Translate this page into:
Scrofuloderma associated with tuberculosis verrucosa cutis
Correspondence Address:
Angoori Gnaneshwar Rao
F-12, B-8, HIG-2, APHB, Baghlingampally, Hyderabad - 500 044, Andhra Pradesh
India
| How to cite this article: Rao AG. Scrofuloderma associated with tuberculosis verrucosa cutis. Indian J Dermatol Venereol Leprol 2014;80:76-78 |
Sir,
The prevalence of cutaneous tuberculosis among various dermatology out-patient departments in India ranges between 0.1-0.5%. [1] Scrofuloderma is a frequently encountered form of cutaneous tuberculosis among children in India, where as lupus vulgaris is the most common form of cutaneous tuberculosis seen in most countries. [2]
An 11-year-old boy was brought for swellings in the left groin and dorsum of left foot of 1-year duration. His mother noticed three linear swellings in the left groin, which ulcerated to discharge serosanguinous fluid, leading to partial healing. Later, she observed a small plaque on the dorsum of left foot. Examination revealed matted left inguinal lymphadenopathy and scar of bacillus Calmette-Guerin vaccination. There were three linear scars on the left groin measuring 3-5 cm in length and 0.5 cm in width [Figure - 1]. A well-circumscribed verrucous plaque of size 6 cm × 4 cm was noted on the dorsum of left foot [Figure - 2]. Diagnosis of scrofuloderma with tuberculosis verrucosa cutis was offered. Mantoux test was positive (18 mm). Smear and culture were negative for both Mycobacterium tuberculosis and fungus. Serology for human immunodeficiency virus was negative. X-ray chest, ultrasonography of the abdomen was unremarkable. Skin biopsy taken from both lesions revealed epithelioid cell granuloma with langhan′s-type of giant cells and dense collection of lymphocytes and plasma cells. Fite stain for acid-fast bacilli was negative. Biopsy tissue for polymerase chain reaction was negative for Mycobacterium tuberculosis. Characteristic morphology, positive Mantoux test and histopathology corroborated in establishing the diagnosis of scrofuloderma with tuberculosis verrucosa cutis.
 |
| Figure 1: Left groin showing three linear scars with sinus and crusted plaque and underlying swelling |
 |
| Figure 2: Hyperkeratotic plaque on the left foot |
The most common sites of scrofuloderma are the chest, neck and axilla. There was no evidence of systemic involvement in the index case. However, systemic involvement was reported in 21.3% of children with cutaneous tuberculosis. It has been observed that bacillus Calmette-Guerin vaccinated patients are less likely to develop disseminated tuberculosis. In concert with this, the index case developed localized cutaneous tuberculosis. Positive mantoux test in the index case concurs with the observation that the majority (98.1%) of children with localized cutaneous tuberculosis exhibit positive reaction to tuberculin antigen. [3] However, in India, mantoux reactivity does not correlate with the extent of the disease. In conformity with the various Indian studies, none of children with cutaneous tuberculosis, including ours, were tested positive for human immunodeficiency virus by enzyme-linked immunosorbent assay. Nonetheless, in a study of 231 patients with cutaneous tuberculosis (adults and children) only two tested positive for human immunodeficiency virus. [4] It is noteworthy that there was no report of coexistence of any type of cutaneous tuberculosis among them, subscribing to the proposition that coexistence is seen mostly in immunocompetent patients. The negative smear and culture for mycobacterium tuberculosis in the reported case could be due to the small number of bacilli in the localized cutaneous tuberculosis. Notably, tuberculous bacilli could be demonstrated in only 22.5% of children with scrofuloderma. [3] In a study, using culture on Lowenstein- Jensen′s medium, researchers observed positive cultures in 51.05% of patients with scrofuloderma, 42.85% with tuberculosis verrucosa cutis and 13.3% with lupus vulgaris. Histopathology confirmed the diagnosis of tuberculosis in the index case. In a study, classical tubercular histology was observed in 47.5% of patients with scofuloderma and 100% patients with tuberculosis verrucosa cutis. [3] Polymerase chain reaction for mycobacterium tuberculosis was negative. However, in a study on utility of polymerase chain reaction for cutaneous tuberculosis, it was found positive in 50% of cases of scrofuloderma and 62.2% cases of tuberculosis verrucosa cutis. Nonetheless, polymerase chain reaction provides rapid and sensitive detection of mycobacterium tuberculosis, particularly in paucibacillary tuberculosis. Furthermore, combination of dot hybridization with polymerase chain reaction markedly increases the sensitivity and specificity of polymerase chain reaction in detecting mycobacterium tuberculosis.
