Translate this page into:
Surgical therapy of vitiligo: Current status
Correspondence Address:
Satish S Savant
Dept. of Skin and STD, Nanavati Hospital, Vile Parle (W), Mumbai-400 056
India
| How to cite this article: Savant SS. Surgical therapy of vitiligo: Current status. Indian J Dermatol Venereol Leprol 2005;71:307-310 |
Vitiligo is an acquired condition that presents as sharply demarcated white macules.[1],[2] It affects 1%-2% people of all races regardless of sex and age. Although the disease does not have any systemic complications, it is of great cosmetic concern, particularly in darker skinned individuals, as in Indians, where it creates psychological problems due to the stigma attached to it. In vitiligo, there is a partial or total destruction of melanocytes, initially only of the epidermis, and later even of the hair follicle, which acts as a reservoir for providing melanocytes during repigmentation.[3] Hence, in patients with vitiligo, the existing melanocytes need to be activated. While medical therapies are the primary treatment, there are some patients refractory to medical treatment. In such patients, surgical therapies can be used either alone or in conjunction with medical therapy to achieve repigmentation provided the disease is stable. Stability has been defined by different authors as a period varying from 6 months to 2 years during which the existing lesions should not have enlarged, no new lesions should have developed, and there should be no koebnerization. [4],[5],[6],[7] It is best to confirm the stability of the disease by doing trial test grafting in a small vitiliginous area 1½-2 months before undertaking surgery of the entire lesion.[8],[9]
Various surgical procedures have been designed with the following aims:[10]
1) Introduction of artificial pigments into the lesions for permanent camouflage, e.g. tattooing.
2) Removal of the depigmented areas forever, e.g. excision with primary closure, and covering with thin Thiersch′s graft.
3) Repopulation of the depleted melanocytes by various grafts, e.g. ultra-thin grafts, suction blister and miniature punch grafts, non-cultured epidermal cell suspension or transplantation, and epidermal and melanocyte cultures.
4) Therapeutically wounding the lesion to stimulate the melanocytes from the periphery and the black hair follicles to proliferate, migrate and re-pigment the lesion, e.g. therapeutic dermabrasion, laser ablation, cryosurgery (liquid nitrogen spraying), needling, and local application of phenol or trichloroacetic acid.
Since 1964, various surgical techniques and modifications have been used to treat recalcitrant but stable vitiligo with permanent and almost complete repigmentation.[11] Behl was the first to report the use of thin Thiersch′s skin graft to treat vitiligo.[12] In 1971, Falabella described the suction blister technique for repigmentation through melanocyte transplantation.[13] Falabella also introduced the autologous miniature punch graft technique in 1978.[14] Suji and Hamada in 1983 used therapeutic spot dermabrasion for stable vitiligo.[15] The technique of spot therapeutic wounding was further extended by using needling, phenol, trichloroacetic acid, cryosurgery, carbon dioxide laser, etc. [16],[17],[18] Halder et al reported the use of ferrous oxide pigment for tattooing for the treatment of vitiligo in a large series in 1989.[19] Cultured autologous melanocytes were first introduced by Lerner et al in 1987.[20] Gaunthier and Surleve-Bazeille used a non-cultured autologous melanocyte rich epidermal cell suspension in 1989 and this technique was further refined by Olsson and Juhlin.[21]-[22] In 1993, Kahn et al successfully re-pigmented vitiligo lesions by a melanocytic transplant using ultra-thin epidermal sheets.[23] Since then, various techniques of vitiligo surgery have been improvised and modified to achieve better results. [24],[25],[26],[27],[28],[29],[30],[31],[32],[33],[34],[35],
The result of all surgical methods should be uniform pigmentation throughout the lesion with the surface texture and color matching that of the surrounding skin as much as possible to be cosmetically acceptable to the patient. The different methods have their own advantages and disadvantages. The choice of method in a particular patient depends on the site, size, shape, etc. of the lesions as well as the experience of the surgeon and the available technical support.
The following methods have been found to be useful at certain locations. For vitiligo areas with at least 25%-50% of black hair, any of the therapeutic wounding methods (phenolization is the simplest and cost effective) will accelerate the process of repigmentation. For the tips of the fingers and toes, and palms and soles, miniature punch grafting (MPG) is the best method. For the angles of the mouth and genitalia, tattooing is the best choice because the chance of graft rejection at these sites is high. The suction blister technique (SBT) works very well over the lips and eyelids, especially after the introduction of surgical glue and the multiple syringe technique.
