Translate this page into:
Syphilis renaissance: Truth or mirage. Analysis of syphilis trends and possible factors from a tertiary care centre in North India
Corresponding author: Dr. Sanjeev Handa, Department of Dermatology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. handa_sanjeev@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Baskaran N, Kumaran MS, Narang T, Handa S. Syphilis renaissance: Truth or mirage. Analysis of syphilis trends and possible factors from a tertiary care centre in North India. Indian J Dermatol Venereol Leprol. 2025;91:356-62. doi: 10.25259/IJDVL_420_2024
Abstract
Background
Syphilis has shown a recent resurgence globally, including in India. However, inconsistency in the data and diagnostic criteria used, especially in India and developing countries, hinders ideal understanding. Factors responsible for this surge need to be explored.
Objectives
This study aimed to assess the trends and describe the clinicodemographic characteristics of syphilis cases seen in a tertiary care health centre from Northern India.
Methods
This is a retrospective chart review of syphilis patients registered in our sexually transmitted infection (STI) clinic spanning 13 years from January 2011 to December 2023. Complete demographic details, sexual history, clinical examination and laboratory investigations of all syphilis cases, including associated STIs, were retrieved.
Results
The retrospective analysis included 2000 records, of which 324 were confirmed syphilis cases (16.2% of total STI cases). Patients’ mean age was 30.9 ± 9.9 years, of which 80.9% were male and 64.2% were married. Education level varied, with professionals comprising 22.2% of the total cohort. Premarital and extramarital exposure were present in 35.8% and 32.7% patients, respectively; over half (56.8%) reported multiple partners and 13% were homosexual. There was an initial plateau in the number of confirmed syphilis attending the clinic (2011–2019), a decrease during 2020–2021 due to COVID and significant increase from 2022 onwards. Latent syphilis was the most common (66.7%), followed by secondary (18.8%) and primary (8.9%). In all, 36.1% of syphilis patients had associated STIs, with human immunodeficiency virus (HIV) infection being the most prevalent (25.0%).
Limitation
Retrospective nature of the study is major limitation. Rising trend needs validation with population-based studies to establish if the rise is true or a shadow phenomenon.
Conclusion
A resurgence of syphilis cases has appeared in the past two years, with latent syphilis contributing to the majority of cases. Possible factors for the surge include changing sexual behaviour, including male having sex with male (MSM), early adolescent sexual exposure, increased screening for latent syphilis, increased healthcare accessibility post-COVID-19 pandemic, and HIV co-infection.
Keywords
Syphilis
STI
MSM
resurgence
sexual behaviour
epidemiology
Introduction
Syphilis is a sexually transmitted multisystem bacterial infection caused by Treponema pallidum subsp. pallidum. There was a global decline in the incidence of syphilis post-1990, which can be attributed to the increase in safe sex practices as a result of the ongoing human immunodeficiency virus (HIV) pandemic.1,2 However, recent data from the global literature, especially the last decade, gives an impression of its re-emergence as a major public health problem.3–5 There is wide variation in the syphilis prevalence rates in various countries, including India.3–9 In 2016, the World Health Organisation released global targets for reducing the health impact of sexually transmitted infections by 2030.10 However, there is a lack of robust data on the prevalence of syphilis, especially from India and other developing countries; there are significant variations in data from different parts of India on the diagnosis and prevalence of syphilis.6–9,11–15
This study explores the trend in syphilis over 13 years at our tertiary care institute, including the clinicodemographic characteristics, sexual behaviour, clinical stage, and serology.
Methods
This is a retrospective chart review, analysing medical records of all sexually transmitted infections (STIs) cases registered in the STI clinic between January 2011 and December 2023, of which only confirmed cases of syphilis were included.
Complete demographic details, including age, sex, marital status, education, and occupation of the cases, were retrieved from the filled STI proformas. Complete sexual history, clinical examination findings, laboratory investigations, treatment administered, and co-existing STIs were also recorded. Data were entered in Microsoft Excel and statistical analysis was performed using SPSS software 29.0.1.0.
Results
Clinicoepidemiological parameters and trends of syphilis cases
In total, 2000 records were retrieved from the STI clinic, of which 324 (16.2%) patients were confirmed cases of syphilis.
