Translate this page into:
Systemic (allergic) contact dermatitis to diclofenac
Correspondence Address:
Chembolli Lakshmi
Department of Dermatology, PSG Hospitals and PSGIMSR, Coimbatore 641 004, Tamil Nadu
India
| How to cite this article: Lakshmi C, Srinivas C R. Systemic (allergic) contact dermatitis to diclofenac. Indian J Dermatol Venereol Leprol 2011;77:536 |
Sir,
We present a case report of a patient who developed aggravation of skin contact sites and generalized pruritic exanthem with constitutional symptoms following both topical and oral exposures to diclofenac. Although diclofenac is widely used, systemic contact dermatitis (SCD) to diclofenac has not been reported. [1]
A 37-year-old woman presented with pruritus, erythema, swelling, and vesiculation over both the knees and lower legs with generalized pruritic urticarial "rash" [Figure - 1], [Figure - 2] and [Figure - 3] of 2 days duration. She complained of malaise, fever, and swelling of the face [Figure - 4].
 |
| Figure 1: Erythema, vesiculation, and swelling over the knees and adjacent parts of lower legs, more on the right knee |
 |
| Figure 2: Symmetrical erythematous plaques over the lower legs |
 |
| Figure 3: Pruritic urticarial papules and plaques over the back |
 |
| Figure 4: Erythema and swelling of the face |
She had sustained trauma over her right knee 18 days back and developed localized pain with swelling. Topical diclofenac was applied for 1 week with resolution of symptoms. The same knee got injured and was prescribed topical diclofenac along with oral diclofenac 50 mg twice daily for 2 days. The topical medication was applied over the affected area, left knee, and the shins. Within 24 h, she developed redness and itching over the knees and lower legs followed by generalized pruritic, urticarial rash associated with facial edema and constitutional symptoms.
SCD to diclofenac was suspected, and she was treated with injection dexamethasone sodium phosphate 8 mg daily for 3 days, antihistamines and topical clobetasol propionate 0.05% ointment over the erythematous areas.
Skin biopsy was done from the erythematous plaque (knee) and from the annular, urticarial plaque (back). The skin lesions regressed within 3-4 days. Patch testing with diclofenac 2.5% was advised, but the patient refused further testing.
Routine investigations were normal. Biopsy from the erythematous plaque over the knee was consistent with allergic contact dermatitis (ACD) [Figure - 5] and from the urticarial plaque was consistent with an exanthematous drug reaction [Figure - 6].
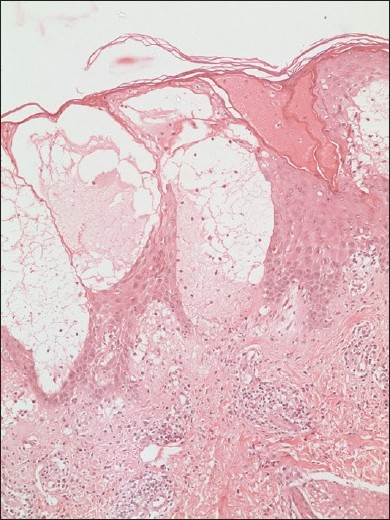 |
| Figure 5: Spongiosis with intraepidermal vesicles perivascular lymphocytic and eosinophilic infiltrate seen throughout the dermis and subcutaneous fat. Few vessels showing lymphocytic infiltration of the wall (H and E stain, ×100) |
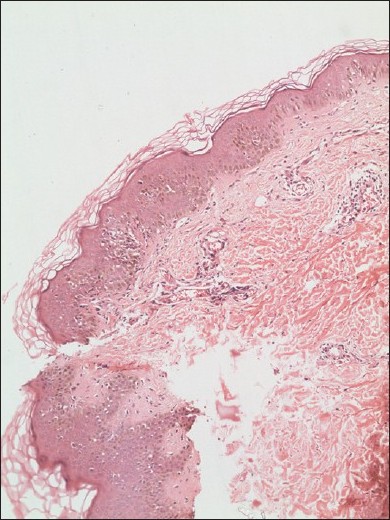 |
| Figure 6: Spongiosis, lymphocytic exocytosis, and interface dermatitis with superficial dermal edema and perivascular lymphocytic infiltration (H and E, ×100) |
SCD may occur after the systemic administration of a hapten (orally, transcutaneously, intravenously, or by inhalation) in sensitized persons. [2] The term "Baboon syndrome" refers to the erythema over the buttocks and inner thighs, [3] and is a characteristic, rare clinical manifestation of SCD. The skin reaction may occur within few hours to days following systemic exposure to the drug. [2] The clinical picture varies from a symmetrical widespread, maculopapular rash, pompholyx with deep-seated vesicles and erythema in the palms and fingers, flare-up of previous dermatitis or previously positive patch