Translate this page into:
Successful treatment of a case of recalcitrant recurrent aphthous stomatitis using steroid-embedded dissolving microneedles
Corresponding author: Dr. Tan Siyun Lucinda, National Skin Centre, 1 Mandalay Road, Singapore - 308205, Singapore. lucindatan@nsc.com.sg
-
Received: ,
Accepted: ,
How to cite this article: Tan S Lucinda, Ho CY, Tey HL. Successful treatment of a case of recalcitrant recurrent aphthous stomatitis using steroid- embedded dissolving microneedles. Indian J Dermatol Venereol Leprol 2022;88:553-5.
Sir,
Recurrent aphthous stomatitis, a common disease affecting the oral and sometimes genital mucosa, is characterised by recurrent single or multiple, discrete, painful ulcers that usually heal within 7–14 days.1 The pathogenesis is unclear and is likely multifactorial with some evidence to support the idea of immune dysregulation resulting in an exaggerated pro-inflammatory process, or a relatively weak anti- inflammatory response.2 Broad differential diagnoses range from benign conditions to systemic considerations, including connective tissue disorders and inflammatory bowel disease. There is no effective treatment for recurrent aphthous stomatitis, with topical and systemic agents used with variable success. Severe cases can be recalcitrant to various treatment modalities with chronic recurrent attacks of painful oral ulcers causing patient distress. We present a patient with debilitating recurring disease, resistant to multiple treatment modalities, who was eventually successfully treated with steroid-embedded dissolving microneedles.
The patient was a 27-year-old Chinese female, previously healthy with a possible allergy to non-steroidal anti- inflammatory drugs. The onset of disease was in 2016 when she presented with recurrent, painful, buccal ulcers. It would start with a vague itch over the buccal mucosa, followed by swelling. Her condition was aggravated by biting on the swollen buccal mucosa for itch relief resulting in severe recurrent buccal ulcers flaring once every few weeks [Figure 1a]. She had no gut complaints and no family history of inflammatory bowel disease or autoimmune diseases. Investigations done are summarised in Table 1. She was treated for major complex recurrent aphthous stomatitis and responded only partially and temporarily to repeated courses of oral prednisolone (0.5–1 mg/kg/day), together with potent topical steroids and 0.1% tacrolimus. Intralesional triamcinolone (Kenalog®) injections were painful and did not aid in controlling the disease. Colchicine, antihistamines, and gabapentin failed to alleviate flares and prevent recurrences.

- Extensive erosions over bilateral buccal mucosa
| Investigations | Results |
|---|---|
| Buccal biopsy (November 2017) |
Histology: Acanthotic epidermis with cells in the superficial layer pale and vacuolated. Subepidermal blisters not seen. There is a superficial perivascular and periadnexal infiltrate of lymphocytes and plasma cells seen |
| Direct immunofluorescence (November 2017) | Negative |
| Full blood count | Within normal limits |
| Liver function tests | |
| Renal function | |
| Human immunodeficiency virus | Negative |
| Hepatitis B | |
| Hepatitis C | |
| Iron | Within normal limits |
| Folate | |
| Vitamin B12 | |
| C3 | |
| C4 | |
| Antinuclear antibody | Negative |
| dsDNA | |
| Anti proteinase | |
| Anti myeloperoxidase | |
| ELISA for antibodies against | Negative |
| Desmoglein 1 and 3 | |
| Herpes simplex polymerase chain reaction |
Positive • However, treatment and preventive doses of oral acyclovir did not improve or control her disease flares |
Pain necessitated regular doses of tramadol and oxycodone. She was subsequently started on cyclosporine, initially at 4 mg/kg/day, with good response and no further episodes of buccal ulcers.3 Cyclosporine was tapered off after a year of treatment.
Recurrence started in April 2019, after she bit her lower lip accidentally during a meal. The tiny injury rapidly progressed to an extensive ulcer involving most of her lower lip with occasional itching and swelling, resulting in biting which worsened the ulcers, similar to prior experiences. She developed multiple lower lip ulcers, coalescing in some areas, with active raised borders [Figure 1b]. Oral prednisolone (up to 1 mg/kg/day) and acyclovir was restarted but it did not halt ulcer progression. Cyclosporine at 4.4 mg/kg/day was added but the ulcers failed to heal [Figure 1c]. Copious amounts of potent topical steroids/tacrolimus also did not provide much relief.

- Multiple lower lip ulcers, coalescing in some areas, with active raised borders

