Translate this page into:
Scar examination in sporotrichosis: An additional tool for clinical diagnosis
2 Infection Disease Clinical Research Laboratory, Evandro Chagas Infectious National Institute, Oswaldo Cruz Foundation (FIOCRUZ), Rio de Janeiro, Brazil
3 Leishmaniasis Surveillance Laboratory (Lab Vigileish), Rio de Janeiro, Brazil
4 Department of Dermatology, Military Central Hospital (HCE), Rio de Janeiro, Brazil
5 Leishmaniasis Surveillance Laboratory (Lab Vigileish), Rio de Janeiro; Researcher Level 1D of the National Council of Scientific and Technologic Development (CNPq), Brazil
Correspondence Address:
Marcelo R Lyra
Leishmaniasis Surveillance Laboratory (Lab Vigileish), Evandro Chagas Infectious National Institute (INI), Oswaldo Cruz Foundation (FIOCRUZ)
Brazil
| How to cite this article: Lyra MR, Valle AC, Pimentel MI, Antonio LF, Lyra JP, Ara�jo RC, Schubach AO. Scar examination in sporotrichosis: An additional tool for clinical diagnosis. Indian J Dermatol Venereol Leprol 2015;81:290-292 |
Sir,
Sporotrichosis is a subcutaneous mycosis caused by a dimorphic, saprophytic fungus Sporothrix schenckii. It affects several animal species including humans, and usually occurs after inoculation of the fungus through the skin or mucosa following minor trauma.
The infection may be acquired during leisure activities, or occupationally among farmers and gardeners who come in contact with vegetables or soil. Transmission from cats via bites or scratches has been reported as the main form of transmission in Rio de Janeiro. [1],[2] A feline epidemic was detected in 1998, which was accompanied by an increase in the number of human cases suffering from sporotrichosis. [3] At the Evandro Chagas Infectious National Institute, 13 cases were registered between 1975 to 1997, 759 cases from 1998 to 2004, and 804 cases from 2005 to 2008. [4] In 2013, the number of new cases remained high and no reduction was expected in the short term.
The characteristic cutaneous lesion is a gumma, but it may be verrucous, plaque-like, nodular or ulcerated as well. Unusual clinical manifestations have been reported. [5] The disease evolves according to the patient′s immunity. Subclinical to localized forms with a solitary lesion without regional lymphangitis (25.3% cases), lymphocutaneous (55.6% cases), disseminated cutaneous, and extracutaneous forms have been described. A differential diagnosis of cutaneous leishmaniasis (due to overlapping of endemic areas) and other verrucous diseases must be included in the work up.
The large sample size allowed us to observe a clinical aspect not yet described in literature, which is the tendency of lesions to become linear when scarring [Figure - 1] and [Figure - 2]. This is independent of the original shape of the lesion or skin tension lines. The presence of atrophic areas intermixed with hypertrophic areas give the scar a unique appearance [Figure - 3].
