Translate this page into:
Sexual behavior and condom use among a population of men who have sex with men attending a dermatology-sexually transmitted infection clinic in Beirut-Lebanon
Correspondence Address:
Isma�l Maatouk
Hammoud Medical University Hospital, Beirut
Lebanon
| How to cite this article: Maatouk I. Sexual behavior and condom use among a population of men who have sex with men attending a dermatology-sexually transmitted infection clinic in Beirut-Lebanon. Indian J Dermatol Venereol Leprol 2016;82:687-689 |
Sir,
In Lebanon, men who have sex with men may account for most new human immunodeficiency virus (HIV) infections.[1],[2] The proportion of people infected with HIV among men who have sex with men in 2011 is estimated at 3.6%.[3]
Few studies of high risk behavior among men who have sex with men have been undertaken in Lebanon, probably because of the social and religious taboos and because homosexuality is highly stigmatized and even illegal.[4] Studies in Lebanon have revealed that approximately 50% of men who have sex with men consistently use condoms; however, only 25% reported using a condom during their last sexual intercourse.[5],[6],[7] On an average, men who have sex with men have 10–25 partners over a year.[1],[6],[8] According to the new World Health Organization consolidated guidelines, HIV testing is on the top list of the services that can help to prevent spreading the virus yet, the testing rate is as low as 24% in Lebanon.[3] All these studies included a group of men who have sex with men registered in non-governmental organizations; unfortunately, the population that seeks private care is almost unreachable.
During the first week of June 2015, 31 men who have sex with men attended the dermatology-sexually transmitted infection clinic for a medical consultation and they were invited to participate in the study. Data collected included (1) location, (2) age, (3) number of sexual partners in the preceding 6 months, (4) condom use in the last 10 sexual intercourses (oral sex excluded), (5) use of mobile dating applications, (6) alcohol and/or drugs during or before sex, (7) history of any sexually transmitted infection including human immunodeficiency virus, (8) frequency of sexually transmitted infection tests per year, (9) a subjective self-assessment of human immunodeficiency virus risk.
The questionnaire used for the study was based on one of the tools used for surveillance of HIV and other sexually transmitted infections among men who have sex with men in France.[9] The Hammoud Hospital Ethics Committee advised that formal ethical approval for the study was not required as protocols did not deviate from routine clinical practice. Participants provided written informed consent to participate in this study. Interviews were conducted in the language preferred by the participant (Arabic, French or English) on internet-based software.
The location of study subjects, numbers of sexual partners, condom use, use of cell phone dating applications, use of alcohol and/or drugs with sex, previous sexually transmitted infections including HIV infection, frequency of testing for sexually transmitted infections and subjective assessment of risk behaviour are shown in [Table - 1].
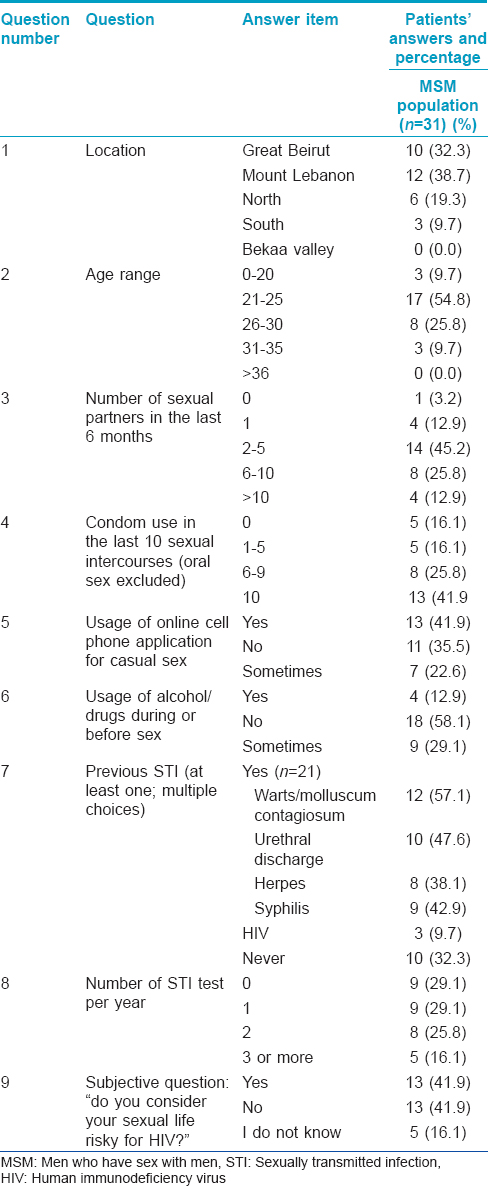
This small study reporting data from a dermatology-sexually transmitted infection clinic helps to explore some factors of sexual behavior and condom use in men who have sex with men. This data can guide sexually transmitted infections screening and prevention strategies to be implemented in this hard-to-reach stigmatized population. As was the case in previous studies, this study suggests that unprotected anal sex is very common among this sample of mostly young and urban men. Eighteen (58.1%) participants had unprotected anal sex, which is slightly lower than the number found by Wagner et al. which was 64%.[10]
Three (9.7%) men tested positive for human immunodeficiency virus in this sample which is a higher rate compared to the estimated percentage (1.5%) found in a previous larger study done on this population.[10]
Our study population had a much higher rate of testing for sexually transmitted infections, 22 men (71%) had undergone at least one test in the past year than reported in other studies of men who have sex with men in Lebanon and the Middle East region.[2],[10] This may be because of the health-care seeking behavoiur of our study participants or because of the increased awareness created by the national health programs. However, 29% did not undergo any tests. None of our participants had other sexually transmitted infections or syndromes, probably because they were treated by other specialists.
