Translate this page into:
Successful treatment outcome with itraconazole and potassium iodide in disseminated sporotrichosis
Correspondence Address:
Binod K Khaitan
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi
India
| How to cite this article: Khaitan BK, Gupta V, Asati DP, Seshadri D, Ramam M. Successful treatment outcome with itraconazole and potassium iodide in disseminated sporotrichosis. Indian J Dermatol Venereol Leprol 2018;84:101-104 |
Sir,
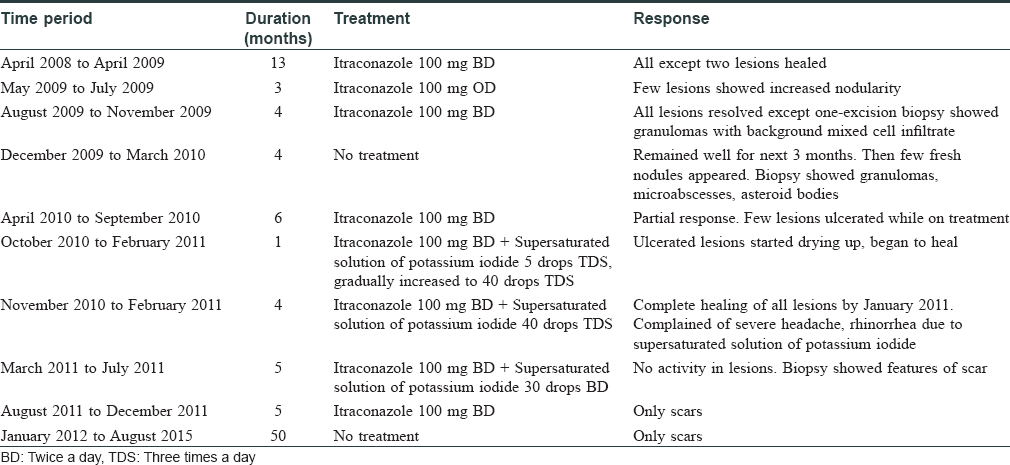
A 57-year-old man, from Rajasthan, India presented with a 6 months history of painful erythematous nodules and plaques, some of which were ulcerated and crusted over the trunk, upper, and lower limbs. Few lesions on the back were linear in shape [Figure - 1] and [Figure - 2]. He also complained of hoarseness of voice for 2 months. There was no preceding history of trauma, thorn pricks, or animal bites. Medical history was significant for well-controlled hypertension (on ramipril and amlodipine) and diabetes mellitus (on glimepride and metformin). Routine hematological investigations were unremarkable, whereas mantoux test and enzyme-linked immunosorbent assay (ELISA) for human immunodeficiency virus (HIV)-1 and 2 were negative. Skin biopsies from intact and ulcerated plaques showed necrotizing epithelioid cell granulomas in the dermis with neutrophilic microabscesses [Figure - 3] and [Figure - 4]. Special stains and culture for fungi and mycobacteria were negative. Laryngoscopy revealed a supraglottic growth, however, the patient refused for biopsy of the lesion. Contrast-enhanced computerized tomography of the chest and abdomen was unremarkable. With a provisional diagnosis of disseminated cutaneous sporotrichosis, the patient was treated with oral itraconazole 200 mg/day. Over the next 12 months, all the lesions completely healed with scarring. The patient also noticed significant improvement in his voice, and the dose of itraconazole was tapered to 100 mg/day. Within the next 3 months, few of the earlier healed lesions began to show increased nodularity. The dose of itraconazole was hiked to 200 mg/day, which led to near complete resolution of all lesions within 4 months except for one persistent lesion which was excised and showed similar histological features as the previous lesions. Subsequently, itraconazole was stopped and the patient remained well for the next 3 months. However, 1 month later, few fresh nodules appeared on the abdomen and forearms, which on histological examination showed dense mixed cell infiltrates and asteroid bodies [Figure - 5] on periodic acid Schiff (PAS) staining characteristic of sporotrichosis [Figure - 6]; however, the fungal culture was negative. Itraconazole was restarted at a dose of 200 mg/day. However, this time, there was only partial flattening of the lesions, therefore, supersaturated solution of potassium iodide was added at a starting dose of 5 drops thrice daily, which was gradually increased to 40 drops thrice daily over a month. All lesions healed completely with 5 months of combination therapy, which was continued for a further 4 months with a lower dose of supersaturated solution of potassium iodide (30 drops thrice daily) as the patient complained of severe headache and rhinorrhea. After 9 months of combination therapy, biopsy from a healed lesion showed features of a scar. Subsequently, supersaturated solution of potassium iodide was stopped while itraconazole 200 mg daily was continued for 5 more months and stopped. It is now 4 years since all treatment was stopped, and presently, the only cutaneous abnormalities are scars at the sites of healed lesions, without any evidence of reactivation of older lesions [Figure - 7] and [Figure - 8]. The treatment course and response in our patient is summarized in [Table - 1].
