Translate this page into:
Subungual mass in a patient of xeroderma pigmentosum: Looking beyond malignant transformation
Corresponding author: Dr. Neetu Bhari, Department of Dermatology and Venereology, AIIMS, New Delhi, India. drntbhari@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ahuja R, Kumar D, Arava S, Bhari N. Subungual mass in a patient of xeroderma pigmentosum: Looking beyond malignant transformation. Indian J Dermatol Venereol Leprol. 2024;90:806-8. doi: 10.25259/IJDVL_944_2023
Dear Editor,
A 16-year-old girl, with a known case of xeroderma pigmentosum, presented with a slowly progressive firm, non-tender skin-coloured subungual plaque in the middle finger of her left hand for the past 4 years. The plaque appeared to arise from the underlying nail bed, causing the nail plate to lift with a concave dorsal curvature [Figure 1]. Subungual yellowish to dark brown hyperkeratotic debris was present in a few other fingernails. Onychoscopic evaluation of the subungual mass showed whitish-yellow structureless areas, arranged in a whorled pattern with adherent whitish scaling [Figure 2]. KOH microscopy from the subungual debris did not show any hyphae. On the face, there were some hyperpigmented papulo-nodules and barely elevated plaques with fine overlying scaling and haemorrhagic crusting, in a background of hyper- and hypopigmented macules. These nodules had shown features of basal cell carcinoma on histological evaluation. She had a history of photosensitivity and a tendency of keloid formation. Her two younger sisters also had xeroderma pigmentosum. There was no history of consanguinity or similar complaints in other family members. The patient did not recall any significant trauma before the appearance of the nail changes. A 4 mm punch biopsy was perfomed from the subungual mass considering subungual fibroma, fibrokeratoma and keratoacanthoma as clinical differentials.

- Skin--coloured, firm subungual plaque lifting the nail plate in the middle finger of the left hand.
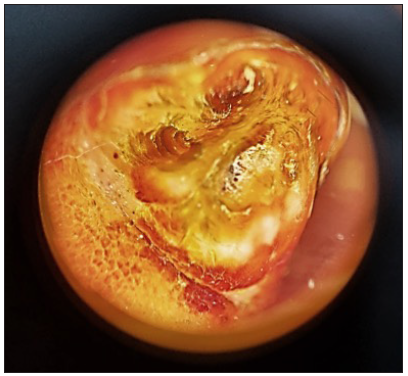
- On onychoscopy, whitish yellow structureless areas, somewhat arranged in a whorled pattern with adherent whitish scaling were seen (Heine Delta 20T, magnification 10x).
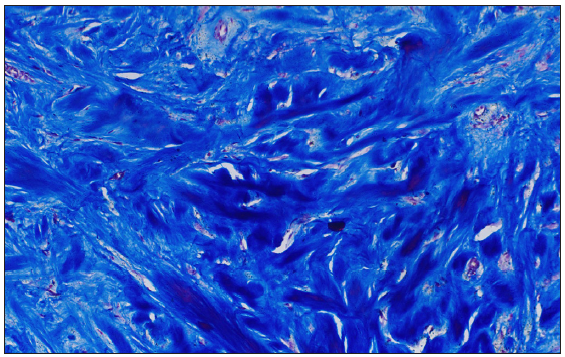
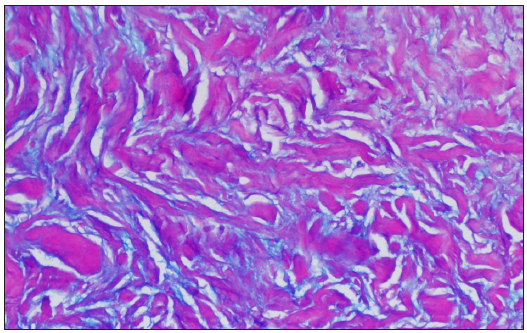
Histopathological evaluation of the subungual mass showed a hyperkeratotic stratum corneum with fibroblastic proliferation in the dermis. There were haphazardly arranged bundles of homogeneously eosinophilic thick collagen, with the presence of mucin between the collagen bundles in a few areas, more apparent on alcian blue. The thick collagen bundles were more prominent on Masson’s trichrome staining [Figure 3].