The mean age of patients was 30.9 ± 9.9 years, with a male: female ratio of 4.2:1. Almost two-thirds were married (n = 208, 64.2%). There were 22 pregnant women, referred from antenatal clinics. Regarding education, 30.5% (n=99) were graduates or postgraduates, 34.3% (n=111) had completed higher secondary schooling/ diploma, 30.9% (n=100) had studied only up to primary/mid/high school, and illiterates were only 4.3% (n=14). The commonest occupation was professionals (n=72, 22.2%), others included various skilled, semi-skilled, and unskilled workers (n=151, 46.6%), students (n=45, 13.9%), and housewives (n=44, 13.6%).
During the initial years, there was a steady number of syphilis patients visiting us, followed by a decrease during 2020–2021 possibly owing to the COVID pandemic. However, since 2022, there has been a significant spike in cases [Figure 1]. Syphilis constituted 22.59% (47/208) and 21.99% (75/341) of all STI cases during these years.

- Line diagram showing the trend of total STI and syphilis cases over the past 13 years. (STI: Sexually trasnmitted infections)
The most common stage of presentation was latent syphilis of unknown duration in 66.7% (216/324) of patients, with most presenting between 2022 and 2023 (67/216, 31%) [Figure 2]. We also noted a significant rise in primary and secondary syphilis during the same years.
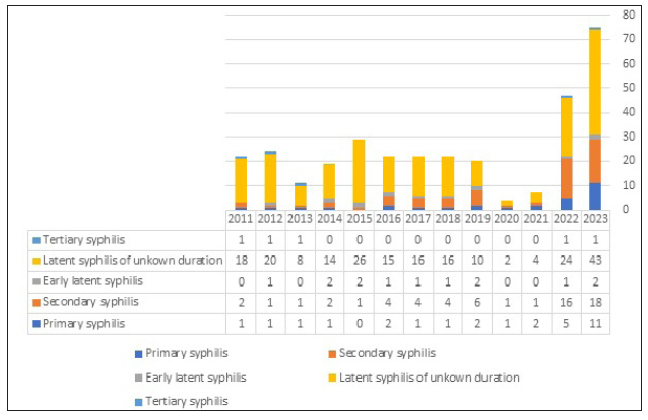
- Bar diagram showing the distribution of syphilis cases across various stages over the past 13 years.
Sexual history
Premarital and extramarital exposure were present in 35.8% (n = 116) and 32.7% (n = 106) cases, respectively [Table 1]. Exposure to multiple partners was seen in more than half of the study cohort (n = 184, 56.8%). Homosexuality was noted in 42 (13%) patients, and 26 (8%) patients were bisexual. Most patients practised unprotected sexual exposure (n = 297, 91.7%).
| Variables | Primary syphilis (n = 29) | Secondary syphilis (n = 61) | Latent syphilis (n = 229) | Tertiary syphilis (n = 5) | Total (n = 324) |
|---|---|---|---|---|---|
| Age in years (Mean ± SD) | 26.7 ± 8.3 | 29.7 ± 11.8 | 31.6 ± 9.4 | 37.7 ± 7.5 | 30.9 ± 99 |
| Gender | |||||
| Males | 27(93.1) | 56(91.8) | 175(76.4) | 4(80) | 262(80.9) |
| Females | 2(6.9) | 5(8.2) | 54(23.6) | 1(20) | 62(19.1) |
| Partners other than spouse | |||||
| Casual | 5(17.2) | 17(27.9) | 42(18.3) | 1(20) | 65(20.1) |
| Friend | 13(44.8) | 22(36.1) | 68(29.7) | 1(20) | 104(32.1) |
| Relative | 2(6.9) | 2(3.3) | 5(2.2) | 1(20) | 10(3.1) |
| CSW | 4(13.8) | 11(18.0) | 36(15.7) | - | 51(15.7) |
| Sexual orientation | |||||
| Heterosexual | 22(75.9) | 44(72.1) | 178(77.7) | 4(80) | 248(76.5) |
| Homosexual | 5(17.2) | 10(16.4) | 27(11.8) | - | 42(13.0) |
| Bisexual | 2(6.9) | 7(11.5) | 16(7.0) | 1(20) | 26(8.0) |
| Route of exposure | |||||
| Genito-genital | 21(72.4) | 39(63.9) | 174(76.0) | 4(80) | 238(73.5) |
| Genito-oral | - | - | 4(1.7) | - | 4(1.2) |
| Peno-rectal | 3(10.3) | 8(13.1) | 17(7.4) | - | 28(8.6) |
| Combination | 5(17.2) | 14(22.9) | 26(11.4) | 1(20) | 46(14.2) |
| STIs in partner | |||||
| Yes | 3(10.3) | 1(1.6) | 45(19.7) | 1(20) | 50(15.4) |