 |
| Figure 1: Multiple erythematous plaques on the back. Linear configuration of some of the plaques can be noted |
 |
| Figure 2: Plaque with overlying ulceration on the left arm |
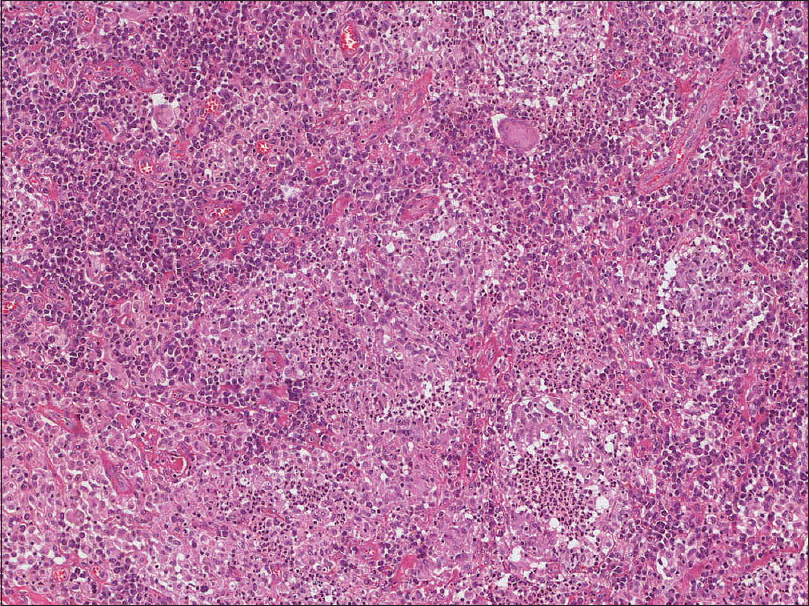 |
| Figure 3: Biopsy from one of the plaques showing dense dermal infiltrate composed of lymphocytes, histiocytes, plasma cells with collection of epitheloid cells and an occasional giant cell admixed with polymorphs (hematoxylin and eosin, ×100) |
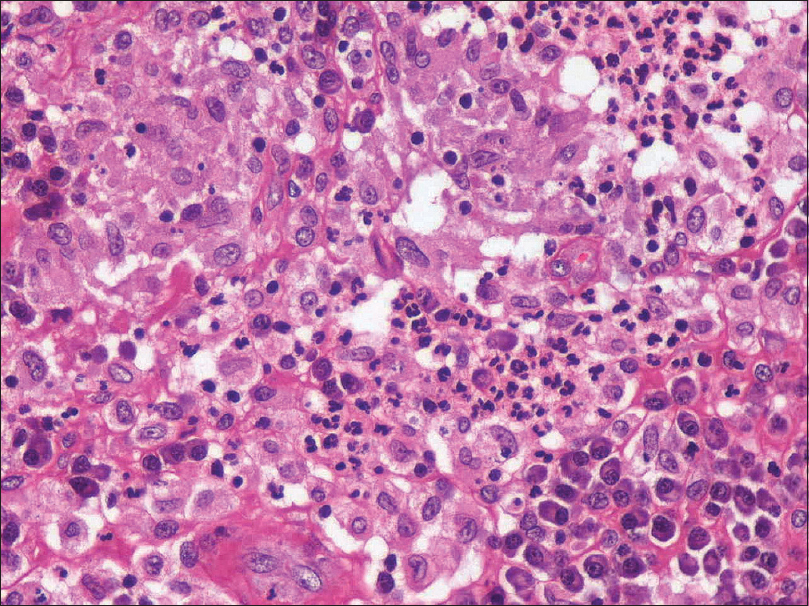 |
| Figure 4: Higher magnification showing collection of neutrophils (neutrophilic microabscess) along with epithelioid cells and plasma cells (hematoxylin and eosin, ×400) |
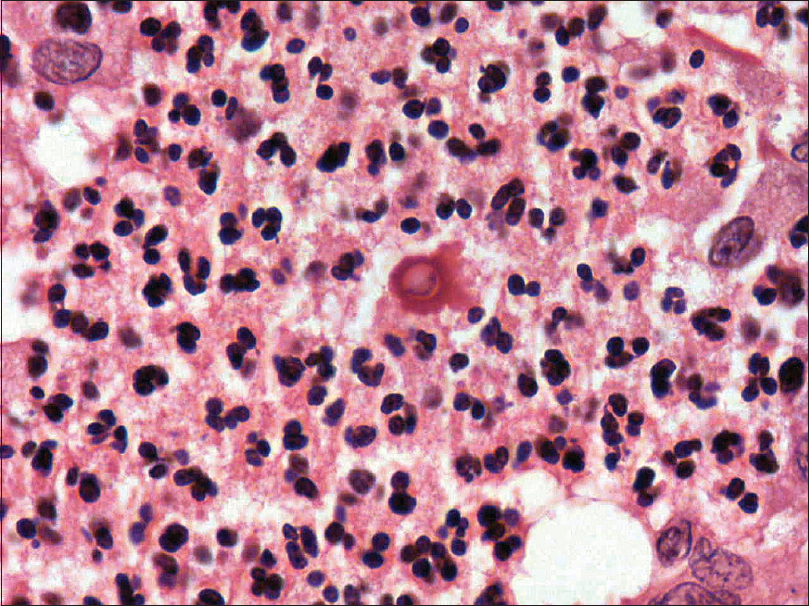 |
| Figure 5: Central yeast with surrounding radiating eosinophilic material (asteroid body) seen in the subsequent biopsy (hematoxylin and eosin, ×400) |
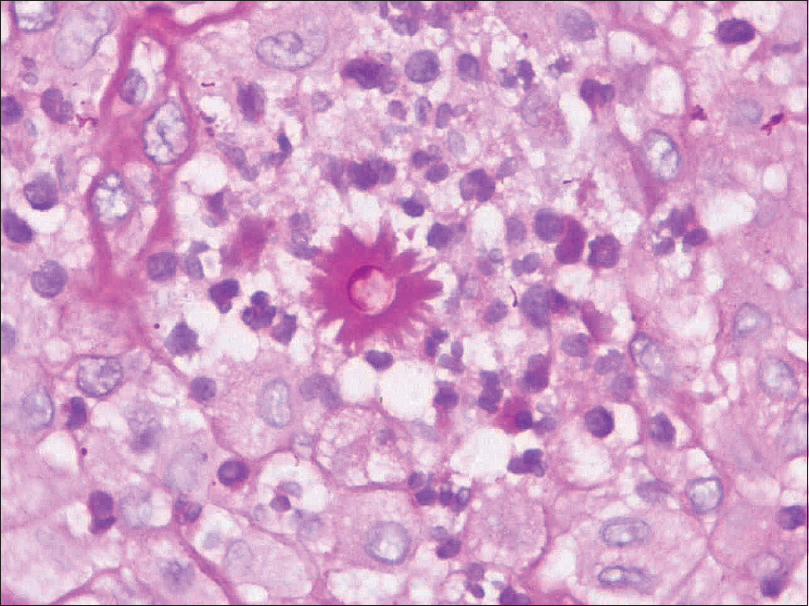 |
| Figure 6: Central yeast with surrounding radiating eosinophilic material (asteroid body) seen in the subsequent biopsy (periodic-acid Schiff, ×400) |
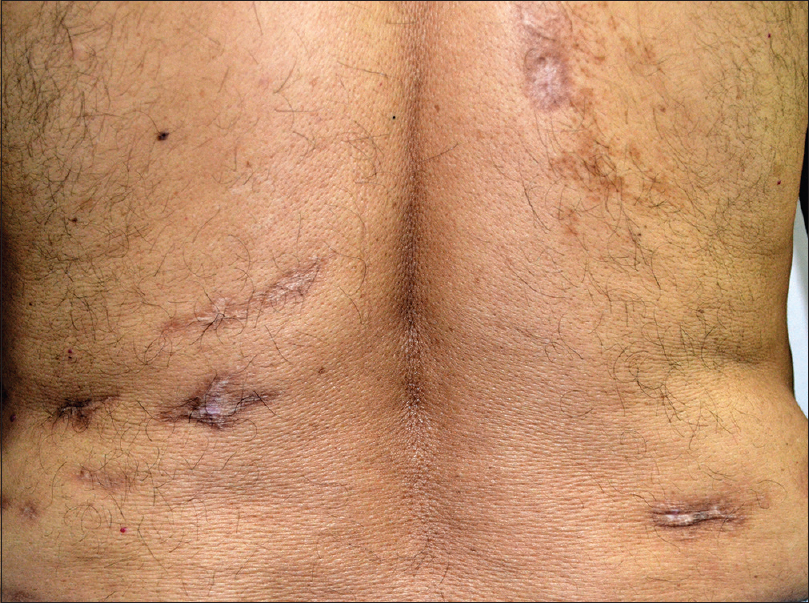 |
| Figure 7: Post-treatment photograph showing healed scars on the back |
 |
| Figure 8: Post-treatment photograph showing healed scars on the left arm |
Sporotrichosis has been reported from many parts of the world, mainly from tropical and temperate areas.[1] In India, majority of the cases have been described from the sub-Himalayan belt.[2],[3] Disseminated cutaneous sporotrichosis is usually seen in immunocompromised patients, however, it has been reported in immunocompetent patients as well.[4],[5],[6] Diabetes mellitus, though well-controlled, could have predisposed our patient to such a widespread infection. Greater virulence of the infecting strain could be another explanation for the disseminated infection in our patient.