Large patches can be covered either with thin Thiersch′s split thickness skin grafts (TT-STSG), ultra-thin skin grafts (UTSG), non-cultured epidermal cell suspension or cellular cultures. The pattern of the lesion also dictates the method to be used. Small gaps or partially healed lesions can be needled, phenolized or tattooed. For geographical amoeboid lesions, MPG is suitable. Round or oval lesions are best treated with TT-STSG, UTSG, suspensions or culture.
While the availability of technical support (e.g. tissue culture laboratory equipment, technical help, and hospital set-up) is also a deciding factor in the selection of the technique, the most important criterion is the expertise of the dermatosurgeon in various techniques. One must select the method with which one is most conversant and comfortable. The technique should be individualized and tailored with respect to each patient. Some patients may require a combination of two techniques. [36],[37],[38],
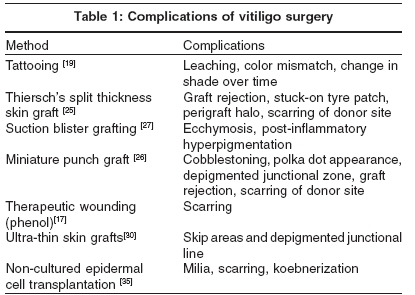
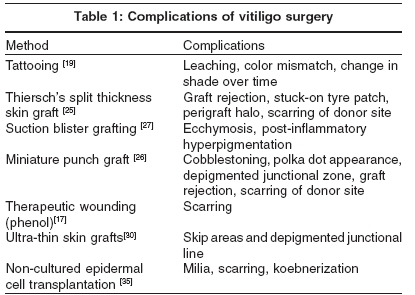
Vitiligo surgeries are not without complications [Table - 1]. Most authors have claimed good-to-excellent results (60% to 95% repigmentation) with the surgical method that they had adopted depending upon the type, size, site and stability of vitiligo lesions, age and color complexion of patient, and whether PUVA/PUVASOL was used post-operatively. [6],[7],[8],[9],[10],[11],[12],[13],[14],[15],[16],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27],[28],[29],[30],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40],[41], Overall, better results are reported in focal and segmental vitiligo (75%-95%) than in generalized vitiligo. Younger (20-30 years) and darker complexioned patients have better results. Comparatively, acral areas, malleoli, knees, and elbows are less responsive to surgery. Smaller patches respond better. Addition of PUVA/PUVASOL therapy enhances repigmentation and increases the success rate (90%-95%).
On an average, TT-STSG, UTSG, and SBT yield 1:1 coverage of the affected area. [6],[7],[8],[9],[10],[11],[12],[13],[14],[15],[16],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27],[28],[29],[30],[31],[32],[33],[34],[35],[36],In MPG the perigraft spread of pigment is 2-4 folds.[3] However, the limitation of MPG is that cosmetic acceptability is not very good. Non-cultured epidermal cell suspension gives coverage of 3-4 times the biopsy specimen size but requires tedious perioperative steps.[42] The best expansion obtained is with pure cultures (mixed or pure melanocytes). But, facilities for culture are expensive, available at few centers, and need technical support. This technique has now been simplified by the commercial availability of an autologous harvesting device (Recell), which reduces the tedious perioperative steps. To cover wider areas, a similar system, called single cell suspension spray (cell spray), is available. [42] It contains expanded autologous cultured epidermal cells. Both these systems are expensive and are not available in India.
In India, miniature punch grafting and SBT will remain the mainstay of vitiligo surgical treatment by virtue of their simplicity, cost effectiveness and efficacy. In future, the method that gives a wider coverage with a smaller amount of donor tissue will succeed if it is economical and easily available.
| 1. |
Kovacs SO. Vitiligo (review). J Am Acad Dermatol 1998;38:647-66.
[Google Scholar]
|
| 2. |
Grimes PE. Vitiligo: an overview of therapeutic approaches (review). Dermatol Clin 1993;11:3254-358.
[Google Scholar]
|
| 3. |
Falabella R. Surgical treatment of vitiligo; why, when and how. J Eur Acad Dermatol Venereol 2003;17:518-20.
