Translate this page into:
Sweet syndrome induced by epidermal growth factor receptor (EGFR) inhibitors
Corresponding author: Dr. Wai Sze Agnes Chan, Assistant Professor, Department of Medicine and Therapeutics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong, China. agneswschan@cuhk.edu.hk
-
Received: ,
Accepted: ,
How to cite this article: Cheung CMT, Li JJX, IP EC, Chan WSA. Sweet syndrome induced by epidermal growth factor receptor (EGFR) inhibitors. Indian J Dermatol Venereol Leprol 2022;88:664-666.
Sir,
Epidermal growth factor receptor inhibitors are associated with multiple cutaneous toxicities, with PRIDE (papulo-pustules or paronychia, regulatory abnormalities of hair growth, itching and dryness) syndrome being the most frequently observed adverse cutaneous effect.1 We report a case of Sweet syndrome induced by epidermal growth factor receptor inhibitors.
A 72-year-old woman, with recently diagnosed stage IV epidermal growth factor receptor-mutated non-small-cell lung carcinoma, was admitted to Prince of Wales Hospital in Hong Kong for painful rashes for five days and a fever of one-day duration. Two weeks before admission, she was started on oral erlotinib 150 mg daily. She was not on any other medication.
On admission, her vitals were stable (blood pressure 162/93 mmHg and heart rate 101 beats per minute). She was febrile with a temperature of 38.1°C. Clinical examination revealed multiple erythematous, edematous papules and plaques with bullae and pustules on her trunk and limbs, with involvement of palms and soles. There was no mucosal lesion. Systemic examination did not show any clinical evidence of internal organ involvement.
Complete hemogram, peripheral smear and renal and liver function tests were within normal limits. Her total leukocyte count was 8000 cells/mm3 with 73% of neutrophils. The absolute eosinophil count was 100 cells/mm3. C-reactive protein was moderately elevated at 26.5 mg/L. Chest radiography did not reveal any new abnormality.
The patient was initially managed as a papulopustular eruption due to erlotinib, with secondary infection. Erlotinib was withdrawn and treatment was started with doxycycline 100 mg twice a day orally and amoxicillin-clavulanic acid combination 1.2g intravenously 8 hourly. Blood and urine cultures were sterile. Deoxyribonucleic acid polymerase chain reaction analysis on vesicle fluid tested negative for herpes simplex virus 1 and 2 and varicella-zoster virus. On day five of admission, culture from a pustule showed scanty growth of Morganella morganii, sensitive to cefotaxime and the antibiotic was changed to intravenous cefotaxime 1g 8 hourly. However, her skin lesions and fever persisted despite three days of cefotaxime. Intravenous meropenem 1g 8 hourly was started, and cefotaxime was discontinued. Repeat blood and pus cultures were sterile. The patient received meropenem for 14 days. Her skin lesions and fever slowly subsided over three weeks of hospitalisation.
After complete resolution of symptoms, the patient was started on oral osimertinib 80 mg daily, along with oral doxycycline 100 mg twice a day for prevention of epidermal growth factor receptor inhibitor-induced papulopustular eruption. Twenty days after initiation of osimertinib, the patient again developed multiple, tender, erythematous and edematous papules and plaques studded with bullae and pustules on the trunk, limbs, palms and soles [Figures 1a and b]. Urine and blood cultures were sterile. Bacterial and fungal cultures carried out on swabs from pustules were negative. Deoxyribonucleic acid polymerase chain reaction analysis from a pustule on the forearm was negative for herpes simplex virus 1 and 2 and varicella-zoster virus. Skin biopsy from an edematous papule on the leg showed focal epidermal necrosis with collections of neutrophils, intra-epidermal vesicles, marked papillary oedema and diffuse dermal neutrophilic infiltrate with nuclear dust [Figure 2]. A diagnosis of drug-induced Sweet syndrome was made. Prednisolone 30 mg daily was started and the patient became afebrile after three days, with skin lesions completely resolving in two weeks. Prednisolone was then tapered by 10 mg every two weeks and was completely stopped after a six-week treatment course. Osimertinib was subsequently restarted orally at a lower dose of 80 mg every other day, along with oral prednisolone 5 mg daily. There was an infrequent recurrence of erythematous papules afterwards, but no fever was noted. The patient decided to continue with osimertinib as symptoms were self-limiting and tolerable.

