Translate this page into:
Seroprevalence of syphilis and biologically false positive cases in a tertiary care center
Correspondence Address:
Supriya Sanjay Tankhiwale
Department of Microbiology, Government Medical College, Nagpur - 440 003, Maharashtra
India
| How to cite this article: Tankhiwale SS, Naikwade SR. Seroprevalence of syphilis and biologically false positive cases in a tertiary care center. Indian J Dermatol Venereol Leprol 2014;80:340-341 |
Sir,
Syphilis remains an important cause of morbidity in India and is associated with other ulcerative sexually transmitted infections. Serology remains the mainstay of diagnosis of syphilis. Two categories of serological tests for the diagnosis of syphilis are currently available: cardiolipin tests like the Venereal Disease Research Laboratory (VDRL) test and specific tests like the Treponema pallidum hemagglutination assay (TPHA). The World Health Organization recommends the use of a combination of a non-treponemal test and a treponemal test for screening and diagnostic purposes. [1]
However, at many centres, the diagnosis is made based only on the VDRL test resulting in misdiagnosis, under or over-diagnosis due to the nonspecific nature of the test.
In view of this, the present study was planned to know the seroprevalence of syphilis and the proportion of biological false positive VDRL reactions by subjecting all reactive sera to treponemal tests like the treponema pallidum hemagglutination assay. A total number of 13008 patients attending the sexually transmitted disease (STD) clinic, antenatal clinic (ANC) and those referred by non-government organizations (NGOs) were included in the study period from June 2012 to March 2013. The patients referred by NGOs include female sex workers, men who have sex with men and transgenders. Among 13008 patients, 2537 were males, 10414 were females and 57 were transgenders.
Serum samples from all patients were screened for cardiolipin antibodies by the VDRL test using antigen obtained from the serologist to Government of India, Kolkata. VDRL-reactive specimens were subjected to quantitative VDRL test with successive two-fold dilutions. All the sera reactive in qualitative VDRL test were examined for antitreponemal antibodies by TPHA test (Plasmatec, UK). VDRL and TPHA tests were performed according to standard procedures following manufacturer′s instructions.
The majority of the male patients belonged to age group 25 to >45 yrs whereas the female patients included were of younger age, (from 22 to 44 yrs). Most of the patients referred from Non Governmental Organisations were <20 yrs age. VDRL reactive sera were divided into two categories, one having titre <1:8 and other one with titre ≥1:8 for evaluation of TPHA results and for assessment of biological false positives.
The overall seroprevalence of syphilis in the study group was 0.7% (90/13008). Out of three groups, the seroprevalence was highest in male attendees of STD clinic (1.42%). Almost equal numbers of male patients (0.34%) and female patients (0.35%) were seropositive. When analysed according to sub-groups, there was a statistically significant difference by chi square test (P = 0.05) between the seroprevalence of syphilis in males and females. The seroprevalence in males was 1.73% (44 of 2537) and in females was 0.4% (46 of 10414) which is comparable to the report by Geusau et al.[2] Regarding syphilis seroprevalence, different studies show variable findings. [3] In a Delhi based study, among the patients attending various hospitals, seroprevalence of syphilis was 1.2%. [4] The low seroprevalence in our study could be attributed to the diverse population under study and differences in sociocultural aspects.
In our study, seroprevalence of syphilis was found to be highest in STD clinic attendees (1.35%) followed by patients referred by non-governmenatal organizations (0.8%) and least in samples from antenatal clinics (0.07%). The highest seroprevelance was in STD clinic attendees emphasizing the need for sexual health education for these groups. A Delhi-based study also found the highest seroprevalence of syphilis in STD clinic attendees (3.5%) followed by various outpatient departments, wards (1.43%) and antenatal clinics (0.75%) [4] which may be due to the fact that it is a large metropolitan city.
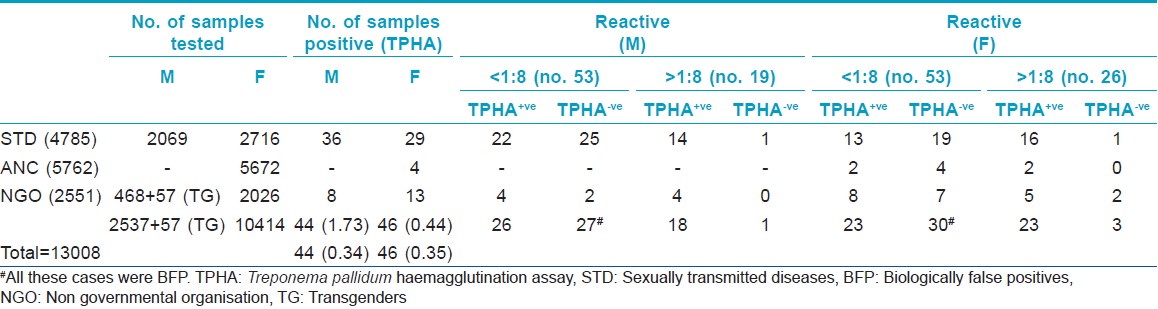
[Table - 1] shows sex-wise distribution of results of TPHA tests in the two groups. There were 53 males and females each with a VDRL titer <1:8 while there were 19 males and 26 females with tires ≥1:8. Sixty-one cases which were VDRL reactive but TPHA negative were considered biologogical false positives. Thus, the proportion of biological false positive cases in the present study was 0.47% (61/13008) which is comparable to 0.5% by Hossain et al.,[5] in Saudi Arabia.
A lower proportion of biological false positives (0.47%) in the present study shows the importance of TPHA in diagnosing syphilis. More false positives would have reported if only the non-specific VDRL test had been used (90/13008=0.69%). Though TPHA is not a 100% sensitive and specific test, the ease of performing the test in a less-equipped laboratory makes it a better option than more specific treponemal tests.
Acknowledgment
The authors acknowledge National AIDS Control Organisation (NACO), New Delhi and Maharashtra State AIDS Control Society, Mumbai for financial support. We are thankful to Dr. R.P. Singh and Dr. S.S. Fusey for sending the cases and Mrs. Kalindi Deogade and Mrs. Manisha Sharma for their technical support.
| 1. |
World Health Organization. Treponemal infections. Technical reports series 674. Geneva: WHO; 1982.
[Google Scholar]
|
| 2. |
Geusau A, Kitter H, Hein U, Dangl-Erlach E, Stingl G, Tschachler E. Biological false positive tests comprise a high proportion of Venereal Disease Research Laboratory reactions in an analysis of 300, 000 sera. Int J STD AIDS 2005;16:722-6.
[Google Scholar]
|
| 3. |
Maity S, Bhunia SC, Biswas S, Saha MK. Syphilis seroprevalence among patients attending sexually transmitted disease clinic in West Bengal, India. Jpn J Infect Dis 2011;64:506-8.
[Google Scholar]
|
| 4. |
Bala M, Toor A, Malhotra M, Kakran M, Murlidhar S, Ramesh V. Evaluation of the usefulness of Treponema pallidum haemagglutination test in the diagnosis of syphilis in weak reactive Venereal Disease Research Laboratory sera. Indian J Sex Transm Dis 2012;33:102-6.
[Google Scholar]
|
| 5. |
Hussain T, Kulshreshtla KK, Yadav VS, Sengupta V, Katoch VM. Seroprevalence of human immunodeficiency virus and syphilis infections among patients attending the STD, Gyn. and Obs. ANC clinics of northern India: Observations from seven rounds of sentinel surveillance (1998-2004). Am J Infect Dis 2006;2:28-35.
[Google Scholar]
|
Fulltext Views
4,276
PDF downloads
2,182





