Translate this page into:
Spectrum of seborrheic keratoses in south Indians: A clinical and dermoscopic study
Correspondence Address:
Devinder Mohan Thappa
Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry 605 006
India
| How to cite this article: Rajesh G, Thappa DM, Jaisankar TJ, Chandrashekar L. Spectrum of seborrheic keratoses in south Indians: A clinical and dermoscopic study. Indian J Dermatol Venereol Leprol 2011;77:483-488 |
Abstract
Background: Even though seborrheic keratoses (SK) have been well characterized clinically and histopathologically, data regarding clinical and dermoscopic correlation of different types of SK are inadequate. Aims: We carried out a study to establish any correlation between the clinical and dermoscopic appearance of SK and its variants. Methods: This was a descriptive study conducted in the Department of Dermatology, a tertiary care institute, from August 2008 to June 2010. Patients with SK were evaluated with respect to age, sex, age of onset, duration, site of lesions, number of lesions, and morphology. Dermoscopy was performed in all cases. Results: A total of 250 cases of SK were recruited. A male-to-female ratio was 1:1.04. The most common age group affected by SK was 60 years and above (40%). The most common clinical variant was common seborrheic keratosis (CSK) (60%). Comedo-like openings (CL) (80%), fissures and ridges (FR) (52%), and sharp demarcation (SD) (83%) were consistent finding on dermoscopy in CSK. Dermatosis papulosa nigra (DPN) and pedunculated seborrheic keratoses (PSK) had characteristic CL and FR in both of them. Fingerprint (FP) (55%) and network-like (NL) (88%) structures were commonly seen in flat SK. Stucco keratoses demonstrated SD (100%) and NL structures (100%). Conclusions: The most common clinical variant of SK was CSK, followed by DPN, PSK, Flat SK, and stucco keratoses. Dermoscopic findings were consistent with those described in the literature.Introduction
Seborrheic keratoses (SK) are the most common benign epidermal tumors composed of epidermal keratinocytes. [1] The condition is very common in white races, usually occurs in middle-aged individuals and can arise as early as adolescence. [1] Males and females are equally affected. [2] The lesion of SK can occur at any site but most frequent on face and upper trunk. [1] The lesions are usually asymptomatic but may be itchy, [1] begin as well-circumscribed, dull, flat, tan, or brown patches with pseudohorn cyst. As they grow, they become more papular, taking on a waxy verrucous or "stuck on" appearance. Dermoscopy is helpful in establishing diagnosis in unclear cases.
Even though SK have been well characterized clinically and histopathologically, data regarding clinical and dermoscopic correlation of different types of SK are inadequate. Hence, this study is being carried out to determine the pattern of clinical variants of SK and to establish whether there is any correlation between the clinical variants of SK and their dermoscopic appearance.
Methods
It was a descriptive study conducted between August 2008 and June 2010 in the dermatology department at our institute. Institute ethical clearance was obtained before the study. All patients attending dermatology OPD with lesions of SK willing to participate in the study were included in the study. Full history and detailed examination were done. The following parameters were recorded: age, sex, age of onset, family history, duration, site of lesions, number of lesions, size of lesions and morphology. An incident light source (handheld magnifying lens with power Χ 10) was used to detect elevated skin lesions and also to examine surface texture of individual skin lesions. Dermoscopy (Hanse Microscope HVS-CM500N/D with magnifications Χ32 and Χ140) was performed in all cases in randomly chosen pigmented lesions which were clinically diagnosed as SK and the criteria for SK-Comedo-like (CL) openings, milia-like (ML) cysts, fissures and ridges (FR), fingerprint (FP)-like structures, moth-eaten (ME) border, hairpin (HP) blood vessels, network-like (NL) structures, and sharp demarcation (SD) were recorded and those requiring confirmation were biopsied. Patients were given appropriate treatment if needed. For the descriptive statistics, the SPSS 15 software package (SPSS Inc, Chicago IL, USA) was used.