The mean number of sexual partners in the last 3 months, in a previous study, was reported to be 2.[10] Most of our patients (45.2%) fell in the category of “2–5 partners for the last 6 months.”
New trends in sexual behavior among men who have sex with men in Lebanon that were not detected previously are (1) usage of online dating applications on the mobile phone (denied in only 35.5%) that may serve as a tool to reach potential partners (2) alcohol and/or drugs before/during sex (denied in 58.1%).
The presence of syphilis in 42.9% of our participants indicates a role for performing serological tests for syphilis routinely in this population. To the subjective question on whether they considered themseveles at risk of acquiring human immunodeficiency virus infection, the study patients equally answered “yes” or “no” (16.1% answered“I do not know.”) Thus, this population of young urban men is aware of the human immunodeficiency virus which is most probably due to the campaigns led by Lebanon's national acquired immune deficiency syndrome control program and local organizations.
A key limitation of our data was the low sample size and the poor representation of older (aged above 36) men. Other papers have reported similar limitations, the reason being, perhaps, a lack of intrinsic motivation to participate.[11]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
WHO, UNICEF, UNAIDS. Global HIV/AIDS Response: Epidemic Update and Health Sector Progress Towards Universal Access, in Progress Report. Geneva, Switzerland: World Health Organization; 2011.
[Google Scholar]
|
| 2. |
Mumtaz G, Hilmi N, McFarland W, Kaplan RL, Akala FA, Semini I, et al. Are HIV epidemics among men who have sex with men emerging in the middle east and North Africa? A systematic review and data synthesis. PLoS Med 2010;8:e1000444.
[Google Scholar]
|
| 3. |
Afifi R, DeJong J, El-Barbir F, El-Khoury D, Ghanem M, Kassak K, et al. Mishwar: An Integrated Bio-behavioral Surveillance Study among Most at Risk Populations in Lebanon: Female Sex Workers, Injections Drug Users, Men who Have Sex with Men, and Prisoners, in Final Report. Beirut, Lebanon: Ministry of Public Health; 2008.
[Google Scholar]
|
| 4. |
Obermeyer CM. HIV in the middle east. BMJ 2006;333:851-4.
[Google Scholar]
|
| 5. |
Mahfoud Z, Afifi R, Ramia S, El Khoury D, Kassak K, El Barbir F, et al. HIV/AIDS among female sex workers, injecting drug users and men who have sex with men in Lebanon: Results of the first biobehavioral surveys. AIDS 2010;24 Suppl 2:S45-54.
[Google Scholar]
|
| 6. |
Wagner GJ, Aunon FM, Kaplan RL, Rana Y, Khouri D, Tohme J, et al. Aqualitative exploration of sexual risk and HIV testing behaviors among men who have sex with men in Beirut, Lebanon. PLoS One 2012;7:e45566.
[Google Scholar]
|
| 7. |
Kahhaleh JG, El Nakib M, Jurjus AR. Knowledge, attitudes, beliefs and practices in Lebanon concerning HIV/AIDS, 1996-2004. East Mediterr Health J 2009;15:920-33.
[Google Scholar]
|
| 8. |
Nakib ME, Hermez J. HIV/AIDS Prevention among Vulnerable Groups in Beirut, Lebanon. in XIV International AIDS Conference AIDS 2002. Barcelona, Italy; 2002.
[Google Scholar]
|
| 9. |
Elford J, Jeannin A, Spencer B, Gervasoni JP, van de Laar MJ, Dubois-Arber F; HIV and STI Behavioural Surveillance Mapping Group. HIV and STI behavioural surveillance among men who have sex with men in Europe. Euro Surveill 2009;14. pii: 19414.
[Google Scholar]
|
| 10. |
Wagner GJ, Tohme J, Hoover M, Frost S, Ober A, Khouri D, et al. HIV prevalence and demographic determinants of unprotected anal sex and HIV testing among men who have sex with men in Beirut, Lebanon. Arch Sex Behav 2014;43:779-88.
[Google Scholar]
|
| 11. |
Yeka W, Maibani-Michie G, Prybylski D, Colby D. Application of respondent driven sampling to collect baseline data on FSWs and MSM for HIV risk reduction interventions in two urban centres in Papua New Guinea. J Urban Health 2006;83 6 Suppl: i60-72.
[Google Scholar]
|
Fulltext Views
2,417
PDF downloads
1,370