[Google Scholar]
|
| 4. |
Savant SS. Autologous miniature punch skin grafting in stable vitiligo. Indian J Dermatol Venereol Leprol 1992;58:310-4.
[Google Scholar]
|
| 5. |
Boersma BR, Westerhof W, Bos JD. Repigmentation in vitiligo vulgaris by autologous minigrafting: results in nineteen patients. J Am Acad Dermatol 1995;33:990-5.
[Google Scholar]
|
| 6. |
Njoo MD, Westerhof W, Bos JD, Bossuyt MM. A systematic review of autologous transplantation methods in vitiligo. Arch Dermatol 1998;134:1543-5.
[Google Scholar]
|
| 7. |
Guerra L, Capurro S, Melchi F. Treatment of "stable" vitiligo by timed surgery and transplantation of cultured epidermal autografts. Arch Dermatol 2000;136:1380-9.
[Google Scholar]
|
| 8. |
Falabella R, Arrunategui A, Barona MI, Alzate A. The minigrafting test for vitiligo: detection of stable lesions for melanocytes transplantation. J Am Acad Dermatol 1995;32:228-32.
[Google Scholar]
|
| 9. |
Westerhof W, Boersma BR. The minigrafting test for vitiligo: detection of stable lesions for melanocytes transplantation. J Am Acad Dermatol 1995;33:1061-2.
[Google Scholar]
|
| 10. |
Savant SS. Introduction to vitiligo surgery. In: Savant SS, editor. Textbook of dermatosurgery and cosmetology. 2nd edn. Mumbai: ASCAD; 2005. p. 336.
[Google Scholar]
|
| 11. |
Westerhof W, Lontz W, Vanscheidt W, Braathen L. Vitiligo news in surgical treatment. J Eur Acad Dermatol Venereol 2001;15:510-1.
[Google Scholar]
|
| 12. |
Behl PN. Treatment of vitiligo with homologous thin Thiersch's skin grafts. Curr Med Pract 1964;8:218-21.
[Google Scholar]
|
| 13. |
Falabella R. Epidermal grafting: an original technique and its application in achromic and granulating areas. Arch Dermatol 1971;104:592-600.
[Google Scholar]
|
| 14. |
Falabella R. Pigmentation of leukoderma by minigrafts of normal pigmented autologous skin. J Dermatol Surg Oncol 1978;4:916-9.
[Google Scholar]
|
| 15. |
Tsuji T, Hamada T. Topically administered fluorouracil in vitiligo. Arch Dermatol 1983;119:722-7.
[Google Scholar]
|
| 16. |
Savant SS. Therapeutic spot and regional dermabrasion in stable vitiligo. Indian J Dermatol Venereol Leprol 1996;62:139-45.
[Google Scholar]
|
| 17. |
Savant SS. Therapeutic wounding. In: Savant SS, editor. Textbook of dermatosurgery and cosmetology. 2nd edn. Mumbai: ASCAD; 2005. p. 370-7.
[Google Scholar]
|
| 18. |
Savant SS, Shenoy S. Chemical peeling with phenol for the treatment of stable vitiligo and alopecia areata. Indian J Dermatol Venereol Leprol 1999;65:93-8.
[Google Scholar]
|
| 19. |
Halder RM, Pham HN, Breadon JY. Micropigmentation for the treatment of vitiligo. J Dermatol Surg Oncol 1989;15:1092-8.
[Google Scholar]
|
| 20. |
Lerner AB, Halaben R, Klaus SN, Moellmann GE. Transplantation of human melanocytes. J Invest Dermatol 1987;89:219-24.
[Google Scholar]
|
| 21. |
Gauthier Y, Surleve-Brazeille JE. Autologous grafting with noncultured melanocytes; a simplified method for treatment of depigmented lesions. J Am Acad Dermatol 1992;26:191-4.
[Google Scholar]
|
| 22. |
Olsson MJ, Juhlin L. Melanocyte transplantation in vitiligo. Lancet 1992;340:981-5.
[Google Scholar]
|
| 23. |
Kahn AM, Cohen MJ, Kaplan L. Vitiligo: treatment by dermabrasion and epithelial sheet grafting - a preliminary report. J Am Acad Dermatol 1993;28:773-4.
