Translate this page into:
Standard guidelines for care: Sclerotherapy in dermatology
2 Department of Dermatology, Bangalore Medical College and Research Institute, Bangalore, India
Correspondence Address:
Niti Khunger
Department of Dermatology and STD, VM Medical College and Safdarjang Hospital, New Delhi
India
| How to cite this article: Khunger N, Sacchidanand S. Standard guidelines for care: Sclerotherapy in dermatology. Indian J Dermatol Venereol Leprol 2011;77:222-231 |
Abstract
Definition: Sclerotherapy is defined as the targeted elimination of small vessels, varicose veins and vascular anomalies by the injection of a sclerosant. The aim of sclerotherapy is to damage the vessel wall and transform it into a fibrous cord that cannot be recanalized. It is a simple, cost-effective, efficacious and esthetically acceptable modality for both therapeutic and esthetic purposes. Indications: Therapeutic indications include varicose veins and vascular malformations. Esthetic indications include telangiectasias and reticular veins. In the management of varicose veins, it may need to be combined with other surgical methods of treatment, such as ligation of the saphenofemoral junction, stab ligation of perforators and stripping. A surgical opinion may be necessary. Methodology: A thorough knowledge of the anatomy and physiology of the venous system of the legs, basic principles of venous insufficiency, methods of diagnosis and, in addition, uses, mechanisms of action and complications of sclerosing agents and proper compression techniques are important pre-requisites to successful sclerotherapy. Although various sclerosing agents are available, polidoconal and sodium tetradecyl sulfate are most commonly used. More recently, these sclerosants have been used in microfoam form for increased efficacy. The basic principle of a successful sclerotherapy technique is the use of an optimal volume and concentration of the sclerosant according to the size of the vessel. The sclerosant is injected carefully into the vessel and compression is applied. Contraindications: Contraindications include superficial and deep venous thrombosis, sapheno-femoral junction incompetence, pregnancy, myocardial decompensation, migraine, hypercoagulable state, serious systemic illness, dependency edema, immobility, arterial disease, diabetes mellitus and allergic reactions to sclerosants. Complications: While sclerotherapy is usually a safe procedure, complications may occur due to inappropriate patient selection or improper injection techniques. The complications may be acute or delayed. Complications include hyperpigmentation, matting, local urticaria, cutaneous necrosis, microthrombi, accidental intra-arterial injection, phlebitis, deep vein thrombosis, thromboembolism, scintillating scotomas, nerve damage and allergic reactions. Physician Qualification: Sclerotherapy may be administered by a surgeon or dermatologist who has acquired adequate training during post-graduation or through recognized fellowships and workshops dedicated to sclerotherapy. He should have an adequate knowledge of the anatomy of the venous system, be able to diagnose and manage venous disease and its associated consequences as well as possess the necessary skills to perform the procedures, understand the appropriate indications and limitations, technique modifications and management of the potential adverse sequelae associated with sclerotherapy and also understand the pharmacology of the sclerosing solutions. Facility: The procedure may be performed in the physician's procedure room.Introduction
Sclerotherapy is the injection of a chemical solution (sclerosant) into a vein, damaging the endothelial lining and causing vessel occlusion and the development of fibrous tissue. It is an established procedure used for the treatment of varicose veins, low-flow vascular malformations, symptomatic hemangiomas, benign vascular tumors and telangiectasias.
Sclerotherapy has not been widely practiced in India as yet. This being a conservative and simple procedure, helps to reduce the cost and morbidity associated with surgery. These guidelines seek to establish minimum standards of care to be followed during sclerotherapy.
Rationale and Scope
These guidelines identify the indications and contraindications for sclerotherapy, various agents that can be used, methodology, pre- and post-procedure care, associated complications and expected results.
Definition
Sclerotherapy is defined as the targeted elimination of small vessels, varicose veins and vascular malformations by the injection of a sclerosant into the lumen of the vessel. [1] The aim of sclerotherapy is to damage the vessel wall and transform it into a fibrous cord that cannot be recanalized.
Mechanism of Sclerotherapy
The various sclerosants used cause a marked damage to the endothelium of the vessels and, possibly, of the entire vascular wall. Subsequently, a secondary, local thrombus attached to the vessel wall is generated and the vessel is finally transformed into a fibrous cord, i.e. sclerosis. [1]
The goal of interventional procedure in varicose veins is to normalize the venous physiology. Direct sclerotherapy of an underlying incompetent perforator, even through an ulcer, can be performed. Sclerotherapy in this setting has shown to markedly enhance ulcer healing. Sclerotherapy of the incompetent perforators or superficial varicose veins increases the efficacy of the calf muscle pump, resulting in an improved clearance of extravascular fluid.
Indications
Sclerotherapy may be indicated for therapeutic or cosmetic purposes [Table - 1].
