Translate this page into:
Sister Mary Joseph's nodule derived from lung cancer
2 Department of Pneumology, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
Correspondence Address:
Xingqi Zhang
Department of Dermatology, The First Affiliated Hospital, Sun Yat-sen University, No. 58 Zhongshan Er Road, Guangzhou, 510080
China
| How to cite this article: Wang F, Chen H, Zhang X. Sister Mary Joseph's nodule derived from lung cancer. Indian J Dermatol Venereol Leprol 2011;77:609-611 |
Sir,
Sister Mary Joseph′s nodule (SMJN) refers to metastatic malignant tumor nodules of the umbilicus, which was first introduced by Hamilton Bailey in 1949. It was named after Sister Mary Joseph, a nurse who was the first person to observe umbilical nodules as one of the less-well known signs of intraabdominal metastatic disease. It can be the first symptom of an underlying cancer.
In most cases, common sites of primary tumors of the SMJN are the stomach and colon in males, but ovaries and endometrium in females. Rare metastases from other areas such as cecum, pancreas, gall bladder, fallopian tube and prostate have also been reported. However, in as many as 30% of the cases, the site of origin of the metastasis remains unidentified. [1] We present here a case of SMJN originating from the pulmonary adenocarcinoma and discuss its possible modes of metastatic spread.
A 51-year-old female presented with a painless, ulcerated mass in the umbilicus for more than 1 year. Three months before consultation, she developed right chest pain and tightness.
Physical examination revealed a dark-red subcutaneous nodule with an ulcerated surface and a purulent discharge in the umbilicus [Figure - 1]. On palpation, the nodule was hard, immobile and adherent to the overlying skin. Systemic examination revealed decreased breath sounds and dullness on chest auscultation at the right lower lung area. Serum titers of both carcinoembryonic antigen (CEA) and CYFRA21-1 were found to be positive. The chest computed tomography (CT) scan showed a parenchymal opacity in the right lower lung [Figure - 2]a. Obvious right pleural effusion and atelectasis of middle and lower lobes of the right lung was also noticed. Furthermore, CT scan of the upper abdomen showed thickening and beaded changes of the peritoneum and pleura at the basis pulmonis [Figure - 2]b. Smear examination of the pleural fluid revealed atypical cells. Thoracoscopy revealed numerous white lesions located on the right lung and right visceral pleura. Biopsy of the visceral pleura showed infiltration of malignant cells, suggestive of adenocarcinoma [Figure - 3]a, and was stained positively for both Cytokeratin 7 (CK7) and Cytokeratin 20 (CK20). Umbilical skin biopsy also showed adenocarcinoma cells positively stained for both CK7 and M-CEA infiltrating the whole dermis [Figure - 3]b. Thorough examination of other systems did not reveal any positive findings for neoplastic involvement. Based on the above clinical, laboratory, radiological and histological findings, the patient was diagnosed as lung adenocarcinoma: T4N1M1, stage IV.
 |
| Figure 1: Dark-red subcutaneous nodule with an ulcerated surface and a purulent discharge in the umbilical area |
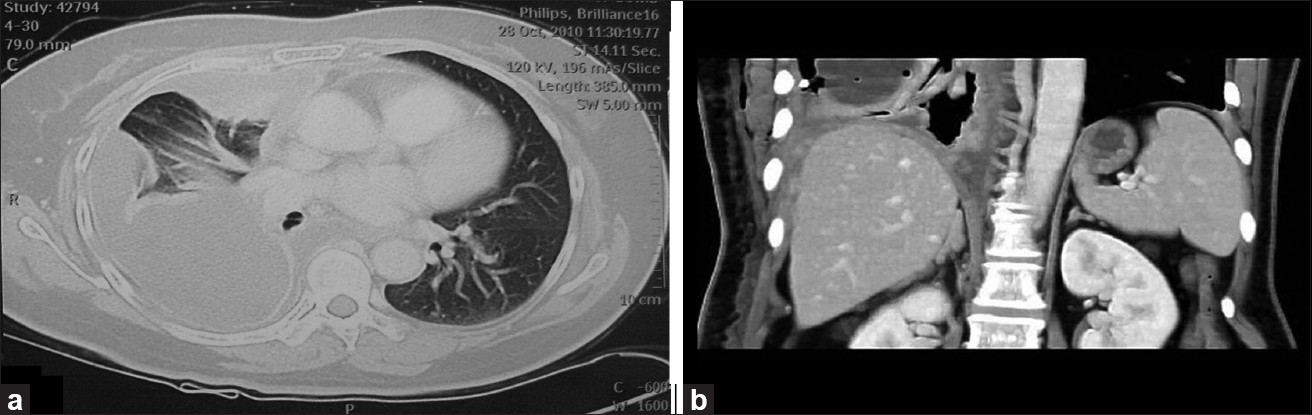 |
| Figure 2: (a) Computed tomography image of patient's chest showing right pleural effusion, atelectasis of right lung and parenchymal opacity. (b) Computed tomography image of the patient's upper abdomen showing thickening and beaded changes of the peritoneum and pleura at the basis pulmonis |
