Translate this page into:
Stratum corneum findings as clues to histological diagnosis of pityriasis lichenoides chronica
Correspondence Address:
Rajiv Joshi
Consultant Dermatologist and Dermato-pathologist, P. D. Hinduja Hospital and Medical Research Centre, Mahim, Mumbai 16
India
| How to cite this article: Joshi R. Stratum corneum findings as clues to histological diagnosis of pityriasis lichenoides chronica. Indian J Dermatol Venereol Leprol 2008;74:156-157 |
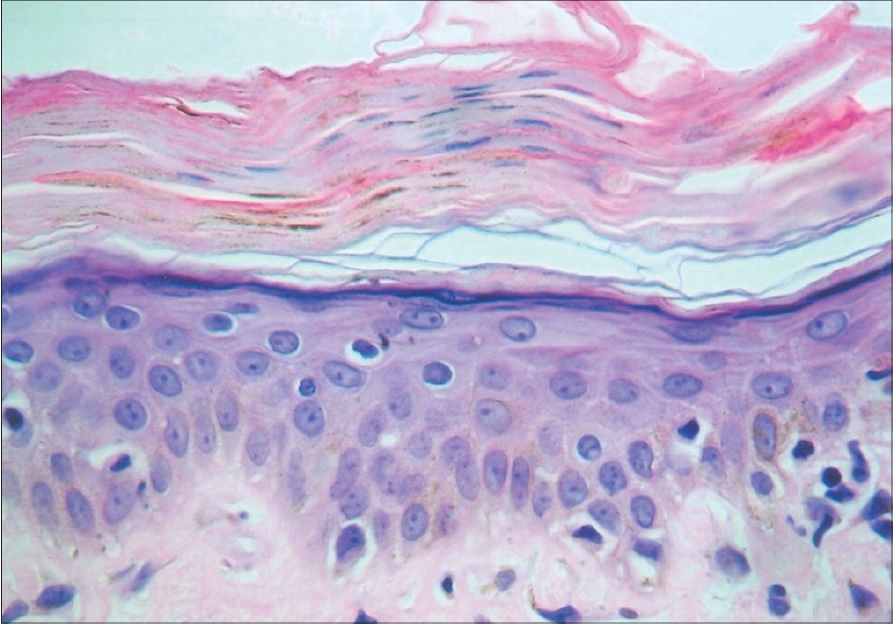 |
| Figure 3: Thick laminated stratum corneum with layered parakeratosis and abundant melanin (H and E, �400) |
 |
| Figure 3: Thick laminated stratum corneum with layered parakeratosis and abundant melanin (H and E, �400) |
 |
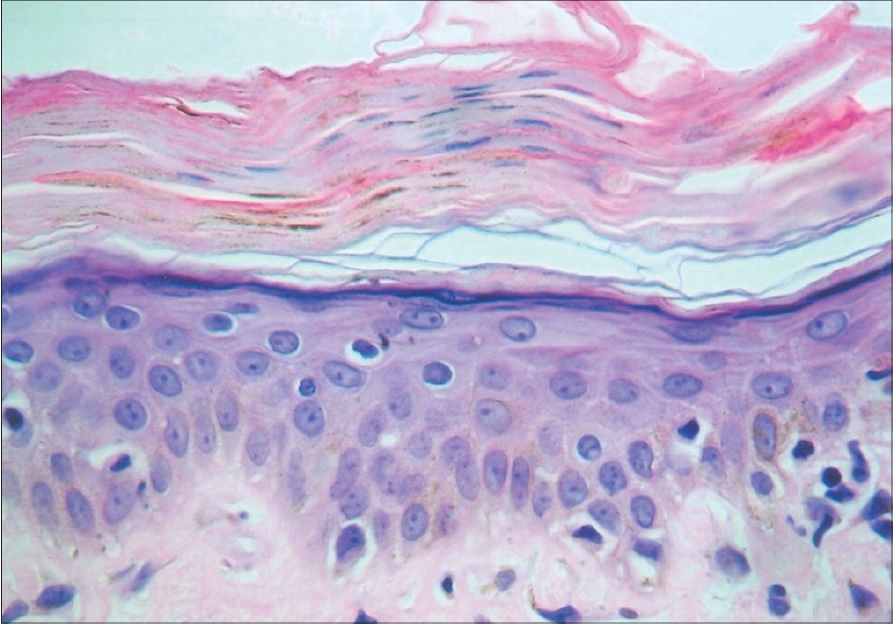
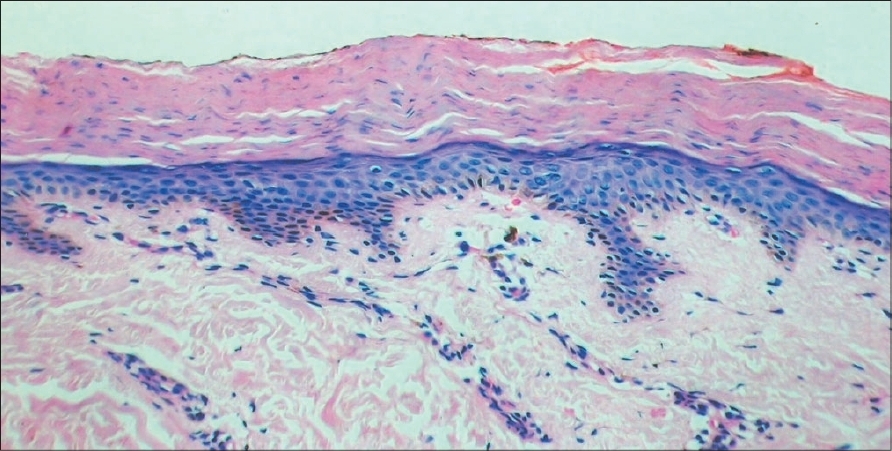
| Figure 2: Bright pink horny layer with thin, flat parakeratosis in foci and flecks of melanin. Also seen are erythrocytes within the epidermis (H and E, �200) |
 |
| Figure 2: Bright pink horny layer with thin, flat parakeratosis in foci and flecks of melanin. Also seen are erythrocytes within the epidermis (H and E, �200) |
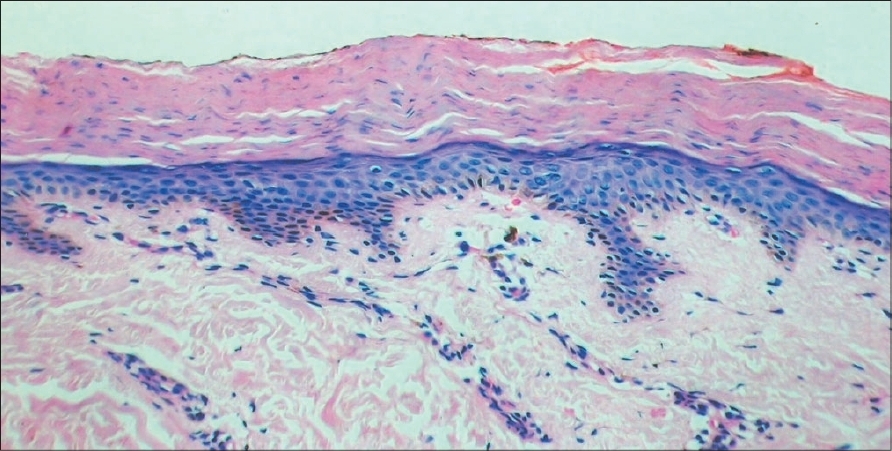 |
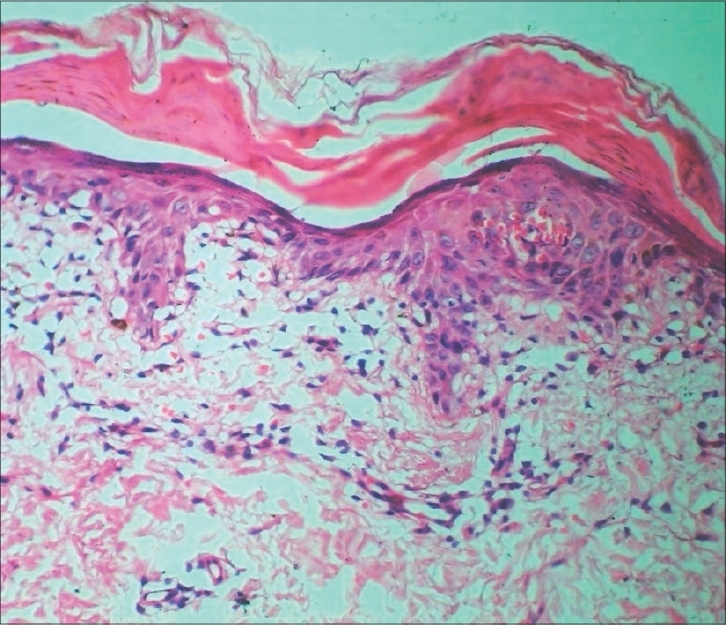
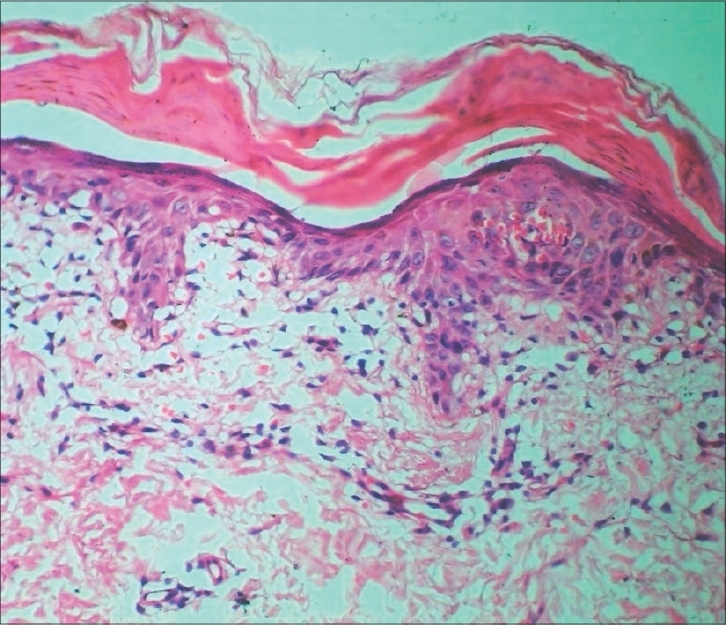
| Figure 1: Thick laminated stratum corneum with confluent parakeratosis overlying a well developed granular layer |
 |
| Figure 1: Thick laminated stratum corneum with confluent parakeratosis overlying a well developed granular layer |
Sir,
This letter is in response to the article, "A clinical and histopathological study of pityriasis lichenoides" by Nair PS. [1] The author mentions that basal cell vacuolization and perivascular infiltrate were parameters considered mandatory for the histological diagnosis of pityriasis lichenoides. Thus, cases clinically diagnosed as