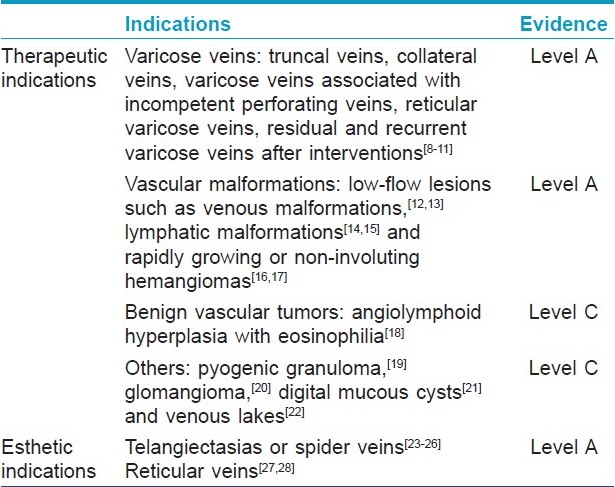
The primary therapeutic indication is the treatment of varicose veins and vascular malformations. Truncal, collateral and reticular varicose veins, varicose veins associated with incompetent perforators and residual or recurrent varicose veins after surgical interventions are amenable to treatment with sclerotherapy. In vascular malformations, sclerotherapy is the therapy of choice for low-flow lesions such as venous and lymphatic malformations.
Background Anatomy and Physiology
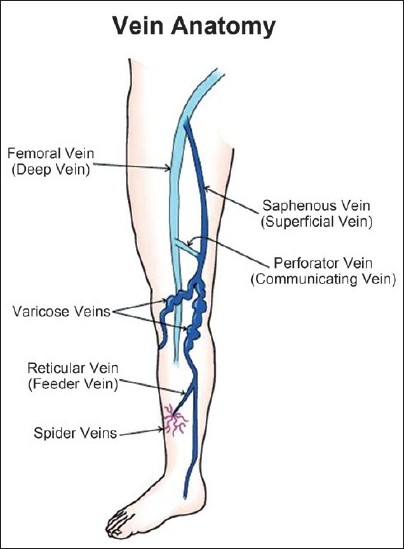
Varicose veins are tortuous, dilated veins often associated with incompetent valves. Telangiectasias are flat, red vessels smaller than 1 mm in diameter. Venules are blue, between 1 and 2 mm, whereas reticular veins are 2-4 mm in diameter. A thorough review of the anatomy and physiology of the venous system of the lower extremity is essential before practicing sclerotherapy. [2]
The lower extremity has a superficial and a deep venous system. The deep venous system includes the femoral, popliteal, anterior tibial, posterior tibial and peroneal veins. The superficial system is extremely variable and includes the great and short saphenous veins and the subdermal lateral venous system. The great and short saphenous veins occasionally connect by the intersaphenous veins. Several communicating vessels, called perforators, are present between the superficial and the deep systems. Occasionally, telangiectasias may communicate directly with the deeper system [Figure - 1].
 |
| Figure 1: Superficial and deep venous systems of lower extremity |
When the calf muscles contract, the valves of the perforating veins and the superficial veins close, forcing blood to flow proximally at a high pressure to the deep venous system. Because of prolonged gravitational hydrostatic pressure, in predisposed individuals, there is a sequential retrograde failure of the venous valves, leading to venous hypertension and varicose veins.
Varicose veins are common and affect 10-20% of the adult population in westernized countries. [3] The incidence of varicose veins increases with each decade of life. [4] Varicose veins may cause significant morbidity, including stasis dermatitis, ankle edema, spontaneous bleeding, superficial thrombophlebitis, recurrent cellulitis, lipodermatosclerosis and ulceration of the ankle and foot. A majority of the patients also have symptoms including pain, cramping, fatigue, restlessness of the legs, dull aching, burning and a sensation of heaviness in the legs. Sclerotherapy is the primary treatment for small vessel varicose disease of the lower extremity, including telangiectasias, venules and reticular veins. [1],[5] Large varicosities do not respond as well as small varicosities to sclerotherapy. The goal of interventional procedures in varicose veins is to normalize the venous physiology. Treatment of telangiectasia is primarily cosmetic. In Caucasians, telangiectasias comprise the most common of all cosmetic complaints, reported in 70% of the women. [3]
Vascular malformations are currently classified as arterial, capillary, venous, lymphatic and combined. They are differentiated from true hemangiomas on the basis of endothelial cell characteristics and the number of mast cells. [6] True hemangiomas often involute with age, while vascular malformations remain stable or slowly grow with the patient, and typically require some form of therapy when cosmetic disfigurement, bleeding or functional impairment occur. From a therapeutic perspective, one of the most important differentiating characteristics of vascular malformations is their classification as "high flow" or "low flow" based on findings at physical examination, imaging or both. [7] Sclerotherapy is indicated in the treatment of low-flow vascular malformations and symptomatic hemangiomas. High-flow vascular lesions do not respond to sclerotherapy alone and require surgical intervention. However, in high-flow lesions, sclerotherapy may be utilized prior to surgery to decrease the size of the vessels and reduce the intraoperative bleeding.
Sclerotherapy is considered to be the first-choice method for the treatment of small intracutaneous varicose veins, including reticular varicose veins and spider veins. [4],[5] Sclerotherapy also enhances healing of venous leg ulcers. [29] Direct sclerotherapy of an underlying incompetent perforator, even through an ulcer, can be performed and has shown to markedly enhance ulcer healing. For the treatment of collateral and incompetent perforating veins, percutaneous phlebextraction and ligation of perforating veins or endoscopic dissection of perforating veins are better treatment options. [30] Surgery is the method of first choice for the treatment of truncal veins with valvular insufficiency. [4]
Vascular malformations do not resolve spontaneously and require treatment. The choice of therapy depends on the affected vessel type, symptoms, size and location of the lesion. Sclerotherapy is mainly indicated for the treatment of low-flow venous and lymphatic malformations. [12],[13],[14],[15] In case of hemangiomas, the current treatment strategy is that any proliferative lesion that carries a risk of ulceration or bleeding or that is rapidly expanding in a cosmetically sensitive area is a candidate for early intervention. Sclerotherapy is indicated for the treatment of large rapidly proliferating or ulcerating hemangiomas. [16],[17]
Limitations
Sclerotherapy is not effective for the treatment of flat portwine stains, high-flow lesions like AV fistulas and large varicose veins with incompetent saphenofemoral junction.