- Multiple erythematous and edematous papules and plaques with bullae and pustules on the forearm of a patient following osimertinib

- Multiple erythematous and edematous papules and plaques with bullae and pustules on the foot of a patient following osimertinib
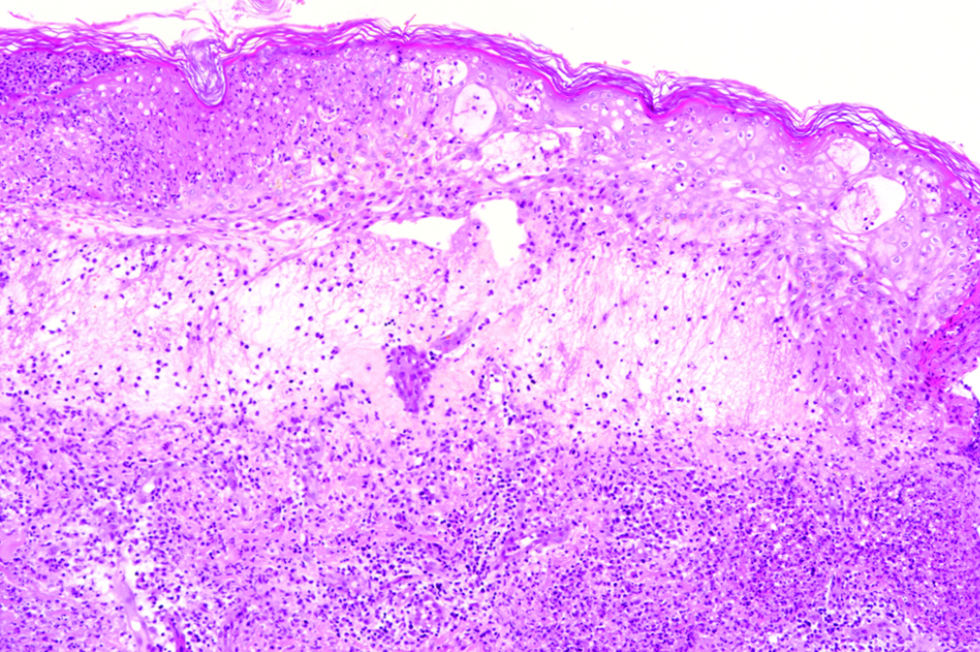
- Skin biopsy from an edematous papule on the leg showing focal epidermal necrosis with collections of neutrophils, intra-epidermal vesicles, marked papillary oedema and diffuse dermal neutrophilic infiltrate with nuclear dust (H and E, × 100)
Sweet syndrome, also known as acute febrile neutrophilic dermatosis, is a rare inflammatory disease characterised by acute onset of painful erythematous plaques or nodules, pyrexia and dense neutrophilic infiltrates in histology.2 It can be subclassified into classical, malignancy-associated and drug-induced Sweet syndrome, among which drug-induced Sweet syndrome is the least frequent form, accounting for less than 5% of all cases.3 Common culprits include granulocyte-colony stimulating factor and all-trans retinoic acid, but it has been reported following several other drugs.2-4
We were unable to find any previous reports of epidermal growth factor receptor inhibitors-induced Sweet syndrome. The patient had a score of five on Naranjo adverse drug reaction probability scale, indicating a probable drug reaction.5 Our case fulfils the diagnostic criteria of drug-induced Sweet syndrome proposed by Walker and Cohen, with typical symptoms and histological findings, compatible temporal relationship between drug intake and clinical presentation, and an excellent response to systemic steroids.2 Although skin biopsy was not performed during the patient’s initial presentation, it is highly likely that she suffered from Sweet syndrome instead of epidermal growth factor receptor inhibitor-related papulopustular eruption with secondary infection, given the fact that her fever was unresponsive to appropriate culture and sensitivity-guided antibiotics, with same symptoms reappearing on re-challenge with another epidermal growth factor receptor inhibitor. The exact pathogenesis of drug-induced Sweet syndrome is unclear and is considered multifactorial. Postulated mechanisms include drug-related direct neutrophilic activation and drug hypersensitivity reaction, with underlying immune dysregulation and genetic predisposition.2 Of note, FMS-like tyrosine kinase 3 inhibitor targeted therapy for acute myeloid leukaemia, has been reported to cause drug-induced Sweet syndrome. It induces the maturation of myeloid blasts to neutrophils with dermal localization, which is proposed to be the mechanism causing Sweet syndrome.2 Erlotinib was shown to possess FMS-like tyrosine kinase 3 inhibitory activity in a preclinical study,6 and this might explain its pathomechanism in inducing Sweet syndrome. However, similar action has not been reported for osimertinib. Epidermal growth factor receptor inhibitors are well-known to cause papulopustular eruptions due to inhibition of keratinocyte proliferation, differentiation and survival, and subsequent inflammatory response with abundant neutrophils.7 Whether this neutrophilic activation contributes to the development of Sweet syndrome remains to be determined, but given the rarity of epidermal growth factor receptor-induced Sweet syndrome, it is postulated that this is more likely to be a hypersensitivity reaction than a direct toxic effect of the drug. Nonetheless, oncologists and dermatologists should be aware of this uncommon adverse event of epidermal growth factor receptor inhibitors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- The PRIDE (Papulopustules and/or paronychia, regulatory abnormalities of hair growth, itching, and dryness due to epidermal growth factor receptor inhibitors) syndrome. Br J Dermatol. 2006;155:852-3.
- [CrossRef] [PubMed] [Google Scholar]
- New practical aspects of sweet syndrome. Am J Clin Dermatol 2022:1-18.
- [CrossRef] [PubMed] [Google Scholar]
- Sweet’s syndrome – a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2:34.
- [CrossRef] [PubMed] [Google Scholar]
- A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239-45.
- [CrossRef] [PubMed] [Google Scholar]
- Erlotinib is effective against FLT3-ITD mutant AML and helps to overcome intratumoral heterogeneity via targeting FLT3 and Lyn. FASEB J. 2020;34:10182-90.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanisms of cutaneous toxicities to EGFR inhibitors. Nat Rev Cancer. 2006;6:803-12.
- [CrossRef] [PubMed] [Google Scholar]