Comedo-like openings are ′black head like′ plugs of brown to black color. ML cysts are round, whitish, or yellowish structures. Fissures are irregular linear keratin-filled depressions. FP-like structures are thin, brown, parallel lines resembling FPs. ME border is the concave border of the SK which has been compared to ME garment. HP blood vessels correspond to long capillary loops, mainly found at the border of SK. SD is the abrupt cut-off of the pigmented border. NL structures are grid-like or honeycomb-like structures resembling a pigment network of melanocytic lesions. [3],[4]
Results
A total of 250 patients, 128 (51.2%) females and 122 (48.8%) males, with SK were recruited in this study.
Onset of SK was most common in the 41-60 age group (126 cases, 50.2%) followed by the 21-40 age group (82 cases, 32.7%), 61-80 age group (34 cases, 13.5%), less than 20 years (7 cases, 2.8%), and only one case (0.4%) after 81 years.
Clinical variants of seborrheic keratoses
The most common clinical variant was common seborrheic keratoses (CSK) (150 cases, 60%) [Figure - 1] and [Figure - 2] followed by dermatosis papulosa nigra (DPN) (116 cases, 46.4%) [Figure - 3], pedunculated SK (PSK) (53 cases, 21.2%), flat SK (27 cases, 10.4%), and stucco keratoses (5 cases, 2%) [Figure - 4].
 |
| Figure 1: Common seborrheic keratoses on the chest |
 |
| Figure 2: Common seborrheic keratoses on the face |
 |
| Figure 3: Dermatosis papulosa nigra on the cheeks |
 |
| Figure 4: Stucco keratosis on the leg |
There was female preponderance in PSK (M:F = 1:1.65) and DPN (M:F = 1:1.42) and slightly male preponderance in CSK (M:F = 1.23:1) and both sexes almost equally affected in flat SK (M:F = 1.07:1). Out of 250 patients, 166 (66.4%) had only one clinical variant and 84 (33.6%) had more than or equal to two clinical variants.
Morphology of seborrheic keratoses
The size of the lesions was ranging from 1 mm to 4 cm. One largest SK of size 15 Χ 10 cm 2 was in the genital area in a female patient with vulval SK. The total number of SK recorded in all subjects were 10,479. Seventy cases (28%) had lesions more than or equal to 1 cm.
All the cases in the study had pigmented SK and were divided by color into black, dark-brown, and grey. Most common is black colored SK (199 cases, 79.6%) followed by dark-brown (86 cases, 34.4%), and grey (23 cases, 9.2%). Most common type according to primary lesions was the papular type (195 cases. 78%) followed by the plaque type (94 cases, 37.6%), pedunculated type (53 cases, 21.2%), patch type (26 cases, 10.4%), and one SK was a polypoidal mass in the genital area. Most of the SKs have the verrucous surface (193 cases, 77.2%) followed by those with flat topped (66 cases, 26.4%) and macular (16 cases, 6.4%) surface. One patient had "raindrop pattern" of SK on back.
Only five cases (2%) gave family history of SK. Four (80%) out of them had DPN and the one case with PSK. SK were asymptomatic in 98.8% of cases and only 1.2% had itching in the lesions in the study group, lesions were present in more than two body sites in the symptomatic group.
Dermoscopy
Dermoscopic examination was done in all cases in randomly chosen pigmented lesions which were clinically diagnosed as SK and the criteria for SK-CL openings, ML cysts, FR, FP structures, ME, HP blood vessels, NL structures, and SD were recorded.
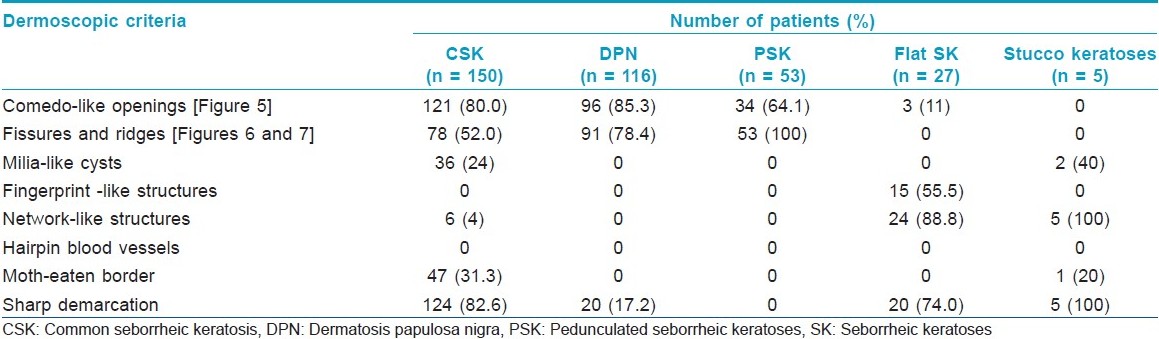
The dermoscopic findings recorded in various clinical variants of SK have been summarized as shown in [Table - 1].