Contraindications
Absolute contraindications [4] :
- Acute superficial or deep vein thrombosis.
- Local infection in the area of sclerotherapy or severe generalized infection.
- Immobility, confinement to bed.
- Advanced peripheral arterial occlusive disease (stage 3 or 4).
- Hyperthyroidism (in the case of sclerosants containing iodine).
- Pregnancy in the first trimester and after the 36 th week of gestation.
- Known allergy to the sclerosant.
- Severe systemic disease.
Relative contraindications:
- Leg edema.
- Sapheno-femoral junction incompetence.
- Thrombophilia with history of deep vein thrombosis.
- Long-standing diabetes.
- Peripheral arterial occlusive disease stage 2.
- Poor general health.
- Myocardial decompensation.
- Migraine.
- Bronchial asthma.
- Marked allergic diathesis.
- Known hypercoagulability.
Sclerotherapy is contraindicated in an immobile patient because ambulation is important to minimize the risks of thrombosis. [4] In diabetes and edema, there is compromised circulation and prolonged healing.
Physician Qualifications
Sclerotherapy may be administered by a dermatologist or a surgeon who has acquired adequate training during post-graduation or through recognized fellowships and workshops dedicated to sclerotherapy.
He should have adequate knowledge of the anatomy of the venous system, be able to diagnose and manage venous disease and its associated consequences as well as possess the necessary skills to perform the procedures, understand the appropriate indications, technique modifications and management of potential adverse sequelae associated with sclerotherapy and also understand the pharmacology of the sclerosing solutions.
Facility
Sclerotherapy can be undertaken in a physician′s office procedure room or minor theater with a high degree of aseptic precautions. A fully equipped minor operation theater with good lighting, appropriate minimal sterilization and storage facilities is desirable.
The main techniques employed in the dermatologist′s office for the treatment of spider veins are sclerotherapy and lasers. For larger varicose veins, dermato-surgeons employ sclerotherapy, ambulatory phlebectomy and endovenous occlusion by laser or radiofrequency. Sclerotherapy is the most frequently used procedure. [2]
Pre-Procedure Assessment
History
A detailed history of the general medical condition, smoking, physical activity, pregnancy and intake of estrogens, hormone replacement therapy, oral contraceptives, aspirin and non-steroidal anti-inflammatory drugs is important. History of Raynaud′s phenomenon or vascular insufficiency and systemic disease such as diabetes mellitus, hypertension, ischemic heart disease should be recorded. Results of previous treatment received for the condition and whether it is a primary or recurrent lesion is also taken.
Examination
Physical examination to assess the skin for evidence of stasis dermatitis, stasis ulcer, examination of the venous system for varicosity, small vessels and large vessels and status of perforators is essential. Examination should include looking for evidence of previous deep vein thrombosis. Arterial pulses should be checked properly. In case of vascular malformation, the extent of malformation, pulsations and whether a bruit is present to rule out an AV fistula is important.
Investigations
The duplex ultrasound (Doppler test) is the most useful tool for workup and has replaced many of the physical examination maneuvers and physiological tests once used for diagnosis. [4] Specific investigations include a Doppler scan of the venous system for location and patency of perforators. Arterial Doppler studies may be carried out if considered necessary. In vascular malformations, a Doppler study indicates the flow of the lesion, whether high flow or low flow. A computed tomography scan or, preferably, a magnetic resonance imaging (MRI) is indicated to assess the extent and depth of the malformation. General investigations such as complete blood counts, bleeding and clotting time, blood sugar and ECG may be carried out.
Documentation of case
Informed consent is essential [Annexure 1][SUPPORTING:1]. Patients should be fully informed of the efficacy, potential side-effects associated with the procedure and chances of recurrence. Clinicians should provide patients with clear written information, including other treatment options. Standardized pre-operative and post-operative photographs should be taken to document the type and extent of the patient′s veins. The operative record should include, at a minimum, the following information: the type, concentration and volume of the sclerosant used and the anatomical site treated (anatomic charts are useful). Complications should be noted and post-operative care advised appropriately.
Counseling
The counseling should include the number of sessions required, duration of treatment, limitations of activity after each session, need for compression therapy and potential adverse events and expected results.
Equipment and Reagents
Materials required for sclerotherapy include selected sclerosant, saline or sterile distilled water for dilution, syringes and needles of appropriate size, cotton rolls or pads and Elastoplast® bandage.