[7] Apart from disseminated cutaneous disease, our patient might have had laryngeal involvement, supported by the rapid improvement in hoarseness of voice with antifungal therapy. The clinical picture, as seen in our case, has a broad differential diagnosis including cutaneous tuberculosis, atypical mycobacterial infection, leishmaniasis, and other deep mycoses all of which may also share the histopathologic finding of a mixed cell infiltrate/granuloma. Though the gold standard for diagnosis of sporotrichosis is the isolation of fungus in Sabouraud's dextrose agar, a culture may not always be positive. Molecular tests such as polymerase chain reaction can also be used to establish the diagnosis, but are not available widely. In such a scenario, a therapeutic trial may help in settling the diagnosis. Though there was an initial good response to itraconazole, lesions relapsed soon after tapering or stopping treatment. It was only on repeated biopsies that the asteroid bodies were visualized, thus confirming the diagnosis. The recommended treatment for disseminated/systemic sporotrichosis, is Amphotericin B followed by oral itraconazole 400 mg/day (for a total of 12 months).[8] Successful treatment of disseminated sporotrichosis with oral itraconazole[9] as well as supersaturated solution of potassium iodide[10] has also been reported previously. As our patient refused amphotericin B citing the high cost of therapy and the need for inpatient treatment, we decided to continue oral itraconazole in view of the initial improvement with this agent. We could not increase the itraconazole dose considering the financial constraints of the patient, and added supersaturated solution of potassium iodide when the clinical response was less than satisfactory. Our patient benefited from the combination of itraconazole and potassium iodide.
To conclude, we wish to emphasize the utility of a therapeutic trial in sporotrichosis and the need for multiple biopsies in arriving at the correct diagnosis, where a definitive diagnosis maybe difficult at the outset. Prolonged combination treatment with itraconazole and potassium iodide may be an alternative treatment strategy in patients with disseminated sporotrichosis who cannot be treated with amphotericin B for any reason.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for her images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published and due efforts will be made to conceal his entity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Barros MB, de Almeida Paes R, Schubach AO. Sporothrix schenckii and Sporotrichosis. Clin Microbiol Rev 2011;24:633-54.
