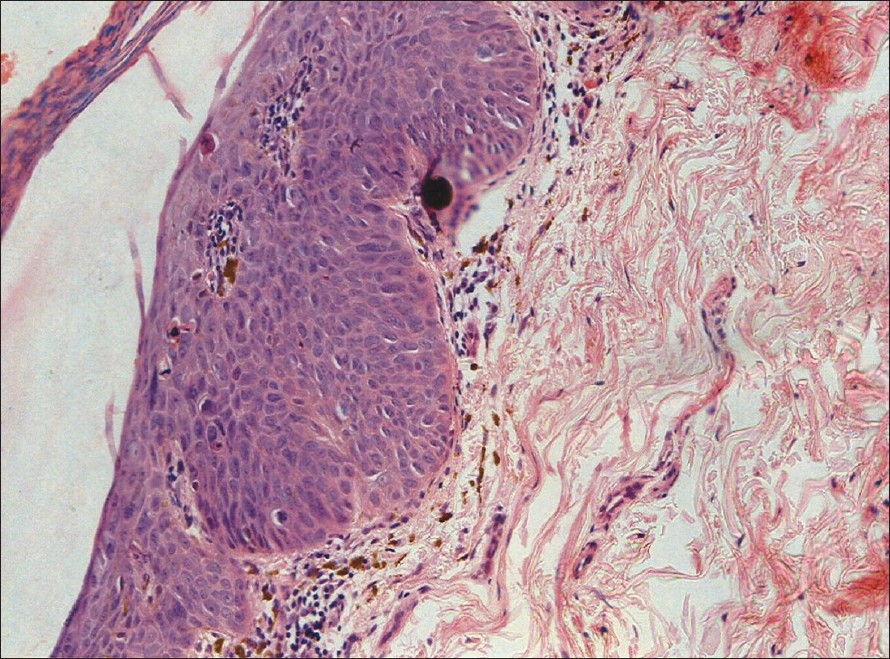
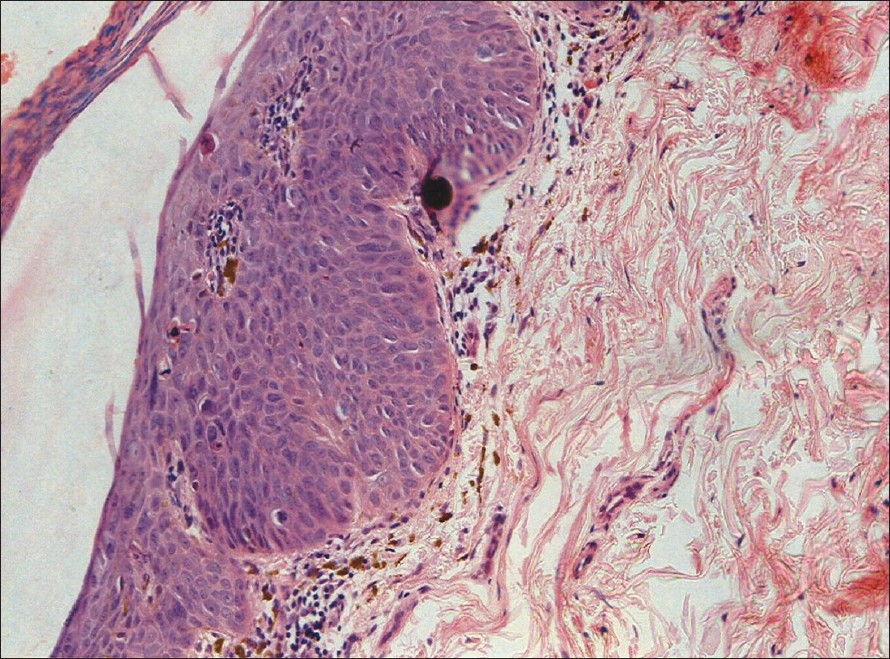
| Figure 2: Skin biopsy (H and E stain, X100) |
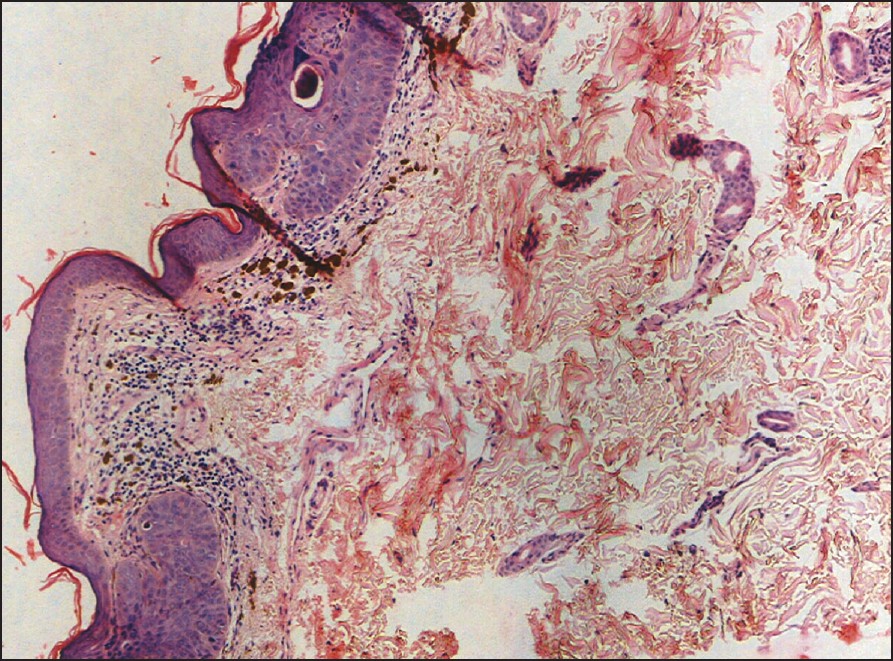 |
| Figure 2: Skin biopsy (H and E stain, X100) |
 |
| Figure 1: Scaly erythematous plaque on the chest |
 |
| Figure 1: Scaly erythematous plaque on the chest |
A 55 year-old male presented to us with an asymptomatic plaque on the chest of a year′s duration. There was a history of excessive exposure to the sun as he was a field worker but there was no history of contact with insecticides, pesticides or fertilizers. There was no similar lesion elsewhere on the body. The patient had been treated by a local physician with topical steroids for the past one year without any improvement. Cutaneous examination revealed a 3 x 3 cm well-marginated, erythematous, mildly scaly plaque on the V area of the neck [Figure - 1]. Biopsy performed from the lesion showed an irregularly acanthotic epidermis with mild nuclear pleomorphism, loss of normal architecture, scattered dyskeratotic keratinocytes, multinucleated giant cells with a lichenoid lymphoplasmacytic infiltrate [Figure - 2],[Figure - 3],[Figure - 4].