| No | 3(10.3) | 5(8.2) | 26(11.4) | 1(20) | 35(10.8) |
| Unaware | 23(79.3) | 55(90.2) | 150(65.5) | 3(60) | 231(71.3) |
| Genital ulcer location | - | - | - | ||
| Glans penis | 13(44.8) | 13(4.0) | |||
| Prepuce | 6(20.7) | 6(1.9) | |||
| Coronal sulcus | 6(20.7) | 6(1.9) | |||
| Shaft of penis | 2(6.9) | 2(0.6) | |||
| Labia minora | 2(6.9) | 2(0.6) | |||
| Skin rash morphology | - | - | - | ||
| Papulosquamous | 21(34.4) | 21(6.5) | |||
| Maculopapular | 20(32.8) | 20(6.2) | |||
| Psoriasiform | 7(11.5) | 7(2.2) | |||
| Macular | 7(11.5) | 7(2.2) | |||
| Papular | 3(4.9) | 3(0.9) | |||
| Ulceronecrotic nodules/plaques | 3(4.9) | 3(0.9) | |||
| Mucosal involvement | - | - | - | ||
| Mucosal ulcers | 5(8.2) | ||||
| Mucous patch | 1(1.6) | ||||
| Condyloma lata | 5(8.2) | ||||
| VDRL test Reactive | 27(93.1) | 61(100) | 224(97.8) | 5(100) | 317(97.8) |
| Median VDRL titre | 1:16 | 1:32 | 1:4 | 1:16 | 1:8 |
| TPHA Positive | 27(93.1) | 61(100) | 229(100) | 5(100) | 322(99.4) |
| VDRL reactive and TPHA positive | 26 (89.6) | 61 (100) | 224 (97.8) | 5 (100) | 316(97.5) |
| HIV infection | 5(17.2) | 20(32.8) | 53(23.1) | 3(60) | 81(25) |
SD: Standard deviation, CSW: Commercial sex worker, STI: Sexually transmitted infections, TPHA: Treponema pallidum hemagglutination assay, VDRL: Venereal disease research laboratory
Analysis of individual parameters in various stages of syphilis
Primary syphilis
A total of 29 patients had primary syphilis. A single ulcer was present in 75.9% (n = 22) [Figure 3a], whereas the remaining patients had more than one ulcer (n = 7, 24.1%) [Figure 3b]. Dark ground microscopy demonstrated treponemes with classical corkscrew motility in four cases.

- Single well-defined indurated ulcer with clean base over the prepuce in patients with primary syphilis.

- Multiple well-defined ulcers over the glans penis and prepuce.
Secondary syphilis
Sixty-one patients had secondary syphilis. The most common morphology was papulosquamous eruption in 21 cases (34.4%) [Figure 4a], followed by maculopapular (n = 20, 32.8%) [Figure 4b], psoriasiform (n = 7, 11.5%) [Figure 4c], macular (n = 7, 11.5%) [Figure 4d] and papular (n = 3, 4.9%) rash. There were three (4.9%) patients with malignant syphilis. Special patterns included annular plaques in two patients, lichenoid plaques, hyperkeratotic plaques, corymbose arrangement of papules [Figure 4e], and moth-eaten alopecia in one patient each. Oral ulcers and condyloma lata affecting the natal cleft were seen in five cases each, and mucous patch in one patient [Figure 4f]. Biopsy findings were available for three cases, including two cases of malignant syphilis. All cases showed psoriasiform hyperplasia with dense infiltrates of plasma cells, lymphocytes, and histiocytes in the dermis.

- Multiple well-defined erythematous to brown papulosquamous plaques with Biett collarette over the palms and soles in a patient with secondary syphilis.

- Multiple brownish hyperpigmented macules and papules over the palms and soles in a patient with secondary syphilis.

- Multiple well-defined psoriasiform plaques over the palms in a patient with secondary syphilis.