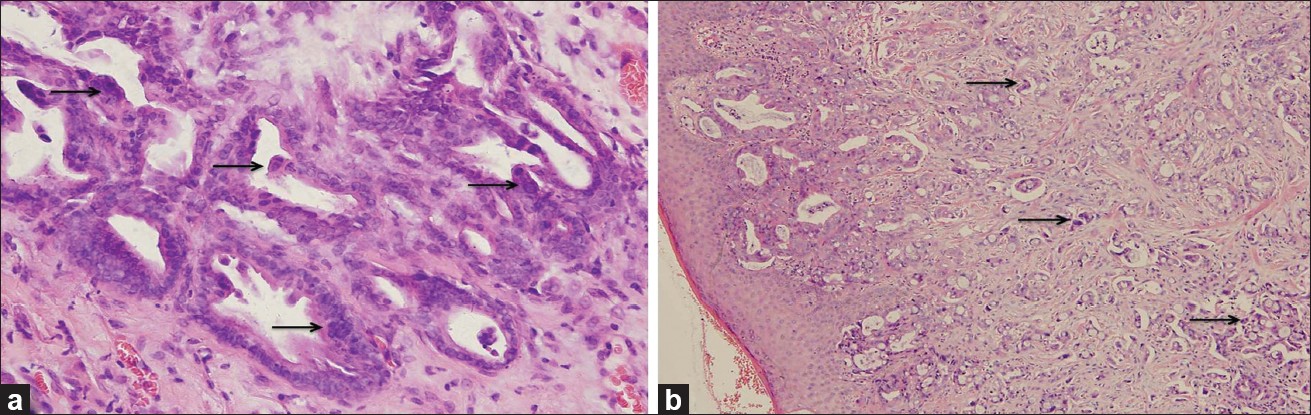 |
| Figure 3: (a) Adenocarcinoma cell infiltration (arrows) of visceral pleura (H and E, ×400). (b) Low-differentiated adenocarcinoma cell infiltration (arrows) of umbilical dermis (H and E, ×100) |
Although cutaneous metastasis from lung cancer is well recognized as most commonly involving the upper chest wall, umbilical metastasis from lung cancer is rather a rare event. Charoenkul et al. [2] reviewed 262 cases of reported umbilical metastases till 1977, without a single case originating from lung cancer. Up till now, only five cases of pulmonary adenocarcinoma from 121 cases of SMJN have been reported by several researchers. [3],[4] In our case, pulmonary adenocarcinoma was identified as the primary tumor of SMJN based on negative findings of the thorough examination of other systems, including gynecological organs and radiological imaging results, which showed involvement of the right lower lung manifesting as a single lesion only. We thus excluded the possibility of metastatic tumors to the lungs from other unidentified primary tumors that would, in contrast, have manifested as multiple lesions involving both lungs. Therefore, lung cancer should be recognized as one of the malignant neoplasms that can have umbilical metastasis. It should be pointed out that the patient developed cutaneous umbilical lesion that preceded chest symptoms; Therefore, SMJN may be the first presenting sign and may have clinical significance as an ominous diagnostic sign in the cases of disseminated lung cancer.
Possible modes of metastatic spread to the umbilicus can be either hematogenous, involving anastomosis of the paraumbilical and portal veins, or contiguous extension along the peritoneum, and embryonic structures such as the obliterated urachus, the ligamentum teres and the falciform ligament. [5] Similar to the case reported by Saito et al., [3] contiguous extension from the right pleura to the anterior peritoneal surface was the most likely mode of spread in our case, based on the abdomen CT findings, which revealed thickening and beaded changes of the anterior peritoneum. We presume that the right lung cancer is more prone to umbilical metastasis than the left lung cancer, as the right pleura is closer to the above-named embryonic structures than the left pleura.
We reported a case of SMJN originating from pulmonary adenocarcinoma to extend the list of differential diagnosis of SMJN in female patients and emphasize the importance of examination of the respiratory system, apart from other systems of common origin in suspected cases.
| 1. |
Deb P, Rai RS, Rai R, Gupta E, Chander Y. Sister Mary Joseph nodule as the presenting sign of disseminated prostate carcinoma. J Cancer Res Ther 2009;5:127-9.
[Google Scholar]
|
| 2. |
Charoenkul V, DelCampo A, Derby A, Hodgson WJ, McElhinney AJ. Tumors of the umbilicus. Mt Sinai J Med 1977;44:257-62.
[Google Scholar]
|
| 3. |
Saito H, Shimokata K, Yamada Y, Nomura F, Yamori S. Umbilical metastasis from small cell carcinoma of the lung. Chest 1992;101:288-9.
[Google Scholar]
|
| 4. |
Dodiuk-Gad R, Ziv M, Loven D, Schafer J, Shani-Adir A, Dyachenko P, et al. Sister Mary Joseph's nodule as a presenting sign of internal malignancy. Skinmed 2006;5:256-8.
[Google Scholar]
|
| 5. |
B, Deng A. Umbilical metastasis from prostate carcinoma (Sister Mary Joseph's nodule): A case report and review of literature. J Cutan Pathol 2007;34:581-3.
[Google Scholar]
|
Fulltext Views
3,901
PDF downloads
1,688