What is your Diagnosis ?
| 1. |
Kossard S, Rosen R. Cutaneous Bowen's disease: An analysis of 1001 cases according to age, sex and site. J Am Acad Dermatol 1992;27:406-10.
[Google Scholar]
|
| 2. |
Yeh S, How SW, Lin CS. Arsenical cancer of skin. Histologic study with special reference to Bowen's disease. Cancer 1968;21:312-39.
[Google Scholar]
|
| 3. |
McGrae JD Jr, Greer CE, Manos MM. Multiple Bowen's disease of the fingers associated with Human papilloma virus type 6. Int J Dermatol 1993;32:104-7.
[Google Scholar]
|
| 4. |
Patel GK, Goodwin R, Chawla M, Laidler P, Price PE, Finlay AY, Motley RJ. Imiquimod 5% cream monotherapy for cutaneous squamous cell carcinoma in situ (Bowen's disease): A randomised double blind placebo controlled trial. J Am Acad Dermatol 2006;54:1025-32.
[Google Scholar]
|
| 5. |
Clayton TH, Tait J, Whitehurst C, Yats VM. Photodynamic therapy for superficial basal cell carcinoma and Bowen's disease. Eur J Dermatol 2006;16:39-41.
[Google Scholar]
|
Fulltext Views
3,449
PDF downloads
3,986