pityriasis lichenoides et varioliformis acuta (PLEVA)/pityriasis lichenoides chronica (PLC) but not having basal cell vacuolization and perivascular infiltrate were excluded from the study. It would be interesting to know the percentage of such patients because in practice, many cases that are clinically diagnosed as PLC do not always show basal cell vacuolization. Furthermore, if the criterion of basal cell vacuolization is applied strictly for the diagnosis of PLC, many of these cases would not be diagnosed as PLC.
The histological findings in PLC are irregular, psoriasiform, epidermal hyperplasia with a superficial perivascular, lymphocytic infiltrate and a few melanophages. [2] Interface changes with few lymphocytes in the lower epidermis that obscure the dermo-epidermal interface with mild spongiosis and some vacuolization of basal keratinocytes are seen in early developing lesions. Unlike PLEVA, extravasated erythrocytes in the upper dermis and within the epidermis, individually necrotic keratinocytes (apoptotic keratinocytes) and ballooning of keratinocytes are rarely seen. The granular layer is usually well developed unlike psoriasis.
Pityriasis lichenoides (both the acute form known eponymically as Mucha-Habermann disease and the chronic form also known as Juliusberg disease) are examples of interface dermatitis and basal cell vacuolization is an expected finding along with other changes that characterize such dermatitides. These changes include lymphocytes obscuring the dermo-epidermal junction, individually necrotic (apoptotic) keratinocytes at the dermo-epidermal junction and also scattered higher up in the epidermis and in the more acute cases, patchy or confluent necrosis of the epidermis.
