Translate this page into:
Successful treatment of Rosai–Dorfman disease using in situ photoimmunotherapy
2 Institute of Photomedicine, Shanghai Skin Disease Hospital, Tongji University School of Medicine, Shanghai, P. R. China; Biophotonics Research Laboratory, Center for Interdisciplinary Biomedical Education and Research, University of Central Oklahoma, Edmond, OK, USA,
Corresponding Author:
Wei R Chen
Biophotonics Research Laboratory, Center for Interdisciplinary Biomedical Education and Research, University of Central Oklahoma, Edmond, OK, USA
wchen@uco.eduXiuli Wang
Institute of Photomedicine, Shanghai Skin Disease Hospital, Tongji University School of Medicine, Shanghai
P. R. China
wangxiuli20150315@163.com
| How to cite this article: Li M, Shi L, Luo M, Chen J, Wang B, Zhang F, Keyal U, Bhatta AK, Chen WR, Wang X. Successful treatment of Rosai–Dorfman disease using in situ photoimmunotherapy. Indian J Dermatol Venereol Leprol 2017;83:332-336 |
Abstract
Rosai–Dorfman disease is difficult to cure. In situ photoimmunotherapy combines local photothermal therapy with immunoadjuvant. In the present case report, a 39-year-old Chinese man with Rosai–Dorfman disease lesions below the left nostril and left preauricular region was treated with in situ photoimmunotherapy. The patient was treated with daily application of topical imiquimod (5%) and laser irradiations every 2 weeks for 8 weeks. After three cycles of treatment, the lesions improved markedly without adverse effects. Our results showed that in situ photoimmunotherapy can be used as an effective treatment for Rosai–Dorfman disease.Introduction
Rosai–Dorfman disease, commonly termed as sinus histiocytosis with massive lymphadenopathy, is typically characterized by fever, painless cervical lymphadenopathy, polyclonal gammopathy and immunologic dysfunction. Extranodal involvement, especially the skin, has been reported in more than 40% of patients with Rosai–Dorfman disease. Symptomatic disease is usually treated with surgery or systemic prednisone.[1] However, these treatment methods seem to be associated with local recurrence and long-term toxicity.
In situ photoimmunotherapy, a form of combination laser immunotherapy and toll-like receptor agonist stimulation, is a tumor-directed immunotherapy technique, in which an intense local immune response is triggered within and around a preexisting deposit of tumor such as a metastasis. It uses near-infrared laser energy to induce increased temperature in target tissue, kill tumor cells directly and release tumor antigens for the generation of antitumor immunity to treat late-stage metastatic cancers.[2]
In this study, we used in situ photoimmunotherapy for the first time to treat a patient with a large, persistent, Rosai–Dorfman disease refractory to other therapies.
Case Report
A 39-year-old man presented with a 9-month history of slowly growing red and raised lesion below the left nostril and left preauricular region [Figure 1a] and [Figure 1b]. Associated symptoms such as fever, pain and itching were not reported. On clinical examination, erythematous plaques of 3 cm × 3 cm size was noted on the left cheek and 0.5 cm × 1 cm on the left preauricular region. There was no lymphadenopathy. Laboratory tests including complete blood count, urinalysis, liver function tests, thyroid function test and erythrocyte sedimentation rate were all within normal range. Hepatitis B surface antigen was positive, but rapid plasma reagin and a rapid human immunodeficiency virus antibody test were negative. An incisional biopsy from the lesion below the left nostril was taken which showed a nodular infiltration within the dermis consisting of plasma cells, lymphocytes and histiocyte aggregates [Figure - 2]. In addition, emperipolesis found large histiocytes [Figure - 3]. Immunohistochemistry was positive for S-100 [Figure 4a] and CD68 [Figure 4b], but negative for CD1a [Figure 4c]. The positive rate of Ki-67 was 5% [Figure 4d]. Based on these findings, a diagnosis of Rosai–Dorfman disease was made.