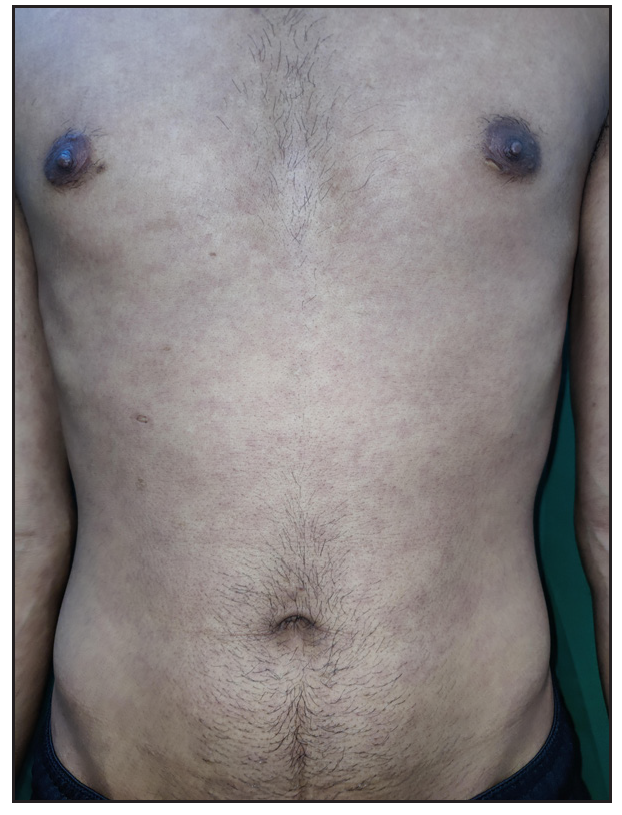
- Copper-coloured macules over the trunk in a patient with secondary syphilis.

- Multiple lichenoid papules and plaques in a Corymbose arrangement over the trunk in a patient with secondary syphilis.

- Mucous patches in a patient with secondary syphilis.
Latent syphilis
There were 229 (70.7%) patients with latent syphilis. The majority were incidentally detected during screening for blood donation (n = 37, 16.2%), antenatal screening (n = 22, 9.6%), screening at anti-retroviral therapy (ART) centre (n = 39, 17.0%), screening of contacts (n = 24, 10.5%) and screening for other indications, including overseas travel (n = 52, 22.7%).
Tertiary syphilis
Five patients with confirmed (positive venereal disease research laboratory [VDRL], median titre of 1:8, and positive cerebrospinal fluid VDRL [CSF-VDRL]) neurosyphilis were referred from the neurology department. Neurological (asymptomatic meningitis) and ocular (uveitis) involvement were seen in three and two patients, respectively.
Overall, the VDRL test was reactive in 97.8% (n = 317) of patients with a median titre of 1:8. TPHA was positive in 99.4% (n=322) patients.
Associated STIs
Among 324 syphilis patients, 117 (36.1%) either presented with an associated STI or gave previous history suggestive of the same. HIV infection was present in 81 (25%). Amongst them, 57 patients had latent syphilis, 19 had secondary syphilis, 2 had primary syphilis and 3 had neurosyphilis. No significant differences in clinical presentation or investigations were noted between HIV infected versus non-infected syphilis patients.
Discussion
Recently, there has been a spurt in literature regarding the steady rise in syphilis incidences.3 This led us to review our department data to assess the trends and note if the increase is true or a mirage. The annual number of syphilis cases remained relatively consistent until 2019, and there was a significant decrease in syphilis incidences between 2020 to 2021 owing to the COVID pandemic. However, since 2022, we noticed a sudden rise in the number of patients with syphilis presenting to us. These trends mirror data from published national and international literature on the prevalence of syphilis in the past decade.3–9 A retrospective study from North India demonstrated a significant increase in syphilis, especially in infectious stages in the past five years.6 An increase in syphilis serological positivity from 0.52% to 2.1% was noted during 2015–2020 in a study from South India11 [Table 2].