[Google Scholar]
|
| 2. |
Mahajan VK, Sharma NL, Sharma RC, Gupta ML, Garg G, Kanga AK. Cutaneous sporotrichosis in Himachal Pradesh, India. Mycoses 2005;48:25-31.
[Google Scholar]
|
| 3. |
Mehta KI, Sharma NL, Kanga AK, Mahajan VK, Ranjan N. Isolation of Sporothrix schenckii from the environmental sources of cutaneous sporotrichosis patients in Himachal Pradesh, India: Results of a pilot study. Mycoses 2007;50:496-501.
[Google Scholar]
|
| 4. |
Gottlieb GS, Lesser CF, Holmes KK, Wald A. Disseminated sporotrichosis associated with treatment with immunosuppressants and tumor necrosis factor-alpha antagonists. Clin Infect Dis 2003;37:838-40.
[Google Scholar]
|
| 5. |
Song Y, Li SS, Zhong SX, Liu YY, Yao L, Huo SS. Report of 457 sporotrichosis cases from Jilin province, Northeast China, a serious endemic region. J Eur Acad Dermatol Venereol 2013;27:313-8.
[Google Scholar]
|
| 6. |
Tang MM, Tang JJ, Gill P, Chang CC, Baba R. Cutaneous sporotrichosis: A six-year review of 19 cases in a tertiary referral center in Malaysia. Int J Dermatol 2012;51:702-8.
[Google Scholar]
|
| 7. |
Kong X, Xiao T, Lin J, Wang Y, Chen HD. Relationships among genotypes, virulence and clinical forms of Sporothrix schenckii infection. Clin Microbiol Infect 2006;12:1077-81.
[Google Scholar]
|
| 8. |
Kauffman CA, Bustamante B, Chapman SW, Pappas PG; Infectious Diseases Society of America. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis 2007;45:1255-65.
[Google Scholar]
|
| 9. |
Yang DJ, Krishnan RS, Guillen DR, Schmiege LM 3rd, Leis PF, Hsu S. Disseminated sporotrichosis mimicking sarcoidosis. Int J Dermatol 2006;45:450-3.
[Google Scholar]
|
| 10. |
Fujii H, Tanioka M, Yonezawa M, Arakawa A, Matsumura Y, Kore-eda S, et al. Acase of atypical sporotrichosis with multifocal cutaneous ulcers. Clin Exp Dermatol 2008;33:135-8.
[Google Scholar]
|
Fulltext Views
5,185
PDF downloads
3,274