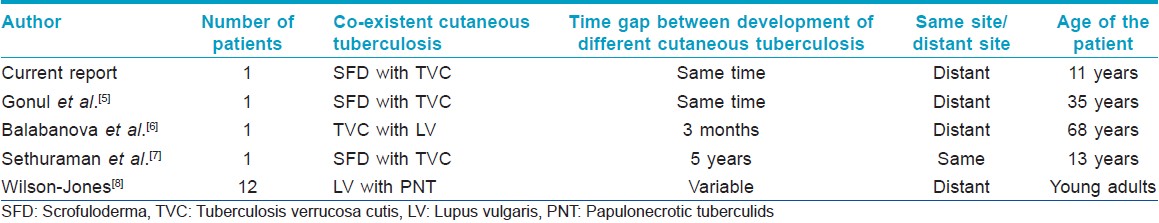
Coexistence of scrofuloderma with tuberculosis verrucosa cutis in the same patient, as seen in the index case, is rare. Both types of cutaneous tuberculosis have diverse underlying immunity as evidenced by CD4 + /CD8 + ratio in the granuloma: Scrofuloderma with low level immunity and tuberculosis verrucosa cutis with intermediate immunity. Gonul et al., reported such coexistence in a 35-year-old woman, who developed scrofuloderma in the left axilla and tuberculosis verrucosa cutis on the dorsum of the left hand at the same time. [5] The case under study also presented with scrofuloderma in the left groin and tuberculosis verrucosa cutis on the dorsum of the left foot simultaneously. Interestingly, tuberculosis verrucosa cutis lesions in both cases are distantly placed from scrofuloderma lesions, albeit on the same limb. Balabanova et al., have also reported coexistence of tuberculosis verrucosa cutis with lupus vulgaris in a 68-year old peasant, who initially developed lupus vulgaris on the chin and 3-months later developed tuberculosis verrucosa cutis on the left foot. [6] Of note, is the distant location of tuberculosis verrucosa cutis away from scrofuloderma/lupus vulgaris in all the three case reports including the index case. Sethuraman et al., reported coexistence of bilateral scrofuloderma with tuberculosis verrucosa cutis in a 13-year-old girl who initially developed scrofuloderma involving both ankles and 5-year later developed tuberculosis verrucosa cutis over the same sites [7] [Table - 1]. The bilateral involvement of scrofuloderma and the development of tuberculosis verrucosa cutis on the scrofuloderma at same sites are noteworthy. Wilson-Jones also reported coexistence of lupus vulgaris with papulonecrotic tuberculids in his study of 12-patients. [8]
Coexistence of scrofuloderma and tuberculosis verrucosa cutis in the same patient is rare and more so in a child like the case under study. The physician should be aware that a patient with one form of cutaneous tuberculosis may also have another form as well.
| 1. |
Kumar B, Kaur S. Pattern of cutaneous tuberculosis in North India. Indian J Dermatol Venereol Leprol 1986;52:203-7
[Google Scholar]
|
| 2. |
Amézquita R. Tuberculosis Cutis, aspects clinocos epidemiologicosen Mexico. Thesis, Acta Leprol, Vol 16. Abstract in Excerpta Medica 1965; 19:674.
[Google Scholar]
|
| 3. |
Kumar B, Rai R, Kaur I, Sahoo B, Muralidhar S, Radotra BD. Childhood cutaneous tuberculosis: A study over 25 years from northern India. Int J Dermatol 2001;40:26-32.
[Google Scholar]
|
| 4. |
Umapathy KC, Begum R, Ravichandran G, Rahman F, Paramasivan CN, Ramanathan VD. Comprehensive findings on clinical, bacteriological, histopathological and therapeutic aspects of cutaneous tuberculosis. Trop Med Int Health 2006;11:1521-8.
[Google Scholar]
|
| 5. |
Gonul M, Gul U, Kilic A, Soylu, S, Demiriz M, Kubar A. Coexistence of tuberculosis verrucosa cutis with scrofuloderma-A case report. Turk J Med Sci 2008;38:495-9.
[Google Scholar]
|
| 6. |
Pramatarov K, Balabanova M, Miteva L, Gantcheva M. Tuberculosis verrucosa cutis associated with lupus vulgaris. Int J Dermatol 1993;32:815-7.
[Google Scholar]
|
| 7. |
Sethuraman G, Kaur J, Nag HL, Khaitan BK, Sharma VK, Singh MK. Symmetrical scrofuloderma with tuberculosis verrucosa cutis. Clin Exp Dermatol 2006;31:475-7.
[Google Scholar]
|
| 8. |
Wilson-Jones E, Winkelmann RK. Papulonecrotic tuberculid: A neglected disease in Western Countries. J Am Acad Dermatol 1986;14:815-26.
[Google Scholar]
|
Fulltext Views
5,732
PDF downloads
2,903





