Translate this page into:
Symmetrical drug-related intertriginous and flexural exanthema due to codeine
2 Department of Pathology, Namık Kemal University, Faculty of Medicine, Tekirdag, Turkey
Correspondence Address:
Gamze Erfan
Department of Dermatology, Namik Kemal University, Faculty of Medicine,Tunca Str. 100. Yil District, Tekirdag
Turkey
| How to cite this article: Erfan G, Yanik ME, Kaya S, Tasolar K, Oznur M, Kulac M. Symmetrical drug-related intertriginous and flexural exanthema due to codeine. Indian J Dermatol Venereol Leprol 2015;81:405-406 |
Sir,
Symmetrical drug-related intertriginous and flexural exanthema (SDRIFE), also known as baboon syndrome, lies within the spectrum of systemically induced allergic contact dermatitis. In recent decades, hundreds of drugs have been reported as being causative agentsof this disease. [1] However, we were unable to find any previous reports of codeine causing this reaction pattern.
A 60-year-old woman presented with a 4-day history of a pruritic, partly confluent, macular rash originating in the gluteal and inguinal area which rapidly progressed to the popliteal area, legs, neck and inframammary area. The rash had developed 2 days after first administration of paracetamol 500mg/codeine 30 mg (Geralgine-K®; Munir Sahin, Turkey), which was used to treat joint pain with a suspicion of psoriatic arthritis. The patient also mentioned that the redness had regressed in the gluteal and inguinal area 2 days earlier. Two months before this episode, the patient had applied topical diclofenac/codeine (Diclactive® 1% gel; Pharmactive, Turkey) for a period of three weeks. There were no other systemic symptoms such as fever or fatigue. Physical examination revealed a symmetrical, erythematous, macular rash on the neck, inframammary area, and the lower and upper extremities [Figure - 1]a. Detailed laboratory and serological investigations for drugs and viral infections were normal. Skin biopsy revealed spongiosis, eosinophilic and lymphocytic exocytosis in the epidermis and a dermal perivascular infiltrate of inflammatory cells, predominantly eosinophils and lymphocytes [Figure - 2]. After discontinuation of the drug, the lesions resolved without treatment within 5 days. Three weeks after the lesions resolved, patch tests with European Baseline Series S-1000 (Chemotechnique Diagnostics®), paracetamol (5% pet.), codeine phosphate (5% and 1% pet.), and Geralgine-K (50% aq., 5% and 1% pet.) were negative, as were prick tests. A provocation test was done with paracetamol; 500 mg/day was administrated for 3 days, and in the 3-week follow-up there were no symptoms. Paracetamol 500 mg/codeine 30 mg was then given. One day after this; mildly pruritic erythema occurred in the neck and waist folds [Figure - 1]b. The patient was thus diagnosed with symmetrical drug-related intertriginous and flexural exanthema due to codeine, based on the clinical features and drug provocation tests.
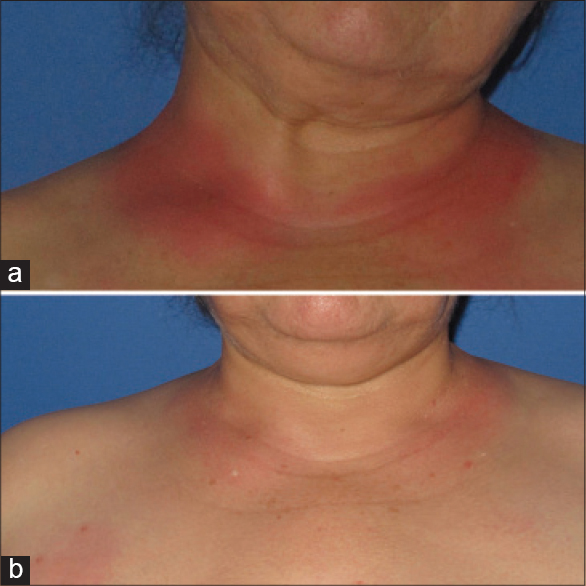 |
| Figure 1: Symmetrical, erythematous, macular rash in intertriginous areas (a) 5 days after codeine administration, (b) 3 days after challenge test with codeine. |
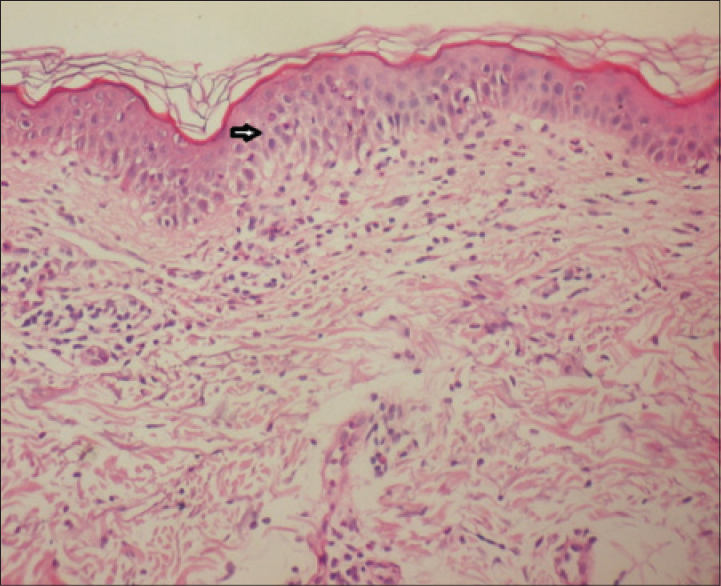 |