Twenty cases (8%) with CSK had dermoscopic findings of white to black, yellowish green horn masses with background features of SK-like CL and FR. These lesions were clinically looking hyperkeratotic [Figure - 5], [Figure - 6] and [Figure - 7].
 |
| Figure 5: Comedo-like openings on the surface of common seborrheic keratosis |
 |
| Figure 6: Comedo-like openings, fissures, and ridges on pedunculated seborrheic keratosis |
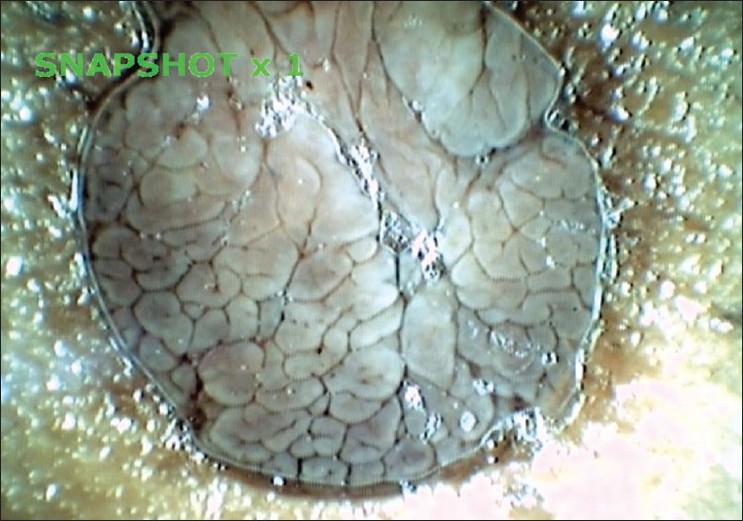 |
| Figure 7: Cerebriform appearance with mainly fissures and ridges on pedunculated seborrheic keratosis |
Shave biopsy for histopathology was done in 10 cases confirming the clinical diagnosis of SK. Among these, seven were of the acanthotic SK type, two were of stucco keratoses and one was of melanoacanthoma.
Discussion
The frequency of SK appears to increase with age. In an Australian study of 100 people composed, 12% of people aged 15-25 years (n = 34), 79% of people aged 26-50 years (n = 24), 100% of people aged 51-75 years (n = 25), and 100% of people older than 75 years (n = 17) had SK and showed increase in the prevalence of SK with advancing age. [5] Similarly, a Korean study with 303 men aged 40-70 years showed considerable increase in the prevalence of SK from 78.9% at 40 years to 93.9% at 50 years and 98.7% in those over 60 years. [6] In our study, 250 patients are with SK. The most common age group affected by SK was 60 years and above (100 cases, 40%), followed by 51-60 years (64 cases, 25.5%), 41-50 years (45 cases, 17.9%), 31-40 years (29 cases, 11.6%) and less than 30 years (12 cases, 4.8%) showing a clear correlation of SK with age as mentioned in the literature.
Clinical variants
Common seborrheic keratoses
Common SK appear only on hair-bearing surfaces, predominantly on the head, trunk, and neck. They commonly present as sharply demarcated, brown, ′′stuck on′′ papules with velvety or granular surfaces, they are uniformly tan to dark brown but may range from white to black. [7] In our study, 60% (150) of cases had CSK, the commonest of all variants that we had observed. The existing literature mentions that CSK are usually seen after the third decade, whereas the youngest patient with CSK in our study was a 12-year-old female, although only 8.6% of total cases (n= 13) with CSK were in the age group less than 40 years. We also found increased frequency of CSK in males, with a M:F ratio of 1.23:1.