 |
| Figure 1: (a) Linear scar on the face. (b) Hypertrophic linear scar on the right hand. (c) Arcuate scar on the forearm. (d) Multiple linear scars on the forearm |
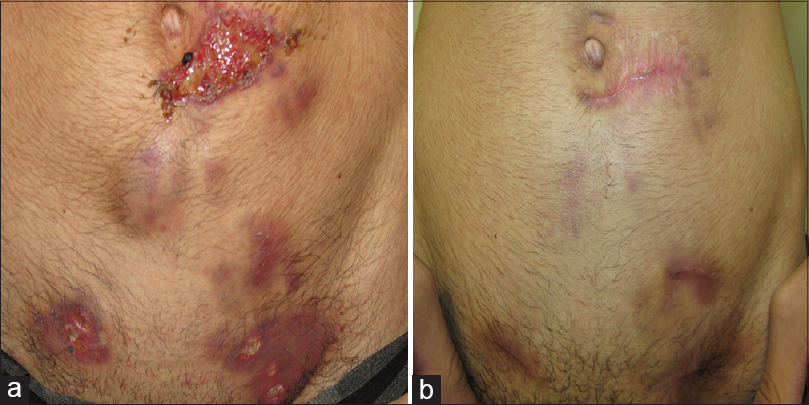 |
| Figure 2: (a) Multiple gummas at different stages of evolution: Nodular, fistulation and ulcerated lesions over the lower abdomen and inguinal region. (b) Presence of linear scars at the sites of preexisting disease |
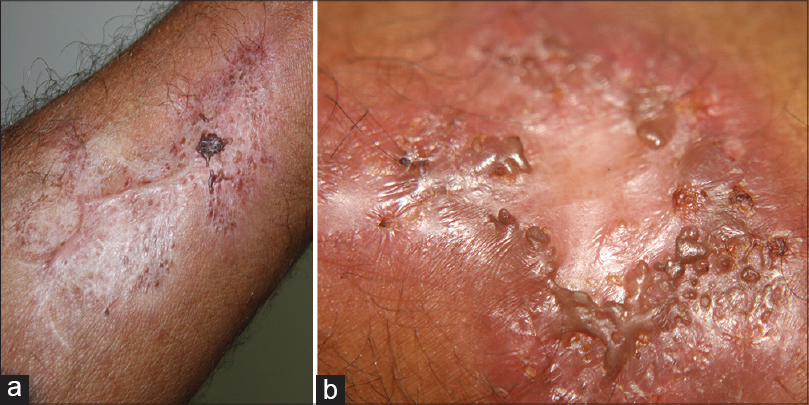 |
| Figure 3: (a and b) Atrophic scars intermixed with areas of hypertrophic scars |
Dermatological diagnosis is usually difficult in this region, as several infectious diseases such as leishmaniasis, sporotrichosis, chromomycosis, tuberculosis and paracoccidioidomycos coexist. The classical description that ulcerated lesions predominate in leishmaniasis, while gummas and lymphangitis predominate in sporotrichosis is valid, but there are exceptions to this rule. In such cases, the appearance of the scar becomes an important finding for differential diagnosis. Leishmaniasis scars are usually hypochromic, atrophic, or hypertrophic and tend to maintain the size of the primary ulcer. The newly described characteristics of sporotrichosis scars allow a good clinical differentiation in cases where scars coexist with active disease.
The diagnosis of sporotrichosis should be confirmed by isolation and identification of cultured Sporothrix schenckii, while leishmaniasis can be confirmed by culture, direct microscopic and histopathological examination. However, these diseases affect economically disadvantaged populations in developing countries, and such tests may be unavailable. In this scenario, good clinical examination and observing the appearance of scars during active disease will be a valuable tool to arrive at the dermatological diagnosis.
| 1. |
Barros MB, Schubach AO, Valle AC, Galhardo MC, Conceição-Silva F, Schubach TM, et al. Cat-transmitted sporotrichosis epidemic in Rio de Janeiro, Brasil: Description of a series of cases. Clin Infect Dis 2004;38:529-35.
[Google Scholar]
|
| 2. |
Schubach A, Schubach TM, Barros MB, Wanke B. Cat-transmitted sporotrichosis, Rio de Janeiro, Brazil. Emerg Infect Dis 2005;11:1952-4.
[Google Scholar]
|
| 3. |
Barros MB, Schubach TM, Galhardo MC, Schubach AO, Monteiro PC, Reis RS, et al. Sporotrichosis: An emergent zoonosis in Rio de Janeiro. Mem Inst Oswaldo Cruz 2001;96:777-9.
[Google Scholar]
|
| 4. |
Schubach A, Barros MBL, Wanke B. Epidemic Sporotrichosis. Curr Opin Infect Dis 2008;21:129-33.
[Google Scholar]
|
| 5. |
Mahajan VK, Sharma NL, Shanker V, Gupta P, Mardi K. Cutaneous sporotrichosis: Unusual clinical presentations. Indian J Dermatol Venereol Leprol 2010;76:276-80.
[Google Scholar]
|
Fulltext Views
3,115
PDF downloads
1,751