[Google Scholar]
|
| 24. |
Gharpuray MB, Mutalik S. Manual punch for tattooing. J Dermatol Surg Oncol 1994;20:548-50.
[Google Scholar]
|
| 25. |
Behl PN, Azad O, Kah R, Shrivastava G. Autologous thin Thiersch's grafts in vitiligo: Experience of 8000 cases, 50,000 grafts (1959-1998) with modified technique in 198 cases in the year 1997-1998. Indian J Dermatol Venereol Leprol 1999;65:117-21.
[Google Scholar]
|
| 26. |
Savant SS. Autologous miniature punch grafting in stable vitiligo. Indian J Dermatol Venereol Leprol 1992;58:310-4.
[Google Scholar]
|
| 27. |
Gupta S, Shroff S, Gupta S. Modified technique of suction blistering for epidermal grafting in vitiligo. Indian J Dermatol 1999;38:306-9.
[Google Scholar]
|
| 28. |
Lontz W, Olsson MJ, Medllmann G, Lerner AB. Pigment cell transplantation for treatment of vitiligo: a progress report. J Am Acad Dermatol 1994;30:591-7.
[Google Scholar]
|
| 29. |
Olsson MJ, Juhlin L. Leucoderma treated by transplantation of a basal cell layer enriched suspension. Br J Dermatol 1998;138:644-8.
[Google Scholar]
|
| 30. |
Kahn AM, Cohen MJ. Repigmentation in vitiligo patients. Melanocyte transfer via ultra thin grafts. J Dermatol Surg 1998;24:365-7.
[Google Scholar]
|
| 31. |
Kahn AM, Ostad SO, Moy DC. Grafting following short pulse CO2 laser de-epithelialization. J Dermatol Surg 1999;25:669-70.
[Google Scholar]
|
| 32. |
Chen YF, Chang JS, Yang PY. Transplant of cultured autologous pure melanocytes after laser abrasion for treatment of segmental vitiligo. J Dermatol Surg 2000;27:434-9.
[Google Scholar]
|
| 33. |
Chen YF, Yang PY, Hu DN. Treatment of vitiligo by transplantation of cultured pure melanocyte suspension. Analysis of 120 cases. J Am Acad Dermatol 2004;51:68-74.
[Google Scholar]
|
| 34. |
Mulekar SV. Melanocyte-keratinocyte cell transplantation for stable vitiligo. Int J Dermatol 2003;42:132-6.
[Google Scholar]
|
| 35. |
Mulekar SV. Long term follow-up study of segmental and focal vitiligo treated by autologous non cultured melanocytes-keratinocyte cell transplantation. Arch Dermatol 2004;140:1211-5.
[Google Scholar]
|
| 36. |
Savant SS. Vitiligo surgery: Which? Where? Why? In: Savant SS, editor. Textbook of dermatosurgery and cosmetology, 2nd edn. Mumbai: ASCAD; 2005. p. 394-7.
[Google Scholar]
|
| 37. |
Mutalik S, Ginzberg A. Surgical management of stable vitiligo: A review with personal experience. J Dermatol Surg 2000;26:248-54.
[Google Scholar]
|
| 38. |
Van Geel N, Ongenae K, Naeyaert JM. Surgical techniques for vitiligo: a review. Dermatology 2001;202:162-6.
[Google Scholar]
|
| 39. |
Yar M, Gilchrist B. Vitiligo. The evolution of cultured epidermal autografts and other surgical treatment modalities. Arch Dermatol 2001;137:348-9.
[Google Scholar]
|
| 40. |
Mahajan BB, Garg G, Gupta RR. Evaluation of cosmetic tattooing in localised stable vitiligo. Int J Dermatol 2002;29:726-30.
[Google Scholar]
|
| 41. |
Gupta S, Kumar B. Epidermal grafting in vitiligo: influence of age, site of lesion and type of disease on outcome. J Am Acad Dermatol 2003;49:99-104.
[Google Scholar]
|
| 42. |
Savant SS. Cultured and non-cultured epidermal cell transplantation. In: Savant SS, editor. Textbook of dermatosurgery and cosmetology. 2nd edn. Mumbai: ASCAD; 2005. p. 387-93.
[Google Scholar]
|
Fulltext Views
6,251
PDF downloads
2,148