Dermatosis papulosa nigra
DPN are very common among blacks (considered a variant of SK in people with dark skin), and generally manifests at earlier ages than CSK. They are more common among women and present as multiple 1-5 mm large black papules over the face, neck, chest, and upper back. Positive family history is common. [7] In our study, 46.4% (116) of cases (48 males and 68 females, M:F ratio 1:1.42) had DPN with females outnumbering males. The 21.5% of cases (n = 25) with DPN were in the age group less than 40 years. Amongst five cases in our study group who gave family history of SK, four cases had DPN and the only other case was CSK. Our observations regarding DPN are in accordance with the published literature, i.e. they manifest at earlier age than other variants of SK are more common in women, and are associated with higher frequency of positive family history.
Pedunculated seborrheic keratoses
We observed clinically, another group of SK which are brown to black, pedunculated papules, of size 1-5 mm, most commonly in areas of friction, commonly seen on neck and axillae, and categorized them as PSK. In our study, 53 (21.2%) cases (20 males and 33 females, M:F ratio 1:1.65) had PSK with females outnumbering males. The 25% of cases (n = 13) with PSK were in the age group less than 40 years. We observed that both DPN and PSK were common in females, manifesting at earlier ages than other variants of SK.
Flat seborrheic keratoses
Flat SK are benign lesions that typically appear as oval tan-brown patches or macules on sun-exposed areas of the skin, especially on the face, backs of the hands and wrists, extensor surfaces of the forearms, and chest. Flat SK are asymptomatic and increase with the age. [8] In our study, 27 (10.4%) of the cases (14 males and 13 females, M:F ratio 1.07:1) had flat SK with almost equal sex distribution.
Stucco keratoses
White or gray-white verrucous papules are a few millimeters in size, often in large numbers (100 or more) on sun-exposed areas (extensor surface of forearms and lower legs, dorsal aspects of hands and feet), more common in men, and are relatively easily scratched off. [7] There were only five (2%) cases (two males and three females) of stucco keratoses in our study. These lesions were observed on forearms and legs as mentioned in the literature.
Dermoscopy
Dermoscopic findings of SK include ML cysts, CL openings, FR, ME borders, HP blood vessels, FP-like structures, NL structures, and SD. [3]
There are only a few studies on the dermoscopy of SK. Braun et al. [4] evaluated 203 pigmented SK (from 192 patients) and reviewed dermoscopic criteria of pigmented SK. The authors found high prevalence of classic dermoscopic criteria of SK, i.e., CL openings (144 lesions, 70%) and ML cysts (135 lesions, 66%), in addition they suggested four other dermoscopic criteria [fissures (124 lesions, 61%), HP blood vessels (129 lesions, 63%), SD (183 lesions, 90%) and ME border (94 lesions, 46%)] which they considered would improve the diagnostic accuracy and reduce the misclassification into melanocytic lesions. Also the authors suggested that another dermoscopic finding in SK, NL structures (94 lesions, 46%) should not be confused with the typical pigment network as seen in melanocytic lesions. Kopf et al. [8] identified "fat fingers" (thick digitate linear, curvilinear, branched, or oval/circular dermoscopic structures typically seen in SK where they represent the gyri of their cerebriform surfaces) in 44% of the lesions after examining 299 SK and suggested that identification of these structures can be very helpful in the dermoscopic diagnosis of SK, especially when the classic features of SK are absent.
We evaluated the dermoscopic criteria in different clinical variants of SK found in our study. To the best of our knowledge, there has been no such study which had evaluated all these criteria. In this study, we could not see the finding of HP blood vessels in any of our cases, this may be because the skin types of south Indians belong to type 4 or 5, and the blood vessels could not be seen through the brown-colored Asian skin. The specificity of the dermoscopic criteria could not be established since we did not do dermoscopic examination for all the SK in a patient.
The commonest dermoscopic findings seen in CSK (n = 150) were CL (n = 121, 80%), SD (n = 124, 82.6%), and FR (FR) (n = 78.58%) and less common findings were ME (n = 47, 31.3%), ML (n = 36, 24%), and NL (n = 6, 4%). One interesting observation in this study was that ML (31.3%) finding in dermoscopy was not as common as seen in study by Braun et al. (66%). [4]
Flat SK (n = 27) showed prominent dermoscopic findings of NL (n = 24, 88.8%), SD (n = 20, 74%), FP-like structures (n = 15, 55.5%), and CL in only three cases (11%), and other findings were not seen. Stucco keratoses (n = 5) showed NL and SD in all the cases (100%), ML in two cases and ME in one case.