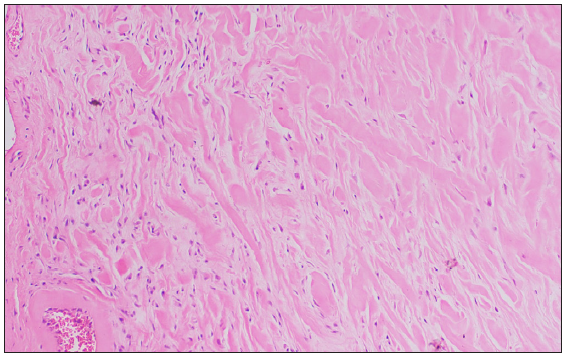
- Histopathology showed haphazardly arranged bundles of homogenously eosinophilic thick collagen (Haematoxylin and Eosin, 100x).
- The thick collagen bundles are more apparent on Masson’s Trichrome (Masson’s trichrome, 200x).
- Presence of mucin between the collagen bundles highlighted on Alcian Blue stain (Alcian Blue-Periodic acid-Schiff, 200x).
A final diagnosis of subungual keloid was made. The patient was advised photoprotection, oral isotretinoin and topical 5% imiquimod for the pre-malignant lesions on the face. Surgical excision has been planned for the larger histologically proven basal cell carcinoma. The patient was offered intralesional steroids for the subungual keloid, but was not keen on monthly injections as the lesion was largely asymptomatic.
Toe keloids are infrequently discussed in literature, classically occurring at the tip or lateral aspect of the digits on the dorsal aspect, following nail surgeries for ingrown toenails and recurrent paronychia.1 This is unlike our case where the keloid was subungual, possibly arising from the nail bed. Although there was no history of previous surgical intervention or a prior nail unit disease in our case, a possibility of unnoticed inadvertent trauma cannot be excluded.
The absence of punctate haemorrhagic spots on gross examination with no tiered parakeratosis or koilocytes on histology ruled out a subungual wart. Histologically, our case lacked dermal fibrosis with multiple ectatic vessels, characteristic of per-ungual fibromas.2 The absence of a central keratinous crater and dyskeratotic eosinophilic cells made subungual keratoacanthoma highly unlikely.3 The tumour was broad-based, not firm and with no tapering, and so did not conform to the finger or hook-like shape of a subungual fibrokeratoma.4 Further, the collagen bundles were not oriented in the vertical axis of the tumour. Instead, the presence of disorganised thick hyalinized collagen (keloidal collagen) bundles in a mucinous ground substance 5 suggested a diagnosis of subungual keloid.
The presence of keloidal tendency in our patient supports our diagnosis. Epigenetic influences on wound healing suggest that oxidative DNA damage in keloidal skin may contribute to its pathogenesis. Fibroblasts with Xeroderma Pigmentosum type C (XPC) mutations exhibit impaired base excision repair leading to increased oxidative DNA damage.6 Thus, keloidal tendency in these patients is likely a true association, rather than a chance occurrence. Further, the subungual hyperkeratosis in other nails in our patient has been reported in other related genodermatoses like Cockayne syndrome, which involves a mutation in similar genes affecting nucleotide excision repair.7 However mutational analyses for a specific complementation subtype of xeroderma pigmentosum could not be done in our case.
In conclusion, subungual keloids are rarely reported and possibly underdiagnosed as they mimic other subungual pathologies. A history of keloidal tendency and the presence of thick hyalinised haphazardly arranged collagen on histology were strong pointers towards this diagnosis. We should also be aware that not all tumours occurring in a patient with xeroderma pigmentosum are necessarily pre-malignant.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)–assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)–assisted technology for assistance in writing or editing of the manuscript, and no images were manipulated using AI.
References
- Toe Keloids treated with core excision, postoperative radiotherapy, and steroid plaster. Plast Reconstr Surg Glob Open. 2020;8:e3085.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Periungual fibroma (Koenen tumors) as isolated sign of tuberous sclerosis complex with tuberous sclerosis complex 1 germline mutation. J Am Acad Dermatol. 2010;62:159-61.
- [CrossRef] [PubMed] [Google Scholar]
- Subungual keratoacanthoma. Indian J Dermatol. 2015;60:623-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Horn on the nail: Acquired ungual fibrokeratoma. J Cutan Aesthet Surg. 2021;14:121-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Histopathological differential diagnosis of keloid and hypertrophic scar. Am J Dermatopathol. 2004;26:379-84.
- [CrossRef] [PubMed] [Google Scholar]
- Xeroderma pigmentosum C (XPC) mutations in primary fibroblasts impair base excision repair pathway and increase oxidative DNA damage. Front Genet. 2020;11:561687.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermatologic findings in 16 patients with Cockayne syndrome and cerebro-oculo-facial-skeletal syndrome. JAMA Dermatol. 2013;149:1414-8.
- [CrossRef] [PubMed] [Google Scholar]