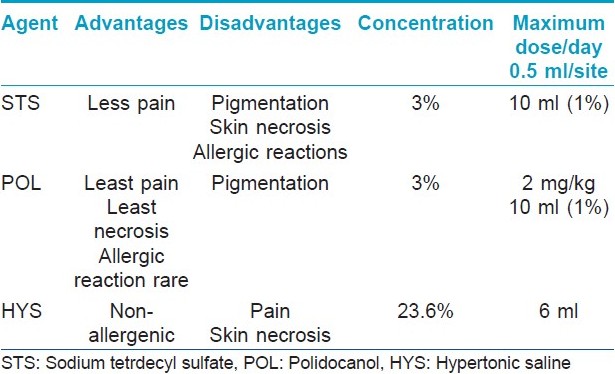
Various sclerosants are given in [Table - 2]. [31]
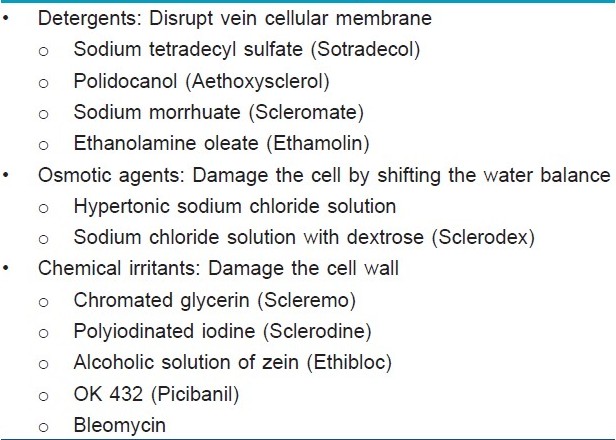
Polidocanol (POL) and sodium tetradecyl sulfate (STS) are the most commonly used sclerosants for their efficacy and safety profile (Level A). These agents are preferred over other agents because they have a very low incidence of allergic reactions, produce a low incidence of pigmentation and other adverse cutaneous effects and fewer complications if extravasated. [2] Studies show no significant differences in the efficacy between the two agents. [32] Other agents, including sodium morrhuate, ethanolamine oleate, OK 432 (picibanil), bleomycin and intravenous doxycycline, have been used as sclerosing agents, predominantly for venous malformations. [33] Hypertonic saline (20% or 23.4% solution) was previously popular for sclerosis of telangiectatic leg veins, but it causes pain and burning and, almost invariably, causes significant necrosis if extravasated. [33] Another sclerosant, 72% chromated glycerin [34] (Scleremo) is very popular in Europe for the treatment of small vessels. It has not yet been Food and Drug Administration (FDA) approved for use in the United States.
The choice of the sclerosant depends on the availability and experience of the treating physician. [2]
In Germany, only one sclerosant is approved for the sclerotherapy of varicose veins, i.e. POL. In the US, STS, sodium morrhuate and ethanolamine oleate were all developed prior to the establishment of the FDA. These agents have never been submitted to the FDA for approval, but they are available as traditional agents. Hypertonic saline 23.4% concentration is approved by the US FDA, but its use in sclerotherapy is off-label. The approval of POL has been recently obtained.
Procedure
Both the physician and the patient should be comfortable and proper lighting should be available. The area to be treated is exposed adequately and cleaned thoroughly with spirit or povidone iodine. Usually, anesthesia, either intralesional or topical, is not required, except for large vascular malformations that may require sedation or general anesthesia. An anxious patient is counseled and an analgesic or antianxiety drug may be administered. A test dose is not recommended as there is a very low risk of allergy.
The sclerosant is diluted to the required concentration with distilled water or saline and loaded in a syringe. Readymade dilutions are not available in India and hence sclerosants have to be diluted to the required concentrations [Table - 3].
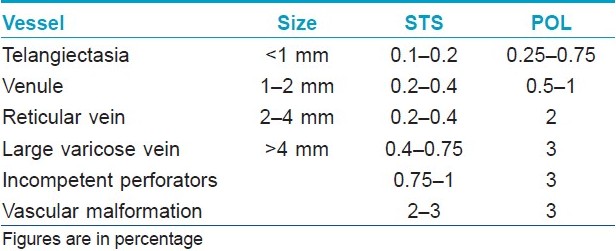
It is carefully injected into the vessel using a 30-gauge needle (for small telangiectasias), with the bevel pointing upward. Before injecting, one must ensure that the tip of the needle is in the lumen of the vessel by aspiration of blood. The quantity of injection varies from 0.1 to 0.5 ml for small veins; for larger veins, a larger volume is required or sclerosants may be injected in the foam form.
The injection should be slow and steady. Severe pain or burning is often a sign of extravasation. In such cases, the site is injected with normal sodium chloride solution or lidocaine to dilute the sclerosant.
The basic principle of treatment is to begin injection into the largest vein and then into the small varicosities. After injection, the site is compressed with cotton balls and tape followed by compression garments.
In low-flow vascular malformations, the preferred method of injection is under color duplex ultrasound-guided or MRI-guided sclerotherapy. Using real-time sonographic guidance, lesions are punctured percutaneously with a 20/21-gauge needle. The quantity of the sclerosant and the number of sites injected depends on the size and location of the vascular malformation. The maximum dosage of the sclerosant should not be exceeded [Table - 4]. The maximum dosage for POL is 2 mg/kg and for STS is 10 ml of 3% solution. Initially, it is preferable to inject a lower concentration and a lower dose to avoid unexpected reactions.
The procedure may be performed in multiple sittings. Treatment intervals may vary, but allowing 4-8 weeks between treatments helps to minimize the number of necessary sessions. The number of sittings depends on the response, concentration of sclerosant, volume used and skill of the operator.