| Study | Place | Year/duration | Number of cases | Sex ratio | Age of syphilis patients (years) | Associated STIs | Seropositivity |
|---|---|---|---|---|---|---|---|
| Nishal et al.13 | Haryana, India | 2008–2012 | 91 (6.22% of all STIs) | 6:1 | 18–40 | HIV 8.79% |
VDRL range Primary: 1:8–1:128 Secondary and latent: 1:32–1:256 |
| Jain et al.14 | New Delhi, India | 2005–2009 | 42 (7.36% of all STIs) | 2.3:1 | 17–46 (mean age 27) | - | VDRL positive in all cases, median titre 1:16 |
| Shah et al.7 | Ahmedabad, Gujarat, India | 2013–2014 | 110 (10.9% of all STIs) | 2.4:1 | 21–40 |
HIV: 24.5% Genital herpes: 44.8% Condyloma acuminate: 27.6% Molluscum: 17.2% Chancroid: 10.3% |
RPR reactivity in 72.7% (most common 1:16) TPHA positive in 84.5% |
| Solaimalai et al.11 | Vellore, Tamilnadu, India | 2015–2020 | 265 | 4.63:1 | Mean age 36 ± 10.2 |
HIV: 23% Genital herpes: 2.3% Hepatitis B: 2.3% Hepatitis C: 0.8% Gonococcal urethritis: 0.4% |
VDRL positive in all patients |
| Gupta et al.6 | Shimla, Himachal Pradesh, India | 2012–2022 | 31 (0.99% of all STI cases) | 3:1 | Mean age 35 | HIV: 12.9% |
RPR less than 1:32 51.6% RPR more than 1:32 48.4% |
| Ahuja et al.18 | New Delhi, India | 2015–2023 | 41 (7.2% of STI cases) in 2015 to 150 (20.86% of STI cases) in 2022 | Increase more marked in male attendees | - | - | - |
| Our study | North India | 2011–2023 | 324 (16.2% of all STI cases, increase from 17.7% in 2011 to 21.99% in 2023) | 4.2:1 | Mean age 30.9 ± 99 |
HIV: 25% Genital herpes: 2.8% Anogenital warts: 6.5% Molluscum: 2.8% Urethritis: 1.2% Vaginal/cervical discharge: 1.2% Hepatitis B: 1.2% Hepatitis C: 1.5% |
VDRL positive in 96.3% TPHA positive in 99.4% |
STI: Sexually transmitted infections, TPHA: Treponema pallidum hemagglutination assay, RPR: Rapid plasma reagin test, VDRL: Venereal disease research laboratory
Globally, the burden of syphilis has increased at a rate of approximately 60% from 1990 to 2019.3 An increasing prevalence has been reported, especially post-2015, in countries including Canada, the United States, England, and Australia.4,5,16,17 The global data from 1990 to 2019 showed that South Asia had recorded the highest number of incident cases of syphilis, with a 59.7% increase in 2019 as compared to 1990.3
On a closer look, there was an increase in patients with latent syphilis. This could be attributed to screening while travelling abroad for occupation and vacation, and robust screening and referral from blood banks and antenatal clinics. An increased health-seeking behaviour and healthcare accessibility post-COVID-19 pandemic could have also contributed to the increase. Other possible reasons include asymptomatic lesions, misdiagnosis of early infectious stages, easy availability and injudicious use of antibiotics, use of indigenous medications leading to partial improvement and progression to subsequent stages, and finally the self-healing nature of the early disease. A similar increase has also been reported from a tertiary care centre in New Delhi, where online sexual activity during the lockdown and redirected healthcare resources were proposed as possible factors.18 However, in addition, there was also an increase in patients with infectious syphilis.
There are many other factors proposed for the increase in the incidence of syphillis. The peak age of incidence was 25–29 years in the global data, which is similar to our study.3 Mean age of cases with primary syphilis was 26 years, which was lower than that for other stages. Early onset of sexual exposure among adolescents could be attributed as one of the potential reasons for an increasing number of infectious syphilis. As reported by UDAYA (Understanding the Lives of Adolescents and Young Adults) survey conducted in 2015–2016, school dropouts, frequent media exposure and exposure to pornography contribute to early sexual debut.19 The increasing availability of dating apps and substance abuse among adolescents may also explain the rising trends of syphilis.20–24
A high proportion of graduates (45.1%) and literates (80%) has been reported in previous studies,6,14 which could be attributed to the increased health-seeking behaviour of the literate population.6 Higher rates have been reported among MSM population, similar to our study,3,4 whose proportion increased from 17.8% in 2012–2020 to 26.2% in 2022–2023, demonstrating a changing sexual behaviour as one of the potential aetiologies for the increase in incidences.
HIV co-infection was present in 25% of cases, which is higher than that reported in previous Indian studies.7–9,11–14 This could also be a potential contributory factor for the rising syphilis cases and vice versa, as the common high-risk behaviour, mucosal breach and inflammation predispose syphilis cases to acquiring HIV infection.25
The strengths of this study include a notably large cohort from comprehensive demographic data, including clinical information and laboratory test details.
Limitation
The limitations of the study include its retrospective study design. Rising trends were noticed; however, this needs further validation with population-based studies to establish whether the rise is true or a shadow phenomenon.