 |
| Figure 1a: Erythematous plaque below the left nostril before treatment |
 |
| Figure 1b: Erythematous plaque over the left pre-auricular region before treatment |
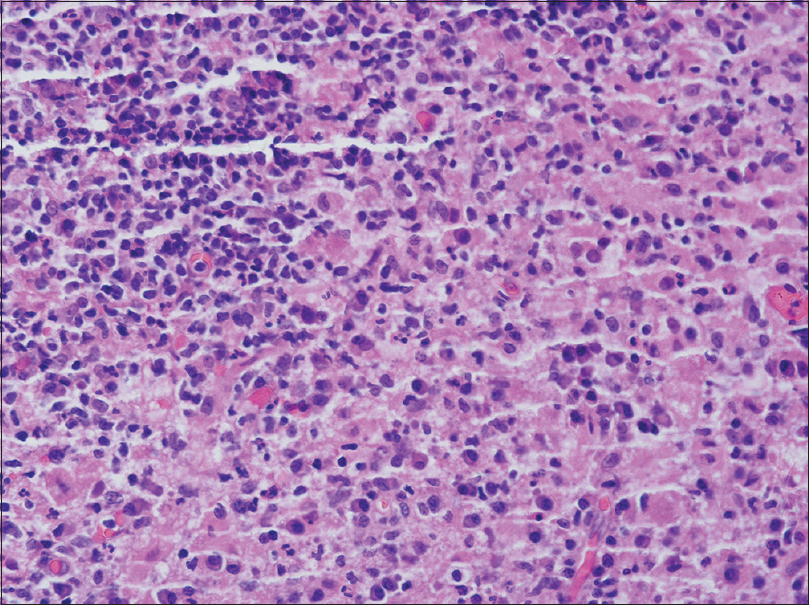 |
| Figure 2: Dermal inflammatory infiltrate consisting of a large number of histiocytes, plasma cells and lymphocytes cells (H and E, ×400) |
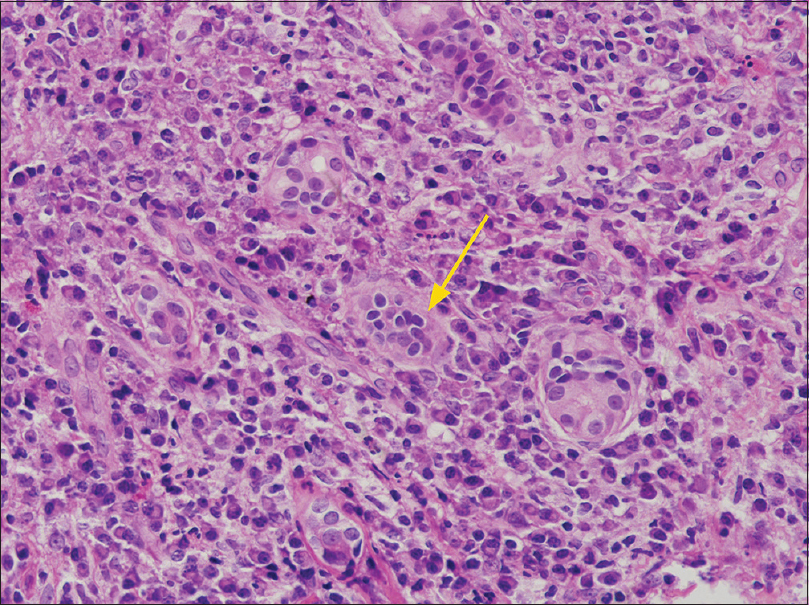 |
| Figure 3: The histiocytes showing emperipolesis (H and E, ×400) |
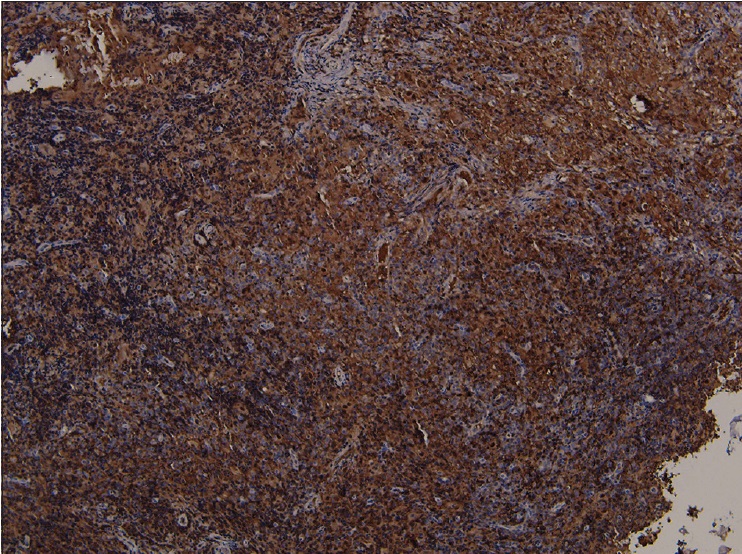 |
| Figure 4a: The histiocytes showing positive for S-100 (×400) |
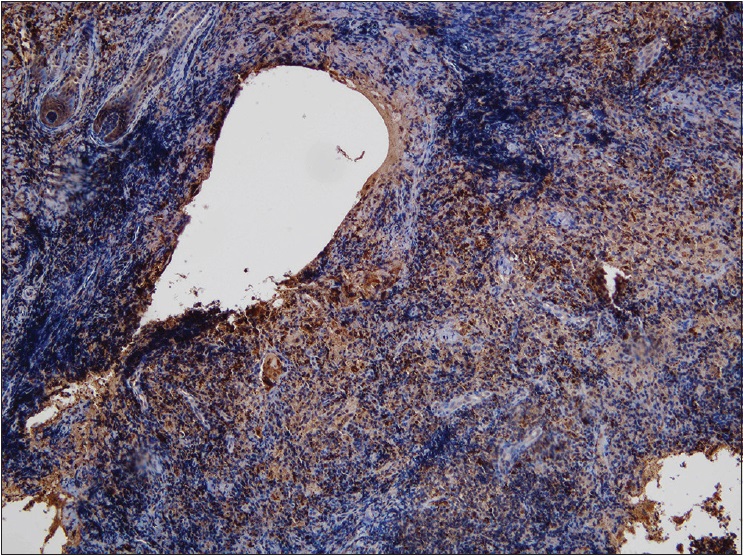 |
| Figure 4b: The histiocytes showing positive for CD68 (×400) |
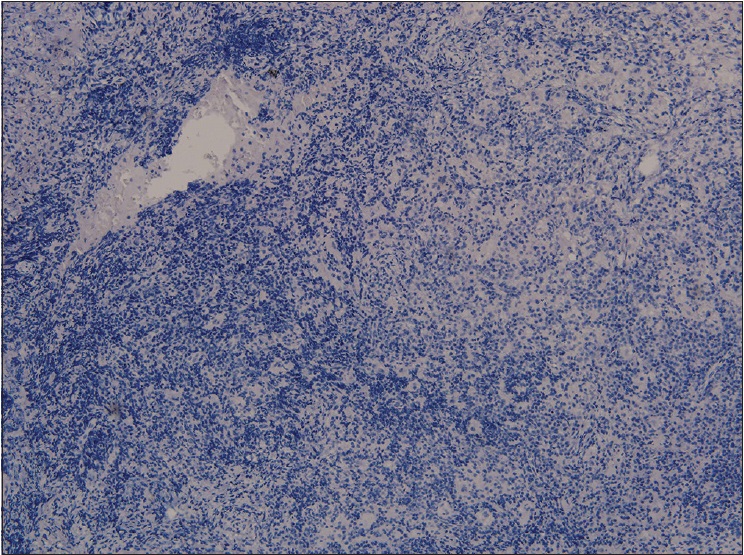 |
| Figure 4c: The histiocytes showing negative for CD1a (×400) |