Post-Procedure Care
Immediately after the injection, compression is given by a cotton ball and taped at the site of injection and a compression bandage using Elastoplast; . Post-treatment compression consists of a graduated 20-30 mmHg support hose for 2 weeks for larger veins and 16 mmHg compression for smaller veins. The duration of compression after the sclerotherapy depends on the size of the vessel injected, and varies from 1 day for spider veins to 3 weeks for the larger veins, although there is no consensus on this issue. [35],[36] Patients should also be instructed to walk for 30 min after the procedure and daily for the next few days. Intensive workouts, heavy exercise, hot baths, strong UV radiation as well blood thinners like aspirin should be avoided for a few days.
Special Techniques of Sclerotherapy
Sclerotherapy guided by duplex ultrasonography [37],[38]
This technique is particularly recommended when sclerosing saphenous junctions, truncal veins next to the saphenous junctions, perforating veins and low-flow vascular malformations. The vein is visualized by duplex ultrasonography in the lying down patient and is punctured during visualization. The needle is visible in the ultrasound image and the intravascular injection can be controlled. The aim of this method is to achieve a controlled procedure that results in fewer complications and an increased effect.
Foam sclerotherapy [39],[40],[41],[42]
This is a technique in which the liquid sclerosant is mixed with air to form a foam, which is then injected into the vessel. Although an old technique, it was reintroduced by Cabrrera in the early 1990s. [39] Tessari developed an easy way of making foam by using two syringes and a three-way stopcock. [40] It is becoming an increasingly popular technique in the treatment of varicose and reticular veins, especially those greater than 1 mm in diameter. The advantages of using foam sclerotherapy include increase in contact between the sclerosing solution and the vessel wall, decrease in dilution of the sclerosing agent secondary to displacement of blood and an increase in the amount of contact time between the sclerosant and the vein. Foam also has the benefit of creating a more uniform distribution of sclerosing solution within the venous system, with decreased side-effects. Therefore, a lower amount and a lower concentration of the sclerosing agent are needed compared with a liquid sclerosant. [39],[40],[41],[42] Foam can be prepared by mixing carbon dioxide (Varisolve; ) [43] or air. In the technique using air, 1 ml of the sclerosing agent is taken up in a 5 cc syringe and connected to another 5 cc syringe containing 4 cc of room air through a three-way stopcock. The sclerosant is pumped into the syringe containing room air and then pumped back using the connector. This is repeated 10 times to get a good foam. It is then immediately injected into the vessel. Compression bandage is applied after the procedure.
Efficacy
The results of sclerotherapy depend on the technique, the sclerosant used and the diameter of the vein. [4],[45],[46]
Sclerotherapy is considered to be the standard treatment or treatment of choice for intracutaneous varicose veins (spider veins and reticular veins), achieving an improvement of up to 80% or 90%. [4],[8],[30] Compression treatment with stockings may further improve the result of the treatment of spider veins and reduce the occurrence of hyperpigmentation. [35],[36]
In the treatment of saphenous veins, good results can be achieved by duplex-guided sclerotherapy with and without foam. [4],[38],[39] However, foam sclerotherapy is considered to be more efficacious as compared with liquid sclerotherapy in the treatment of larger veins. [38],[45] In vascular malformations, although surgical excision is the standard method for the treatment, it often leads to a loss of motor function, nerve damage and massive bleeding if the excision is extensive. Sclerotherapy is an alternative and superior method of treatment, particularly for large lesions. [46]
The advantages of sclerotherapy are that, unlike surgery, it is a minimally invasive procedure that can be performed in the outpatient clinic and there is no need for hospitalization or an anesthetic. There is no surgical scarring and virtually no downtime.
Complications and risks [4],[47],[48],[49],[50],[51],[52]If performed properly with due precautions, sclerotherapy is an efficient treatment method with a low incidence of complications. The following complications can occur:
- Allergic reaction.
- Pigmentation.
- Skin necroses.
- Excessive sclerosing reaction (thrombophlebitis).
- Matting.
- Nerve damage.
- Scintillating scotomas.
- Orthostatic collapse.
- Thromboembolism.
Allergic reactions including anaphylactic shock are rare complications. Inadvertent intra-arterial injections are complications constituting an emergency situation. Hyperpigmentation is more common, with a frequency of 0.3-10%. [47] A percutaneous injection of sclerosing agents has a relatively long history of safe application for the treatment of low-flow vascular malformations. Few complications have been reported with this form of therapy, including skin necrosis, small skin ulcers, urticarial reactions, scarring, allergic reactions and a case of reversible cardiac arrest following injection of large volumes of POL in a child. [51]
In a review of 69 studies with foam sclerotherapy, the median rates of serious adverse events, including pulmonary embolism and deep vein thrombosis, were <1%. [49] The median rate of visual disturbance was 1.4%, headache 4.2%, thrombophlebitis 4.7%, matting/skin staining/pigmentation 17.8% and pain at the site of injection 25.6%.
Alternative Procedures
Conservative treatment
Compression stockings may improve the symptoms of varicose veins. However, if symptoms persist, then procedural treatment is indicated.