Conclusion
There has been an increase in the number and proportion of syphilis cases, especially latent syphilis, in the past two years. This increase follows a stable number of cases in the past decade. Factors contributing to this recent increase include rising latent syphilis due to increased screening, increased healthcare accessibility post-COVID-19 pandemic, changing sexual behaviours, particularly among MSM, early adolescent sexual exposure, and gaps in sexual health education. Further population-based multicentre studies are required from India to confirm the exact rising trends of syphilis.
Ethical approval
The ethical approval was obtained from the Institutional Ethics Committee (INT/IEC/2024/Spl.952) for the study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Surveillance for primary and secondary syphilis—United States, 1991. MMWR CDC Surveill Summ. 1993;42:13-9.
- [PubMed] [Google Scholar]
- Trends in primary and secondary syphilis among men who have sex with men in the United States. Am J Public Health. 2007;97:1076-83.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Global, regional, and national trends of syphilis from 1990 to 2019: The 2019 global burden of disease study. BMC Public Health. 2023;23:754.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Rising syphilis rates in Canada, 2011–2020. Can Commun Dis Rep. 2022;48:52-60.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Genomic epidemiology of syphilis in England: A population-based study. Lancet Microbe. 2023;4:e770-80.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The changing trend of syphilis: Is it a sign of impending epidemic? Indian J Dermatol. 2023;68:15-24.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Syphilis: Is it making resurgence? Indian J Sex Transm Dis AIDS. 2015;36:178-81.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Rising trends of syphilis in a tertiary care center in North India. Indian J Sex Transm Dis AIDS. 2015;36:140-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Let’s not let the guard down! – Early indications of syphilis resurgence? Indian J Dermatol Venereol Leprol. 2019;85:246-7.
- [CrossRef] [PubMed] [Google Scholar]
- Global health sector strategy on Sexually Transmitted Infections, 2016–2021. Geneva, CH: WHO; 2016.
- Upward trends of syphilis in the non-pregnant adults: A six-year report on clinical and epidemiological profile of syphilis from a tertiary care center, India. Front Public Health. 2022;10:908591.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Syphilis in the era of re-emergence: A 6-year retrospective study from a tertiary care center in South India. Indian J Sex Transm Dis AIDS. 2022;43:165-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Changing trends in acquired syphilis at a tertiary care center of North India. Indian J Sex Transm Dis AIDS. 2015;36:149-53.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Current status of acquired syphilis: A hospital-based 5-year study. Indian J Sex Transm Dis AIDS. 2012;33:32-4.
- [CrossRef] [PubMed] [Google Scholar]
- Syphilis on the rise: A series of 12 cases with mucocutaneous features over a short span. Indian J Dermatol Venereol Leprol. 2021;87:321.
- [CrossRef] [PubMed] [Google Scholar]
- Expanded HIV pre-exposure prophylaxis (PrEP) implementation in communities in New South Wales, Australia (EPIC-NSW): Design of an open label, single arm implementation trial. BMC Public Health. 2018;18:210.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- National Overview – Sexually transmitted disease surveillance, 2019. Atlanta (GA): CDC; 2021. https://www.cdc.gov/std/statistics/2019/overview.htm. [Accessed March 01, 2024]
- The shadow pandemic: Rising syphilis rates in the wake of coronavirus (COVID-19) Sex Health. 2024;21:SH23189.
- [CrossRef] [PubMed] [Google Scholar]
- What predicts the early sexual debut among unmarried adolescents (10–19 years)? Evidence from UDAYA survey, 2015–16. PLoS One. 2021;16:e0252940.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Collateral damage: A narrative review on epidemics of substance use disorders and their relationships to sexually transmitted infections in the United States. Sex Transm Dis. 2021;48:466-73.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Review of sexualized drug use associated with sexually transmitted and blood-borne infections in gay, bisexual and other men who have sex with men. Drug Alcohol Depend. 2020;216:108237.
- [CrossRef] [PubMed] [Google Scholar]
- Is social media to blame for the sharp rise in STDs? Soc Sci. 2017;6:78.
- [CrossRef] [Google Scholar]
- Online partner seeking and high-risk behaviour in men who have sex with men and male-to-female transgendered people in Mumbai, India: Implications for prevention strategies. PLoS One. 2023;18:e0284602.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Retrospective analysis of demographic factors and changing pattern of clinical features of acquired syphilis at a tertiary care center in South India. Int J Res Dermatol. 2018;4:534-8.
- [CrossRef] [Google Scholar]
- Early syphilis: Risk factors and clinical manifestations focusing on HIV-positive patients. BMC Infect Dis. 2019;19:727.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