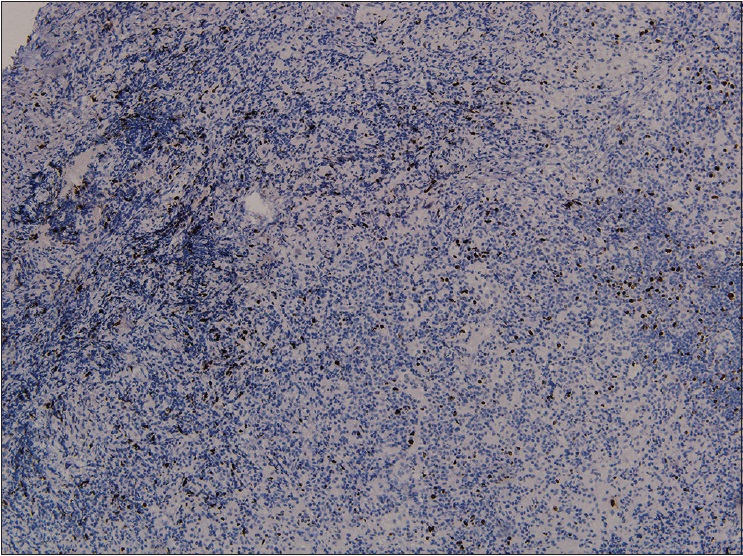 |
| Figure 4d: The histiocytes showing negative for Ki-67 (×400) |
According to the clinical manifestations, the patient was initially treated with oral thalidomide 100 mg bis in die. However, after treatment for 2 months, the lesion was not improved significantly. Instead, the patient developed peripheral neuropathy and gastrointestinal side effects. Therefore, thalidomide treatment was stopped. The patient refused surgery and steroids, due to the known adverse effects. Hence, he was referred for consideration of treatment with in situ photoimmunotherapy. One cycle of in situ photoimmunotherapy included daily application of 5% imiquimod (Sichuan Med-Shine Pharmaceutical Co. Ltd., China) and irradiation of the lesions with 808-nm diode laser (power density = 2.0 W/cm [2], spot size = 2 cm [2], applied for 10 min/treatment spot) at 2-week intervals for 8 weeks [Figure - 5]. The patient received three cycles of treatment at an interval of 4 weeks. During irradiation of the lesion, the temperature of the skin surface was recorded by an infrared thermal imager (FLIR Systems, Inc., USA, T420-NIST). A thermal gradient on the skin surface was generated and the highest temperature reached was 43.4° C [Figure - 6]. After three cycles of in situ photoimmunotherapy, the patient's condition became better. Ultimately, the lesions were flat [Figure 7a] and [Figure 7b]. After completion of the third cycle, the patient was followed up once a month. No adverse effects and recurrence were seen during the follow-up of 6 months.
