Translate this page into:
Secukinumab induced paradoxical worsening of mucocutaneous features of Behcet’s disease
Corresponding author: Dr. Vishal Gupta, Department of Dermatology, All India Institute of Medical Sciences, New Delhi, India. doctor.vishalgupta@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Goyal A, Meshram AS, Gupta V. Secukinumab induced paradoxical worsening of mucocutaneous features of Behcet’s disease. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1883_2024
Dear Editor,
A 26-year-old woman with an 8-year history of recurrent oro-genital and perianal aphthous ulcers and a 1-year history of recurrent painful erythematous papulo-pustules on extremities was referred to our outpatient department with a diagnosis of Behcet’s disease. She had no history of other systemic complaints, including ocular, articular, gastrointestinal, and central nervous systems. Screening for HLAB51 was negative. She had been previously treated with oral prednisolone (20-40 mg/day) along with various immunomodulators (colchicine, thalidomide, azathioprine, cyclosporine, and apremilast) at different time points with moderate-to-good improvement. Still, the disease exacerbated on tapering prednisolone to <20 mg/day. At the time of presentation, she had generalised painful papulo-pustules and multiple oral aphthae. We started the patient on tapering doses of oral prednisolone (starting from 30 mg), methotrexate (20 mg per week), and dexamethasone pulses (100 mg x 3 consecutive days every month). She responded well to the treatment over the next 6 months, but there was a mild recurrence of oral aphthae and cutaneous lesions when prednisolone was tapered to 10 mg on alternate days. The prednisolone dose was increased to 20 mg daily with disease control, and the treatment plan was switched to secukinumab. The patient experienced a mild disease flare following the first two doses of 150 mg secukinumab, following which she autonomously increased the prednisolone dose to 40 mg daily. Despite the prednisolone hike, she developed another more severe flare within 2 days of the third secukinumab dose. Oral thalidomide (100 mg b.d.) was added with improvement over the next few days, but another disease flare happened one day after the fourth secukinumab dose. All the flares were limited to mucocutaneous disease [Figures 1-2], with no systemic manifestations. Secukinumab was discontinued, and her disease improved significantly over the next 2 weeks. At the last follow-up visit, her prednisolone dose was tapered to 20 mg, while continuing thalidomide and methotrexate.
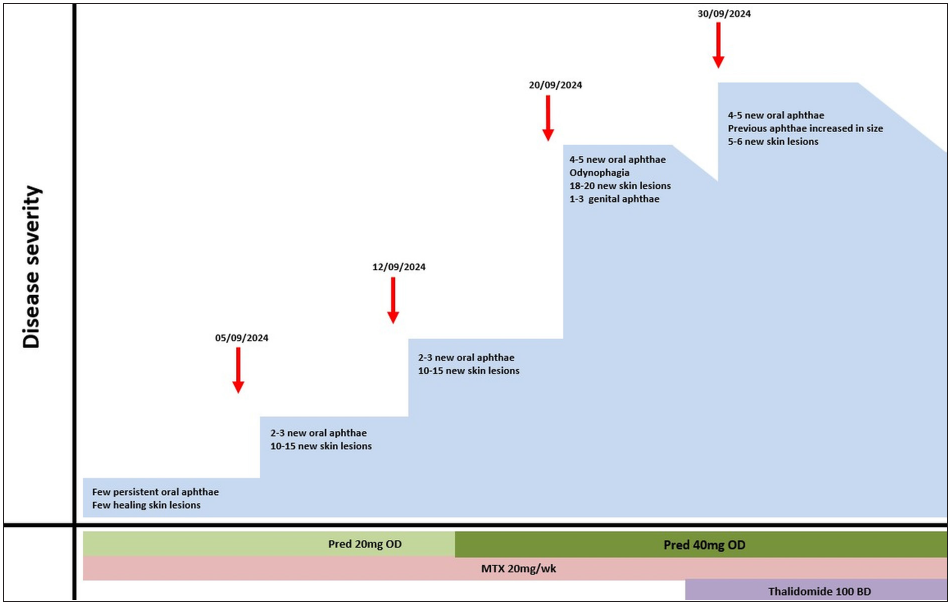
- Timeline showing Behcet’s disease flares with secukinumab treatment (red arrows indicate secukinumab injections).

- Major aphthous ulcer on the tongue.
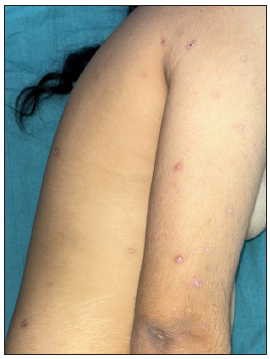
- Multiple erythematous papules and pustules on upper extremities and the trunk.
Apart from Th1 cells, there is an emerging role of Th17 cells in the immunopathogenesis of Behcet’s disease.1 Secukinumab has been found to be safe and effective in treating the mucocutaneous and articular manifestations of refractory Behcet’s disease. In a retrospective series of 15 patients, seven showed a complete response within 6 months, six had a partial response, and two were non-responders.2 Another series of five patients also reported complete response in all the patients with a dose of 150-300 mg, with the higher dose being used for patients with articular symptoms (n=1) or in patients not responding to 150 mg (n=3).3
Secukinumab led to the paradoxical worsening of mucocutaneous manifestations of Behcet’s disease in our patient. We had switched the treatment from steroid pulses to secukinumab in view of the steroid-dependent disease. The disease was relatively well-controlled before, and the flares occurred shortly after each secukinumab administration which required hiking up of the immunosuppressive treatment. Apart from temporal correlation, the fact that the disease showed signs of improvement in the period between secukinumab injections further favours this possibility over spontaneous disease flares.
We found a few reports of Behcet’s-like disease with the use of IL-17 blockers for other indications, such as psoriasis, ankylosing spondylitis, and hidradenitis suppurativa.4 The onset of Behcet’s disease was documented 2-40 weeks after initiation of IL-17 blockers, most commonly as fever and oro-genital ulcers, while other features included papulo-pustules, erythema nodosum-like lesions, and uveitis. All the cases were treated with oral steroids and discontinuation of IL-17 inhibitors. A subset of patients with IL-17 inhibitor-induced Behcet’s disease were found to be positive for HLA-B51 or HLA-B13/B50, suggesting a potential genetic link.4 Though the pathogenesis of such a paradoxical reaction is not clear, it is possible that IL-17 inhibition could disrupt the balance between Th17/Th1 cells and T-regulatory cells, leading to Behcet’s-like manifestations.5 IL-17 blocker-induced paradoxical psoriasis and eczematous eruptions are well-documented. Through this case, we wish to increase awareness about IL-17 blockers triggering the paradoxical flare of Behcet’s disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Immunopathogenesis of Behcet’s Disease. Front Immunol.. 2019;10:665.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Long-term effectiveness and safety of secukinumab for treatment of refractory mucosal and articular Behçet’s phenotype: a multicentre study. Ann Rheum Dis. 2020;79:1098-104.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of the anti-IL 17 secukinumab in refractory Behçet’s syndrome: A preliminary study. J Autoimmun. 2019;97:108-13.
- [CrossRef] [PubMed] [Google Scholar]
- Behcet’s-like disease induced by secukinumab in a patient with psoriasis: A case report and literature review. J Dermatol Treat. 2024;35
- [Google Scholar]
- Microbiome and Behçet’s disease: a systematic review. Clin Exp Rheumatol.. 2023;41:2093-104.
- [CrossRef] [PubMed] [Google Scholar]