| Figure 2: Eosinophilic and lymphocytic exocytosis and spongiosis in the epidermis accompanied by a dermal perivascular infiltrate of inflammatory cells. (H and E, ×200) |
Baboon syndrome was first described as a skin eruption in the intertriginous areas caused by systemic absorption of agents after cutaneous sensitization. Diagnosis is based upon exposure to a systemically administered drug, sharply demarcated erythema of the gluteal area and/or V-shaped erythema of the inguinal area, involvement of at least one other intertriginous site/flexural fold, symmetry of affected areas and the absence of systemic symptoms and signs. [1] The morphology of the rash is considered characteristic. Histopathological findings typically include perivascular infiltrates of inflammatory cells such as lymphocytes and eosinophils. In the present case, all these criteria were fulfilled. Even though codeine is an opioid agonist with a lower incidence of side effects compared with other derivatives, cutaneous side effects such as urticaria, maculo-papular eruptions, angioedema, erythema multiforme, erythema nodosum and toxic epidermal necrosis have all been reported. [2] Generalized contact dermatitis and erythroderma due to type IV hypersensitivity to codeine, have also been reported. [2],[3],[4] Interestingly, in all of the cases mentioned above, patients had a positive patch test for codeine or its derivatives. This data suggests that codeine, which is frequently used by patients in combination with other drugs, can induce late drug allergic reactions such as allergic contact dermatitis.
The pathological mechanism in symmetrical drug-related intertriginous and flexural exanthema is not yet understood; it has been clinically, histologically and immunologically accepted as a type IV drug reaction. [5] In this case, we believe that the history of topical codeine gel administration two months before the eruption may have been responsible for the patient′s sensitization to systemic codeine. Even though symmetrical drug-related intertriginous and flexural exanthema is triggered by systemic absorption of topical or systemic substances, in previously sensitized patients, negative patch tests for the responsible drug have been reported, as was the finding in our case.
| 1. |
Hausermann P, Harr T, Bircher AJ. Baboon syndrome resulting from systemic drugs: Is there strife between SDRIFE and allergic contact dermatitis syndrome? Contact Dermatitis 2004;51:297-310.
[Google Scholar]
|
| 2. |
Schmutz JL, Barbaud A, Trechot P. Codeine and cutaneous drug reactions: Absence of cross-allergy with tramadol and fentanyl. Ann Dermatol Venereol 2010;137:429.
[Google Scholar]
|
| 3. |
Rodriguez A, Barranco R, Latasa M, de Urbina JJ, Estrada JL. Generalized dermatitis due to codeine. Cross-sensitization among opium alkaloids. Contact Dermatitis 2005;53:240-4.
[Google Scholar]
|
| 4. |
Gastaminza G, Audicana M, Echenagusia MA, Uriel O, Garcia-Gallardo MV, Velasco M, et al. Erythrodermia caused by allergy to codeine. Contact Dermatitis 2005;52:227-8.
[Google Scholar]
|
| 5. |
Wolf R, Orion E, Matz H. The baboon syndrome or intertriginous drug eruption: A report of eleven cases and a second look at its pathomechanism. Dermatol Online J 2003;9:2.
[Google Scholar]
|
Fulltext Views
4,797
PDF downloads
2,503





