Translate this page into:
Screening for skin diseases among primary school children in a rural area of Puducherry
Correspondence Address:
Suman Saurabh
Department of Preventive and Social Medicine (PSM), 4th floor, Administrative Block, JIPMER, Puducherry - 605 006
India
| How to cite this article: Saurabh S, Sahu SK, Sadishkumar A, Kakkanattu JC, Prapath I, Ralte IL, Kar V. Screening for skin diseases among primary school children in a rural area of Puducherry. Indian J Dermatol Venereol Leprol 2013;79:268 |
Sir,
Skin diseases are a common problem in school children. Contact between classmates is an important cause of skin infections and infestations. The prevalence and pattern of skin diseases has been seen to vary depending on the socio-economic and cultural factors related to hygiene and treatment-seeking behavior. [1],[2],[3],[4] Since treatment of skin complaints is often neglected by families due to lack of awareness and poor healthcare access, [1],[2] assessment of their burden and pattern at school may improve care through the school health program.
Objective of our cross-sectional study was to find the prevalence and pattern of skin diseases among primary school children in our service area. We screened children in primary classes 1-5 (5-10 year old) in four government schools situated in the service area of our Institute Rural Health Center at Puducherry.
The screening was done in August 2012 by a team of doctors and medical interns. A brief history of skin symptoms was followed by examination of scalp, skin, and nails after ensuring full privacy and adequate lighting. A clinical diagnosis based on examination findings was reached. The findings were also recorded in outpatient slips, which were handed over to the teachers so that the children could be brought to our center for treatment. Chi-square test was used to analyze the distribution of skin diseases with p-value less than 0.05 considered significant.
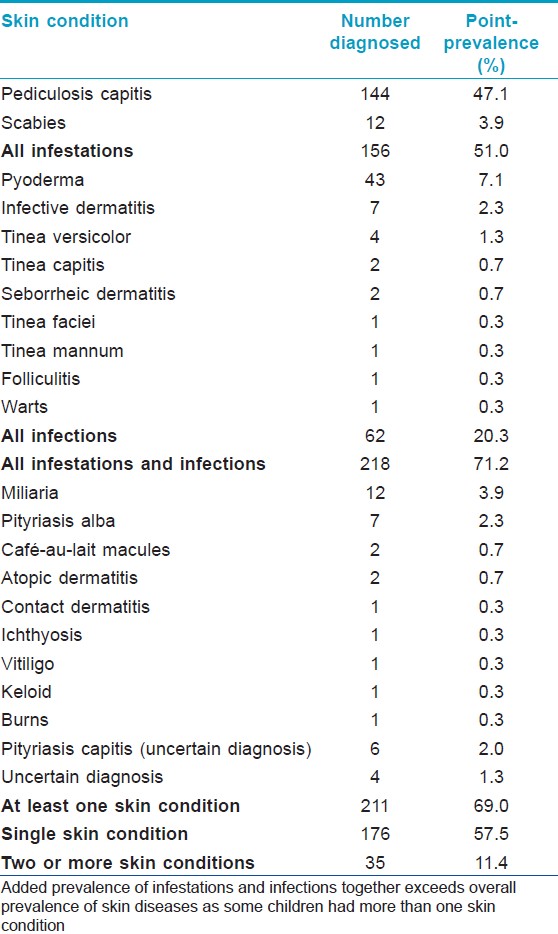
Out of the total 393 students enrolled in primary classes, 306 could be covered (77.9%). Two hundred and eleven students had at least one skin condition, yielding a prevalence of 69.0%. The prevalence in previous studies varied from 33.8% near Chandigarh, India [1] to 77% in Turkey [2] and 80.8% in Ethiopia. [3]
One hundred and seventy-six out of 211 (83.4%) children had a single skin condition. Out of the remaining 35 children, 27 had two, 7 had three, and 1 had four skin conditions. A total of 256 diagnoses were made for the 211 affected students.
Pediculosis itself accounted for 56.5% of these diagnoses with a prevalence of 47.1% [Table - 1]. The top three conditions i.e. pediculosis, pyoderma, and scabies contributed 77.7% of the total burden of skin diseases. Thus, simple approaches on promoting hygiene among school children may bring down the burden of skin diseases drastically.
Girls were affected more than the boys with overall prevalence of 78.5% and 55.2%, respectively (p < 0.001). Pediculosis was 2.3 times more common in girls as compared to boys (p< 0.001). This has previously been attributed to longer hair in girls. [2],[4] On the other hand, pyoderma was twice as common in boys compared to girls (p = 0.02). The prevalence of skin disease increased with age, from 50% for 5-year olds to 74.2% for 9-10 year olds (p = 0.0085). This increase may be explained by cumulative contact with other children increasing the infections and infestations in the absence of any treatment.
Similar high prevalence of pediculosis has been noted in other developing countries. [2],[3],[4] This may not be explained by poor socio-economic status alone. About one-third (30.5%) of the children with pediculosis reported positive family history, which was significantly higher than other skin conditions (p = 0.0011). This shows that cultural factors like sleeping in the same room might play a role in transmission. Furthermore, in our area, head-bath is mostly taken once a week, and sharing of combs and towels is common.
In a previous study, done at our hospital at Puducherry, pediculosis was surprisingly present only in 2.4% of children. [5] Also, only four affected children in our study reported seeking treatment for their skin complaints. This shows that conditions like head lice are seen merely as a nuisance due to lack of awareness in families. [1],[2] Presence of atopic dermatitis in only two children is consistent with its low prevalence in developing countries. [1],[2],[3]
We had a limitation that nutritional deficiency manifestations of skin and hair could not be assessed objectively. Referral to a qualified dermatologist for difficult diagnoses would have been preferable but was not feasible in our rural setting.
The highest reporting of 71.4% for treatment was from children of the village where the health center is situated. Reporting from the other three villages situated 3-8 km away was significantly lower at 31.8% (p< 0.001). Thus, we strongly feel that in order to be effective, skin care must be delivered at the school level itself. Training of teachers, health workers, interns, and doctors in managing common skin conditions must be incorporated in primary health care in the form of school health program.
Acknowledgement
We would like to thank all the teachers and students who participated in this study.
| 1. |
Dogra S, Kumar B. Epidemiology of skin diseases in school children: A study from northern India. Pediatr Dermatol 2003;20:470-3.
[Google Scholar]
|
| 2. |
Inanir I, Sahin MT, Gündüz K, Dinç G, Türel A, Oztürkcan S. Prevalence of skin conditions in primary school children in Turkey: differences based on socioeconomic factors. Pediatr Dermatol 2002;19:307-11.
[Google Scholar]
|
| 3. |
Figueroa JI, Fuller LC, Abraha A, Hay RJ. The prevalence of skin disease among school children in rural Ethiopia-a preliminary assessment of dermatologic needs. Pediatr Dermatol 1996;13:378-81.
[Google Scholar]
|
| 4. |
Suleman M, Fatima T. Epidemiology of head lice infestation in school children at Peshawar, Pakistan. J Trop Med Hyg 1988;91:323-32.
[Google Scholar]
|
| 5. |
Karthikeyan K, Thappa DM, Jeevankumar B. Pattern of pediatric dermatoses in a referral center in South India. Indian Pediatr 2004;41:373-7.
[Google Scholar]
|
Fulltext Views
2,158
PDF downloads
2,169