The interface changes are however, time-dependent and become less prominent as the lesion ages and may not be seen at all in fully developed or regressing lesions, especially in PLC. Clinically, these lesions develop a thick, wafer-like scale adherent in the center of the papule and later heal with hypopigmentation and some scaling. Biopsies taken at these moments in the evolution of the disease often do not show any interface changes or basal cell vacuolization.
Stratum corneum findings, however, may be quite striking and give a clue to the diagnosis of PLC at this stage. The stratum corneum is prominently thickened, laminated, bright pink, almost ′ichthyosiform′ in appearance and houses parakeratosis and flecks of melanin. The parakeratotic nuclei are thin and flat and arranged in layers. The parakeratosis may be very focal and easily missed on scanning magnification or may be extensive and confluent [Figure - 1],[Figure - 2],[Figure - 3].
Stratum corneum changes similar to those described above may uncommonly be seen in lesions of pityriasis rubra pilaris (PRP). In PRP, the parakeratosis assumes a checkerboard appearance with horizontal and vertical tiers of thin, flat, parakeratotic nuclei but melanin is not seen in the stratum corneum.
In sum, if basal cell vacuolization and interface changes are not present in a given section of a biopsy from a patient suspected clinically to have pityriasis lichenoides chronica, the histological findings of a thick, laminated, brightly eosinophilic, horny layer with parakeratosis and flecks of melanin are clues to an old lesion of pityriasis lichenoides.
| 1. |
Nair PS. A clinical and histopathological study of pityriasis lichenoides. Indian J Dermatol Venereol Leprol 2007;73:100-2.
[Google Scholar]
|
| 2. |
Weedon D. Pityriasis lichenoides in vasculopathic reaction pattern. Skin Pathology, Churchill-Livingstone: 1997. p. 209-10.
[Google Scholar]
|
Fulltext Views
5,906
PDF downloads
1,908