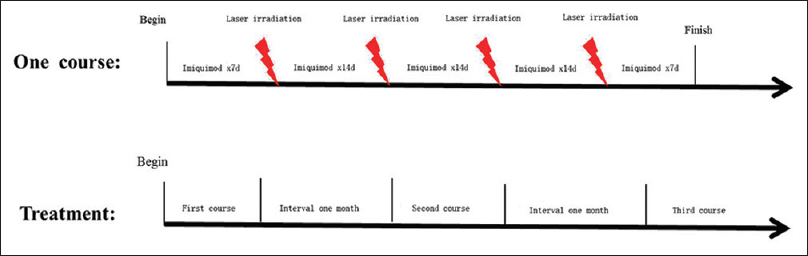 |
| Figure 5: Treatment cycle of photothermal immunotherapy for RDD patient. Three courses of treatment were carried out until the response to the treatment was complete |
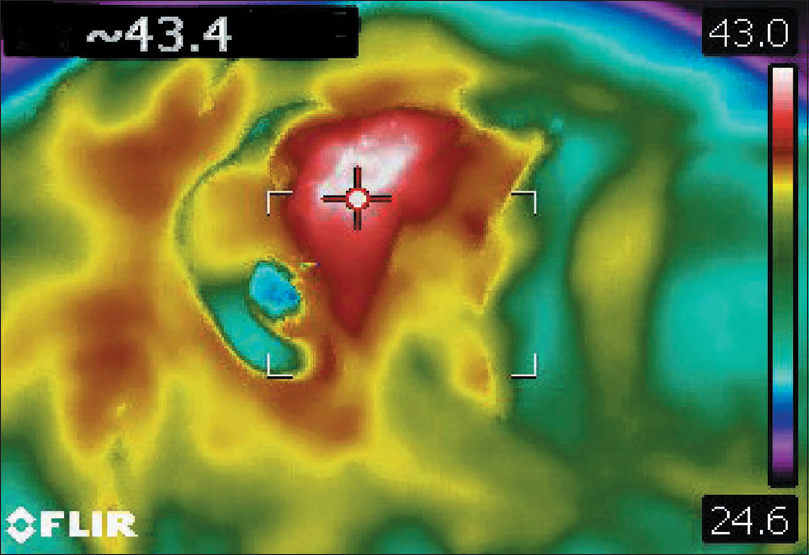 |
| Figure 6: Thermal image took by an infrared thermal imager, showing a thermal gradient with the highest temperature of 43.4℃ on the surface |
 |
| Figure 7a: After the three courses of treatment, the lesions below left nostril were flat and remarkably improved |
 |
| Figure 7b: After the three courses of treatment, the lesions over the left preauricular region were flat and showed remarkable improvement |
Discussion
As Rosai–Dorfman disease is known to have spontaneous regression, aggressive therapeutic measures are not recommended.[2] The present review found that spontaneous resolution (partial or complete) occurred in 16.1% of cases.[3] Available therapeutic measures such as surgery and steroids are associated with adverse effects.[4] Localized Rosai–Dorfman disease can be treated with complete surgical resection, but it has a risk of local recurrence.[5] Furthermore, cosmetic appearance might represent a therapeutic challenge for surgery. Moreover, due to fear and expense of surgery, many patients refuse the treatment. On the other hand, typical initial steroid treatment requires a high dose to achieve successful results. Most of the patients achieve a quick remission with a reduction of inflammatory markers and size of cervical lymph nodes. Unfortunately, steroid tapering was seen to result in reoccurrence of Rosai–Dorfman disease. During every recrudescence, patients experienced long-term toxicity with steroids, such as increased lymph nodes and an increase in inflammatory markers.
In situ photoimmunotherapy is considered a novel treatment for cancer. Wei R. Chen et al. reported that 11 late-stage melanoma patients received in situ photoimmunotherapy in one or multiple 6-week treatment cycles. The probability of 12-month overall survival was 70%. Here, we report for the first time the use of in situ photoimmunotherapy to treat Rosai–Dorfman disease. This report shows palliative responses to in situ photoimmunotherapy for patients who have refractory Rosai–Dorfman disease. As we all know, in situ photoimmunotherapy consists of photothermal therapy and toll-like receptor agonist stimulation has been shown to cure some solid tissues.[6] This is because of the synergistic effects of photothermal therapy and imiquimod. Two mechanisms of action of in situ photoimmunotherapy in Rosai–Dorfman disease can be postulated: One, In situ photoimmunotherapy uses near-infrared laser energy to induce increased temperature in target tissue, kill cells directly and release tumor antigens to generate antitumor immunity.[7] Antigen-presenting cells gather these antigens and migrate to lymph nodes. Dendritic cells present the antigens to T-cells that can induce immune responses against cells.[6] On microscopic examination of Rosai–Dorfman disease, the involved lymph nodes are altered by sinusoidal dilation which contains lymphocytes, histiocytes and plasma cells.[2] Two, Rosai–Dorfman disease is associated with high levels of tumor necrosis factor-a and interlekuin-6;[8] imiquimod [9] also induced IL-1 alpha, IL-1 receptor antagonist, IL-10, granulocyte-macrophage colony-stimulating factor (GM-CSF), granulocyte CSF (G-CSF), and macrophage inflammatory protein-1 alpha to enhance therapeutic effect.