Surgery
The surgical treatments for varicose veins are stripping and ligation of the long or short saphenous veins and ambulatory phlebectomy. In a randomized comparative trial of compression sclerotherapy and ambulatory phlebectomy, the recurrence rates were lower with surgery but the incidence of complications was higher as compared with sclerotherapy. [53]
Endovenous ablation by laser or radiofrequency
In this technique, the vascular endothelium is destroyed by a laser fiber or radiofrequency that is passed through a long catheter along the entire length of the truncal varicosity to be ablated. Under ultrasound guidance, a tumescent solution with a local anesthetic is injected around the entire length of the vessel, which also insulates the heat from damaging the adjacent structures, including nerves and skin as well as pain control. Firm pressure is applied to collapse the vein around the laser fiber and the laser is fired, generating heat, leading to irreversible endothelial damage and thrombosis. [54]
In radiofrequency ablation, thermal energy is delivered directly to the vessel wall, causing immediate closure of the vessel. In contrast to laser therapy, the RF catheter actually comes into contact with the lumen walls. [55]
Sclerotherapy can also be combined with radiofrequency ablation to hasten resolution. [56]
Laser therapy
Vascular lasers such as the pulsed dye laser and long-pulsed Nd:YAG laser have been used for the treatment of telangiectasias. In one small study of 14 patients, no statistically significant difference in results was found between a comparison and sequential study of the long-pulsed Nd:YAG 1,064 nm laser and sclerotherapy in the leg telangiectasias treatment. [57] Endovenous lasers and radiofrequency energy, although expensive, are alternative emerging therapies. Sclerotherapy is a well-known, cost-effective technique with many controlled trials.
Conclusion
Sclerotherapy is a simple and effective office procedure for the treatment of varicose veins and low-flow vascular malformations. It is the treatment of choice for spider veins or telangiectasia over the legs and is indicated in the treatment of reticular and short saphenous varicose veins. It is considered superior to surgical and non-surgical treatments to relieve the symptoms and reach optimal cosmetic results for small, localized, primary varices of the lower extremity. There is currently no consensus on the place of sclerotherapy in the treatment of the long saphenous vein and incompetent perforating veins. [24] The advantages of sclerotherapy are low morbidity, almost no mortality and no necessity for hospitalization; therefore, avoiding loss of work time. [7] However, proper training in the technique, dilution and amount of sclerosant injected is vital for optimal, risk-free outcomes.
Acknowledgements
Dr. Dinker B Rai, Chief of Department of Vascular Surgery and Vascular Laboratory, Interfaith Medical Centre, Brooklyn, USA for his review and advice regarding the draft of this article.
| 1. |
Scurr JH. Venous disorders. In: Russell RC, Williams NS, Bulstrode CJ, editors. Bailey and Love's short practice of surgery. 24 th ed. London: Arnold Publishers; 2004. p. 956.
th ed. London: Arnold Publishers; 2004. p. 956. '>[Google Scholar]
|
| 2. |
Lee AJ, Evans CJ, Allan PL, Ruckley CV, Fowkes FG. Lifestyle factors and the risk of varicose veins: Edinburgh Vein Study. J Clin Epidemiol 2003;56:171-9.
[Google Scholar]
|
| 3. |
Weiss RA, Weiss MA. Treatment of varicose and telangiectatic veins. In: Freedberg JM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's dermatology in general medicine. 6 th ed. USA: McGraw Hill Publishers; 2009. p. 2549-56.
th ed. USA: McGraw Hill Publishers; 2009. p. 2549-56.'>[Google Scholar]
|
| 4. |
Rabe E, Pannier-Fischer F, Gerlach H, Breu FX, Guggenbichler S, Zabel M; et al. Guidelines for sclerotherapy of varicose veins (ICD 10: I83.0, I83.1, I83.2, and I83.9). Dermatol Surg 2004;30:687-93; discussion 693.
[Google Scholar]
|
| 5. |
Tisi PV, Beverley C, Rees A. Injection sclerotherapy for varicose veins. Cochrane Database Syst Rev 2006;4:CD001732.
[Google Scholar]
|
| 6. |
Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-22.
[Google Scholar]
|
| 7. |
O'Donovan JC, Donaldson JS, Morello FP, Pensler JM, Vogelzang RL, Bauer B. Symptomatic hemangiomas and venous malformations in infants, children, and young adults: Treatment with percutaneous injection of sodium tetradecyl sulfate. AJR Am J Roentgenol 1997;169:723-9.
[Google Scholar]
|
| 8. |
Guidelines of care for sclerotherapy treatment of varicose and telangiectatic leg veins. American Academy of Dermatology. J Am Acad Dermatol 1996;34:523-8.
[Google Scholar]
|
| 9. |
Smith PC. Foam and liquid sclerotherapy for varicose veins. Phlebology 2009;24:62-72.
[Google Scholar]
|
| 10. |
Kahle B, Leng K. Efficacy of sclerotherapy in varicose veins-prospective, blinded, placebo-controlled study. Dermatol Surg 2004;30:723-8; discussion 728.
[Google Scholar]
|
| 11. |
Green D. Sclerotherapy for the permanent eradication of varicose veins: Theoretical and practical considerations. J Am Acad Dermatol 1998;38:461-75.
[Google Scholar]
|
| 12. |
Yamaki T, Nozaki M, Sasaki K. Color duplex-guided sclerotherapy for the treatment of venous malformations. Dermatol Surg 2000;26:323-8.
[Google Scholar]
|
| 13. |
Lee BB, Do YS, Byun HS, Choo IW, Kim DI, Huh SH. Advanced management of venous malformation with ethanol sclerotherapy: Mid-term results. J Vasc Surg 2003;37:533-8.