DPN (n = 116) showed only three findings, i.e. CL (n = 95, 85.3%), and FR (n = 91, 78.4%) being the commonest and SD in 20 cases (17 .2%). PSK (n = 53) showed only two findings: FR in all lesions (100%) and CL (n = 34, 64.1%). We noted that both DPN and PSK have prominent dermoscopic findings of FR and CL.
In this study, we also observed dermoscopic finding of white to black, yellowish horn masses with background dermoscopic features of SK-like CL, FR in the lesions which were looking clinically hyperkeratotic (20 cases).
To conclude, as is evident from our study, most of the characteristics of SK are in accordance with the literature published, i.e., SK appear to be more common in middle- and old-aged, with equal sex distribution, predominantly affecting the head, neck, and trunk. The most common clinical variant was CSK (150/250, 60%) followed by DPN (116/250, 46.4%), PSK (53/250, 21.2%), flat SK (27/250, 10.4%), and stucco keratoses (5/250, 2%). Dermoscopy is useful tool to confirm the diagnosis of SK, we could establish that certain dermoscopic findings appear to be consistent with particular clinical variant. Flat SK which were the early lesions of SK had more commonly FP and NL structures, CSK which were more thickened had more commonly CL, FR, and SD. Stucco keratoses showed SD and NL in all. DPN and PSK had in common CL and FR findings which were consistently seen on dermoscopy in both of them.
Limitations
- Small sample size of the stucco keratoses variant.
- The first step in dermoscopy in evaluating pigmented lesions is to determine if a lesion is of melanocytic or nonmelanocytic origin and in this study, we clinically diagnosed the lesions as SK and on dermoscopy we evaluated for the classic criteria (CL, ML) and additional criteria (FR, HP, SD, and ME) which would help in reducing the misclassification into lesions of melanocytic.
| 1. |
Mackie RM, Quinn AG. Non-melanoma skin cancer and other epidermal skin tumours. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed. Oxford: Blackwell Publishing; 2004. p. 36.1-36.50.
th ed. Oxford: Blackwell Publishing; 2004. p. 36.1-36.50.'>[Google Scholar]
|
| 2. |
Thomas VD, Swanson NA, Lee KK. Benign epithelial tumors, hamartomas and hyperplasias. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell D, editors. Fitzpatrick's Dermatology in General Medicine. 7 th ed. New York: McGraw-Hill; 2008. p. 1054-67.
th ed. New York: McGraw-Hill; 2008. p. 1054-67.'>[Google Scholar]
|
| 3. |
Malvehy J, Puig S, Braun RP, Marghoob AA, Kopf AW, editors. Handbook of dermoscopy. 1 st ed. London: Taylor and Francis; 2006. p. 10-20.
[Google Scholar]
|
| 4. |
Braun RP, Rabinovitz HS, Krischer J, Kreusch J, Oliviero M, Naldi L, et al. Dermoscopy of pigmented seborrheic keratoses: A morphological study. Arch Dermatol 2002;138:1556-60.
[Google Scholar]
|
| 5. |
Yeatman JM, Kilkenny M, Marks R. The prevalence of seborrheic keratoses in an Australian population: Does exposure to sunlight play a part in their frequency? Br J Dermatol 1997;131:411-4.
[Google Scholar]
|
| 6. |
Kwon OS, Hwang EJ, Bae JH, Park HE, Lee JC, Youn JI, et al. Seborrheic keratosis in the Korean males: Causative role of sunlight. Photodermatol Photoimmunol Photomed 2003;19:73-80.
[Google Scholar]
|
| 7. |
Noiles K, Vendor R. Are all seborrheic keratoses benign? Review of the typical lesion and its variants. J Cutan Med Surg 2008;12:203-10.
[Google Scholar]
|
| 8. |
Kopf AW, Rabinovitz H, Marghoob A, Braun RP, Wang S, Oliviero M, et al. "Fat fingers:" a clue in the dermoscopic diagnosis of seborrheic keratoses. J Am Acad Dermatol 2006;55:1089-91.
[Google Scholar]
|
Fulltext Views
14,622
PDF downloads
3,700