We report the possible mechanisms of action of in situ photoimmunotherapy for Rosai–Dorfman disease and also report that in situ photoimmunotherapy has no obvious side effects. In our case, the patient had a 9-month history of Rosai–Dorfman disease and there was no improvement in the skin lesions through a variety of methods. Our patient with Rosai–Dorfman disease achieved improvement gradually as the in situ photoimmunotherapy cycles increased, so we believe that the improvement is due to three cycles of in situ photoimmunotherapy treatment. In situ photoimmunotherapy may be an appropriate therapy in refractory disease, owing to facial and other special parts to protect the appearance. The present study is the first reported case of in situ photoimmunotherapy inducing remission in Rosai–Dorfman disease. Because this case is only a case report, we will expand the case series and perform randomized controlled trials to further verify the efficacy of in situ photoimmunotherapy in the treatment of Rosai–Dorfman disease.
Conclusion
ISPI can be used as an effective treatment for Rosai–Dorfman disease.
Financial support and sponsorship
This study was supported financially by the National Natural Science Foundation of China (81272990, 81472538, 81472796).
Conflicts of interest
There are no conflicts of interest.
Ethics statement
The current study was approved by Shanghai Skin Disease Hospital.
| 1. | Toguri D, Louie AV, Rizkalla K, Franklin J, Rodrigues G, Venkatesan V. Radiotherapy for steroid-resistant laryngeal Rosai-Dorfman disease. Curr Oncol 2011;18:e158-62. [Google Scholar] |
| 2. | Madhunapantula SV, Gowda R, Inamdar GS, Robertson GP. In situ photoimmunotherapy: A new hope for cutaneous melanoma patients. Cancer Biol Ther 2010;10:1088-90. [Google Scholar] |
| 3. | Al-Khateeb TH. Cutaneous Rosai-Dorfman disease of the face: A comprehensive literature review and case report. J Oral Maxillofac Surg 2016;74:528-40. [Google Scholar] |
| 4. | Dalia S, Sagatys E, Sokol L, Kubal T. Rosai-Dorfman disease: Tumor biology, clinical features, pathology, and treatment. Cancer Control 2014;21:322-7. [Google Scholar] |
| 5. | Adeleye AO, Amir G, Fraifeld S, Shoshan Y, Umansky F, Spektor S. Diagnosis and management of Rosai-Dorfman disease involving the central nervous system. Neurol Res 2010;32:572-8. [Google Scholar] |
| 6. | Chen WR, Jeong SW, Lucroy MD, Wolf RF, Howard EW, Liu H, et al. Induced antitumor immunity against DMBA-4 metastatic mammary tumors in rats using laser immunotherapy. Int J Cancer 2003;107:1053-7. [Google Scholar] |
| 7. | den Brok MH, Sutmuller RP, van der Voort R, Bennink EJ, Figdor CG, Ruers TJ, et al. In situ tumor ablation creates an antigen source for the generation of antitumor immunity. Cancer Res 2004;64:4024-9. [Google Scholar] |
| 8. | Aouba A, Terrier B, Vasiliu V, Candon S, Brousse N, Varet B, et al. Dramatic clinical efficacy of cladribine in Rosai-Dorfman disease and evolution of the cytokine profile: Towards a new therapeutic approach. Haematologica 2006;91 12 Suppl:ECR52. [Google Scholar] |
| 9. | Testerman TL, Gerster JF, Imbertson LM, Reiter MJ, Miller RL, Gibson SJ, et al. Cytokine induction by the immunomodulators imiquimod and S-27609. J Leukoc Biol 1995;58:365-72. [Google Scholar] |
Fulltext Views
3,906
PDF downloads
1,621