[Google Scholar]
|
| 14. |
Kim KH, Sung MW, Roh JL, Han MH. Sclerotherapy for congenital lesions in the head and neck. Otolaryngol Head Neck Surg 2004;131:307-16.
[Google Scholar]
|
| 15. |
Acevedo JL, Shah RK, Brietzke SE. Nonsurgical therapies for lymphangiomas: A systematic review. Otolaryngol Head Neck Surg 2008;138:418-24.
[Google Scholar]
|
| 16. |
Winter H, Drager E, Sterry W. Sclerotherapy for treatment of hemangiomas. Dermatol Surg 2000;26:105-8.
[Google Scholar]
|
| 17. |
Matsumoto K, Nakanishi H, Koizumi Y, Seike T, Kanda I, Kubo Y. Sclerotherapy of hemangioma with late involution. Dermatol Surg 2003;29:668-71.
[Google Scholar]
|
| 18. |
Khunger N, Pahwa M, Jain RK. Angiolymphoid hyperplasia with eosinophilia treated with a novel combination technique of radiofrequency ablation and sclerotherapy. Dermatol Surg 2010;36:422-5.
[Google Scholar]
|
| 19. |
Matsumoto K, Nakanishi, H, Seike T, Koizumi Y, Mihara K, Kubo Y. Treatment of pyogenic granuloma with a sclerosing agent. Dermatol Surg 2001;27:521-3.
[Google Scholar]
|
| 20. |
Parsi K, Kossard S. Multiple hereditary glomangiomas: Successful treatment with sclerotherapy. Australas J Dermatol 2002;43:43-7.
[Google Scholar]
|
| 21. |
Córdoba S, Romero A, Hernández-Nuñez A, Borbujo JM. Treatment of digital mucous cysts with percutaneous sclerotherapy using polidocanol. Dermatol Surg 2008;34:1387-8.
[Google Scholar]
|
| 22. |
Kuo HW, Yang CH. Venous lake of the lip treated with a sclerosing agent: Report of two cases. Dermatol Surg 2003;29:425-8.
[Google Scholar]
|
| 23. |
McCoy S, Evans A, Sprurrier N. Sclerotherapy for leg telangiectasia: A blinded comparative trial of polidocanol and hypertonic saline. Dermatol Surg 1999;25:381-6.
[Google Scholar]
|
| 24. |
Kern P, Ramelet AA, Wutschert R, Bouname H, Hayoz D. Single-blind, randomized study comparing chromated glycerin, polidocanol solution, and polidocanol foam for treatment of telangiectatic leg veins. Dermatol Surg 2004;30:367-72.
[Google Scholar]
|
| 25. |
Misirlioglu A, Gideroglu K, Akan M, Akoz T. Using silicone gel sheet for the treatment of facial telangiectasias with sclerotherapy. Dermatol Surg 2004;30:373-7.
[Google Scholar]
|
| 26. |
Goldman MP, Weiss RA, Brody HJ, Coleman WP, Fitzpatrick RE. Treatment of facial telangiectasia with sclerotherapy, laser surgery, and/or electrodesiccation: A review. J Dermatol Surg Oncol 1993;19:899-906.
[Google Scholar]
|
| 27. |
Bowes LE, Goldman MP. Sclerotherapy of reticular and telangiectatic veins of the face, hands, and chest. Dermatol Surg 2002;28:46-51.
[Google Scholar]
|
| 28. |
Goldman PM. Polidocanol (aethoxysklerol) for sclerotherapy of superficial venules and telangiectasias. J Dermatol Surg Oncol 1989;15:204-9.
[Google Scholar]
|
| 29. |
Hertzman PA, Owens R. Rapid healing of chronic venous ulcers following ultrasound-guided foam sclerotherapy. Phlebology 2007;22:34-9.
[Google Scholar]
|
| 30. |
Einarsson E, Eklo FB, Negle NP. Sclerotherapy or surgery as treatment for varicose veins: A prospective randomized study. Phlebology 1993;8:22-6.
[Google Scholar]
|
| 31. |
Parsons ME. Sclerotherapy basics. Dermatol Clin 2004;22:501-8.
[Google Scholar]
|
| 32. |
Goldman MP. Treatment of varicose and telangiectatic leg veins: Double-blind prospective comparative trial between aethoxyskerol and sotradecol. Dermatol Surg 2002;28:52-5.
[Google Scholar]
|
| 33. |
Feied CF. Sclerosing solutions. In: Fronek H, editor. The fundamentals of phlebology, venous disease for clinicians. 2 nd ed. USA: American College of Phlebology Publishing; 2007 Ch.5. p. 23.
[Google Scholar]
|
| 34. |
Kern P, Ramelet AA, Wutschert R, Bounameaux H, Hayoz D. Single-blind, randomized study comparing chromated glycerin, polidocanol solution, and polidocanol foam for treatment of telangiectatic leg veins. Dermatol Surg 2004;30:367-72.
[Google Scholar]
|
| 35. |
Goldman MP. How to utilize compression after sclerotherapy. Dermatol Surg 2002;28:860-2.
[Google Scholar]
|
| 36. |
Nootheti P, Cadag KM, Magpantay A, Goldman MP. Efficacy of graduated compression stockings for an additional 3 weeks after sclerotherapy treatment of reticular and telangiectatic leg veins. Dermatol Surg 2009;35:53-8.