- Persistent recurring lower lip ulcers coalescing in some areas
Subsequently, cyclosporine was stopped and she was weaned off oral prednisolone before a trial of treatment with steroid- embedded microneedles (Smicna Pte Ltd., Singapore), that are only available for use by our centre’s patients, was commenced.4 Triamcinolone acetonide was embedded into the distal 50% of 600 µm long hyaluronic acid microneedles organised onto patches of one cm diameter [Figure 2]. The microneedles rapidly dissolve upon contact with moist oral mucosa, requiring approximately one minute to release the full 0.2 mg dose of triamcinolone. The patch was self-applied by the patient over the lower lip ulcer region for two minutes daily over 30 days (total dosage of 6 mg). A sensation of pressure with no severe pain was felt as microneedles penetrated the skin superficial to deeper pain-transmitting nerve endings.5 Hence, local anaesthesia was not employed. Adverse effects were limited to mild pain and small shallow erosions from daily microneedle application. Over the subsequent weeks, the ulcers started healing with scarring; with no recurrence was observed over the next one year despite not being on any treatment [Figure 3].
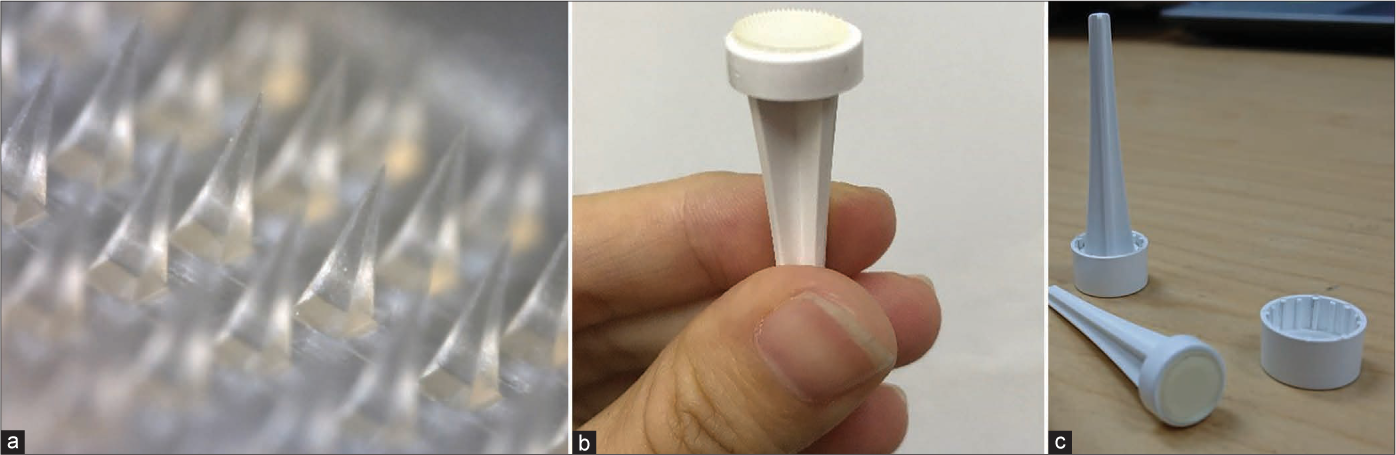
- (a-c) Triamcinolone acetonide is embedded in the distal half of the hyaluronic acid dissolving microneedles and the microneedle patch can be self-applied by patients at a dosage of one patch per day for two minutes over 30 days (equivalent to a conventional single-dose 10 mg/ml injection of intralesional triamcinolone acetonide). The microneedles effectively penetrate the skin superficial to deeper pain-transmitting nerve endings thus obviating the need for local anaesthesia

- Post-treatment image
Recurrent aphthous stomatitis is a clinical diagnosis made after thorough clinical exclude assessment and investigations [Table 1] have been used to exclude underlying systemic causes.6 It can be divided into mild or severe disease known as simple and complex aphthosis, respectively. Simple aphthosis is common, with small and few episodic ulcers healing quickly with minimal pain and disability. Complex aphthosis is uncommon and can be episodic or continuous, with large slow- healing ulcers associated with marked pain and disability. The patient was diagnosed with primary idiopathic major complex recurrent aphthous ulcers, which is a diagnosis of exclusion. The pathogenesis is poorly defined, with predisposing factors including genetic, haematological, vitamin deficiencies, oral trauma, smoking and stress.6 In our patient, an element of oral trauma in the form of self-biting contributed to the worsening of her oral ulcers. While hitherto there were no associated genital ulcers, eye complaints, papulopustular skin lesions or pathergy that fulfilled the diagnostic criteria of Behcet disease, complex aphthosis could be a forme fruste of the disease and our patient will be followed up over time.7 Inflammatory bowel disease was also unlikely given the absence of family history and cardinal gastrointestinal symptoms.
In summary, we present a case of recalcitrant, recurring major complex aphthous ulcers affecting the buccal mucosa and lower lip. Our patient was extremely distressed with the painful ulcers and the complications of weight gain secondary to long-term high-dose oral prednisolone. Her quality of life was severely affected and she could not function well at work. Treatment with triamcinolone-embedded dissolving microneedles enabled disease regression and ulcer resolution. Topical application of microneedles is safe (compared to systemic steroids) and can be applied daily by patients themselves. Such a therapy may be considered as an early treatment option for patients with complex aphthous ulcers.
Declaration of patient consent
The patient’s consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
HL Tey is supported by the Clinician Scientist Awards (NMRC/CSA-INV/0023/2017 and CSAINV20nov-0003) from the National Medical Research Council of Singapore.
Conflicts of interest
There are no conflicts of interest.
References
- Etiopathogenesis of recurrent aphthous stomatitis and the role of immunologic aspects: Literature review. Arch Immunol Ther Exp (Warsz). 2014;62:205-15.
- [CrossRef] [PubMed] [Google Scholar]
- Cyclosporine in the treatment of dermatologic disease: An update. Mayo Clin Proc. 1996;71:1182-91.
- [CrossRef] [PubMed] [Google Scholar]
- Dissolving triamcinolone-embedded microneedles for the treatment of keloids: A single-blinded intra-individual controlled clinical trial. Dermatol Ther (Heidelb). 2019;9:601-11.
- [CrossRef] [PubMed] [Google Scholar]
- Reservoir-based drug delivery systems utilizing microtechnology. Adv Drug Deliv Rev. 2012;64:1590-602.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent aphthous stomatitis: Clinical characteristics and associated systemic disorders. Semin Cutan Med Surg. 1997;16:278-83.
- [CrossRef] [Google Scholar]
- Behçet's disease and complex aphthosis. J Am Acad Dermatol. 1999;40:1-20.
- [CrossRef] [Google Scholar]