test sites, flexural dermatitis, the baboon syndrome, vasculitis-like lesions, erythroderma, exanthema-like toxicoderma and erythema multiforme (EM), or intractable eczema. [1],[2] Systemic symptoms such as headache, fever, malaise, arthralgia, vomiting, and diarrhea may occur. [1],[2] Symmetrical drug-related intertriginous and flexural exanthema, or SDRIFE is a distinctive clinical pattern of drug eruption with five criteria. [4] Our patient did not fulfill the criteria for SDRIFE. The initial application of the diclofenac gel would have sensitized her and subsequent re-application 7-10 days could have resulted in the development of ACD (at application sites) and a systemic reaction as a result of ingestion of the drug. The reaction over the right knee (previously sensitized) was more severe than on the left due to development of SCD following oral challenge with diclofenac. [2] Oral intake acted as an oral challenge, whereas the topical application served as a repeated open application test (ROAT).
Delayed hypersensitivity to diclofenac is confirmed by patch testing. In spite of not performing patch testing, the repeated application of topical diclofenac along with oral challenge fulfilled four of the criteria by Calkin et al. to establish scientific validity. [1]
Both cellular and humoral immune systems (specifically sensitized T-cells and nonspecific cytokine release) are activated in SCD. [2] Flares at previously sensitized sites are probably mediated by specifically sensitized T-cells, resting at the site or reaching the area after specific hapten exposure. [1],[2] The toxicoderma
(skin rash) is attributed to nonspecific cytokine release. [1],[2] Posadas et al. [5] suggested the "p-i concept" where certain small-sized drugs do not form hapten-carrier complexes, but bind directly to T-cell receptors, bypassing the major histocompatibility complex (MHC) molecules, similar to the pharmacological interaction of drugs with immune receptors. [1],[5] These bindings are labile, but sufficient to activate T cells and mimic allergic immune reactions. Interaction with the MHC molecule results in the amplification of the drug-driven T-cell expansion. [2],[5] The p-i concept could explain the development of adverse cutaneous drug reactions (ACDRs) and possibly SCD at the first exposure or within a few hours or days following exposure to the drug. [1],[5]
In our patient, all three pathomechanisms could be operational. Activation of (1) the humoral immune system resulted in constitutional symptoms and skin rash, (2) of the cellular immune system resulted in flare-up of dermatitis at sensitized sites, (3) of the p-i concept resulted in rapid development of clinical signs and symptoms.
| 1. |
Thyssen JB, Maibach HI. Drug-elicited systemic allergic (contact) dermatitis - update and possible pathomechanisms. Contact Dermatitis 2008;59:195-202.
[Google Scholar]
|
| 2. |
Veien NK, Menne T. Systemic Contact dermatitis. In: Frosch PJ, Menne T, Lepoittevin J, editors. Contact Dermatitis. 4 th ed. Berlin: Springer-Verlag; 2006. p. 429-32.
[Google Scholar]
|
| 3. |
Andersen KE, Hjorth N, Menne T. The baboon syndrome: Systemically induced allergic contact dermatitis. Contact Dermatitis 1984;10:97-100.
[Google Scholar]
|
| 4. |
Hausermann P, Harr Th, Bircher AJ. Baboon syndrome resulting from systemic drugs: Is there strife between SDRIFE and allergic contact dermatitis syndrome. Contact Dermatitis 2004;51:297-310.
[Google Scholar]
|
| 5. |
Posadas SJ, Pichler WJ. Delayed drug hypersensitivity reactions - new concepts. Clin Exp Allergy 2007;37:989-99.
[Google Scholar]
|
Fulltext Views
5,474
PDF downloads
3,442