[Google Scholar]
|
| 37. |
Yamaki T, Nozaki M, Sasaki K. Color duplex-guided sclerotherapy for the treatment of venous malformations. Dermatol Surg 2000;26:323-8.
[Google Scholar]
|
| 38. |
Yamaki T, Nozaki M, Iwasaka S. Comparative study of duplex-guided foam sclerotherapy and duplex-guided liquid sclerotherapy for the treatment of superficial venous insufficiency. Dermatol Surg 2004;30:718-22.
[Google Scholar]
|
| 39. |
Frullini A, Cavezzi A. Sclerosing foam in the treatment of varicose veins and telangiectases: History and analysis of safety and complications. Dermatol Surg 2002;28:11-5.
[Google Scholar]
|
| 40. |
Tessari L, Cavezzi A, Frullini A. Preliminary experience with a new sclerosing foam in the treatment of varicose veins. Dermatol Surg 2001;21:58-60.
[Google Scholar]
|
| 41. |
Cabrera J, Redondo P, Becerra A, Garido C, Cabrera J Jr, Garcia MA, et al Ultrasound guided injection of Polidocanol microfoam in the management of venous leg ulcers. Arch Dermatol 2004;140:667-73.
[Google Scholar]
|
| 42. |
Breu FX, Guggenbichler S. European consensus meeting on foam sclerotherapy. Dermatol Surg 2004;30:709-17.
[Google Scholar]
|
| 43. |
Wright D, Gobin JP, Bradbury AW, P Coleridge-Smith, Spoelstra H, Berridgeet D, et al. Varisolve® polidocanol microfoam compared with surgery or sclerotherapy in the management of varicose veins in the presence of trunk vein incompetence: European randomized controlled trial. Phlebology 2006;21:180-90.
[Google Scholar]
|
| 44. |
Rigby KA, Palfreyman SJ, Beverley C, Michaels JA. Surgery versus sclerotherapy for the treatment of varicose veins. Updated November 15, 2005. Cochrane Database Syst Rev 2006;4:CD004980.
[Google Scholar]
|
| 45. |
Belcaro G, Cesarone MR, Di Renzo A, Brandolini R, Coen L, Acerbi G, et al. Foam-sclerotherapy, surgery, sclerotherapy, and combined treatment for varicose veins: A 10 year, prospective, randomized, controlled trial (VEDICO trial). Angiology 2003;54:307-15.
[Google Scholar]
|
| 46. |
Cabrera J, Cabrera J Jr, Garcia-Olmedo MA, Redondo P. Treatment of venous malformations with sclerosant in microfoam form. Arch Dermatol 2003;139:1409-16.
[Google Scholar]
|
| 47. |
Guex JJ, Allaert FA, Gillet JL, Chlier F. Immediate and midterm complications of sclerotherapy report of a prospective multi-center registry of 12,173 sclerotherapy sessions. Dermatol Surg 2005;31:123-8.
[Google Scholar]
|
| 48. |
Goldman MP, Sadick NS, Weiss RA. Cutaneous necrosis, telangiectatic matting and hyperpigmentation following sclerotherapy. Dermatol Surg 1995;21:19-29.
[Google Scholar]
|
| 49. |
Jia X, Mowatt G, Burr JM, Cassar K, Cook J, Fraser C. Systematic review of foam sclerotherapy for varicose veins. Br J Surg 2007;94:925-36.
[Google Scholar]
|
| 50. |
Bush RG, Derrick M, Manjoney D. Major neurological events following foam sclerotherapy. Phlebology 2008;23:189-92.
[Google Scholar]
|
| 51. |
Marrocco-Trischitta MM, Guerrini P, Abeni D, Stillo F. Reversible cardiac arrest after polidocanol sclerotherapy of peripheral venous malformation. Dermatol Surg 2002;28:153-5.
[Google Scholar]
|
| 52. |
Bihari I, Magyar E. Reasons for ulceration after injection treatment of telangiectasia. Dermatol Surg 2001;27:133-6.
[Google Scholar]
|
| 53. |
De Roos KP, Nieman FH, Neumann HA. Ambulatory phlebectomy versus compression sclerotherapy: Results of a randomized controlled trial. Dermatol Surg 2003;29:221-6.
[Google Scholar]
|
| 54. |
Hamel-Desnos C, Gérard JL, Desnos P. Endovenous laser procedure in a clinic room: feasibility and side effects study of 1700 cases. Phlebology 2009;24:125-30.
[Google Scholar]
|
| 55. |
Gohel MS, Davies AH. Radiofrequency ablation for uncomplicated varicose veins. Phlebology 2009;24:42-9.
[Google Scholar]
|
| 56. |
Khunger N. Acquired lymphangiectasis of vulva: A novel therapeutic approach with combination of radiofrequency and sclerotherapy. J Cutan Aesth Surg 2009;2:33-5.
[Google Scholar]
|
| 57. |
Levy JL, Elbahr C, Jouve E, Mordon S. Comparison and sequential study of long pulsed Nd:YAG 1,064 nm laser and sclerotherapy in leg telangiectasias treatment. Lasers Surg Med 2004;34:273-6.
[Google Scholar]
|
Fulltext Views
22,209
PDF downloads
6,544





