Translate this page into:
Targeted ultraviolet B phototherapy in vitiligo: A comparison between once-weekly and twice-weekly treatment regimens
Correspondence Address:
Imran Majid
CUTIS Skin Institute, Karan Nagar Chowk, Srinagar - 190 010, Jammu and Kashmir
India
| How to cite this article: Majid I, Imran S. Targeted ultraviolet B phototherapy in vitiligo: A comparison between once-weekly and twice-weekly treatment regimens. Indian J Dermatol Venereol Leprol 2015;81:600-605 |
Abstract
Background: Targeted ultraviolet B (T-UVB) phototherapy in vitiligo is usually administered twice or thrice a week on non-consecutive days. It is difficult for many patients to adhere to this regimen, forcing them to discontinue treatment. Aim: The study aimed to compare the efficacy of twice-weekly and once-weekly targeted ultraviolet B phototherapy regimens in vitiligo. Methods: Sixty patients with non-segmental vitiligo on the face, neck or trunk were divided into two groups of 30 patients each. The patients in group A received targeted ultraviolet B twice weekly, while those in group B received targeted ultraviolet B once weekly. Repigmentation was monitored and graded as excellent (≥75% repigmentation), good (50−74% repigmentation) and poor (<50% repigmentation). The extent of repigmentation at each body site (primary outcome measure), the number of doses required for initiation of pigmentation, and the cumulative dose of targeted ultraviolet B administered was calculated and compared between both groups. Results: A total of 90 lesions (48 in the twice weeklygroup and 42 in the once weekly group) were treated on the face, neck and trunk. Excellent results were obtained in 62.5% (30/48) of lesions treated twice weekly, and 64.3% (27/42) in lesions treated once weekly. The mean number of doses required for initiation of pigmentation was 4.69 in the twice weekly group, and 4.35 in the once weekly group. The patients in the twice weekly group received a mean cumulative dose of 8.26 J/cm 2, while the once weekly group received 7.69 J/cm 2. No statistically significant differences were observed between the two groups with respect to the outcome, with respect to the total repigmentation, the number of doses till onset of pigmentation, as well as the cumulative dose of targeted UVB. Conclusion: Once-weekly targeted ultraviolet B phototherapy appears to be as efficacious as the twice-weekly regimen in vitiligo.Introduction
Vitiligo is one of the most common acquired disorders of skin pigmentation, that affects about 1% of the world population. The disease causes tremendous psychological trauma, especially in people with coloured skin.[1],[2] Treatment of vitiligo is done on two fronts: to control the progress of the disease and to achieve repigmentation in lesions that have already developed. Phototherapy is one of the best known and documented treatment options in vitiligo.[3],[4] Originating with the use of crude psoralens and sun exposure, phototherapy in vitiligo has advanced to psoralens with ultraviolet A, narrowband ultraviolet B, and its combination with topical treatment options, and finally targeted phototherapy with lasers and ultraviolet light.[4],[5],[6],[7],[8] Among the treatment options currently available in vitiligo, targeted phototherapy is one of the most effective, especially in patients with localized vitiligo.[9],[10] As the term denotes, targeted phototherapy specifically targets the lesional skin, while the rest of the skin remains unexposed. As a result, the uninvolved skin remains protected and the lesional skin can be exposed to higher energies, enabling a rapid therapeutic effect.[9],[11] In addition, the adverse effects of whole body irradiation are avoided.
Different targeted phototherapy devices used in vitiligo include the xenon-chloride excimer laser, excimer lamp and targeted ultraviolet devices that deliver broadband ultraviolet B or narrowband ultraviolet B light. Targeted ultraviolet light based therapies employ conventional non-coherent ultraviolet light that is delivered specifically to the treatment area via fiber-optic cable systems.[12],[13] Targeted phototherapy including targeted ultraviolet B (T-UVB) phototherapy is usually administered twice or thrice a week on non-consecutive days. The dose is gradually increased every session until a faint erythema is observed or when the patient develops perifollicular pigmentation.[13],[14],[15] One of the most important limitations of targeted ultraviolet B phototherapy is that the patient needs to come twice or thrice a week for treatment. This interferes with the daily schedule of many patients, making it difficult for them to continue treatment. Once weekly treatment is certainly more convenient and is thus likely to improve patient compliance.
Methods
This study was conducted in 60 patients with stable non-segmental vitiligo over the face, neck and trunk, involving less than 5% of the total body surface area. For the purpose of the present study, stable vitiligo was defined as vitiligo showing no further spread or spontaneous repigmentation over a 3-month period. The patients were selected from the outpatient department of our institute (Cutis Skin Institute, Srinagar, Kashmir) and the study was conducted from February 2013 to January 2014. Informed consent was obtained from every enrolled patient prior to the start of the study. Patients with photosensitive disorders, history of intake of immunosuppressant or immunomodulator drugs, and patients who had received any other form of phototherapy in the past were excluded from the study. Pregnant patients and those with segmental or acrofacial vitiligo were also excluded. All the patients had Fitzpatrick skin type 3 or 4.
The patients were divided into two groups of 30 each, based on their ability to come for twice or once weekly targeted ultraviolet B treatment. Those who were ready to come for twice-weekly treatment were included in group A, whereas those reluctant or unable to come twice a week were included in group B. Lesions present on the face, neck and trunk were selected for targeted ultraviolet B phototherapy in both these groups. Lesions on the limbs or acral areas were excluded.
All patients were treated with a targeted phototherapy device named Levia R Professional targeted ultraviolet B device (Lerner Medical Devices Inc., USA). The device uses a short arc metal halide lamp with a filter to produce narrowband ultraviolet B light (300-320 nm) with a peak at 314 nm. The output of narrowband ultraviolet B delivered by the machine is in the range of 100−120 mW/cm 2 and the individual dose that the machine can provide ranges from 5 to 800 mJ/cm 2 with possible increments of 5 mJ/cm 2. A stencil is provided with the device to treat vitiligo lesions of different shapes and sizes.
In both groups, the initial dose of targeted ultraviolet B was 200 mJ/cm 2 and the energy was increased by 50 mJ/cm 2 after every dose until a faint erythema or perifollicular pigmentation was noticed. The same dose was continued until the patient continued to show mild erythema or perifollicular pigmentation. In case of blistering or painful erythema, treatment was stopped for a week and the dose was reduced by 50 mJ/cm 2 from the last dose received. No topical or oral drugs were used in any of the groups during the study period. Targeted narrowband ultraviolet B was continued until the patients continued to show pigmentation or for a maximum of 30 sessions.
Patients in the twice weekly group received targeted ultraviolet B on the selected lesions twice a week with a gap of 2−3 days in between doses while those in the once weekly group received targeted ultraviolet B once a week, usually on a fixed day. Response to treatment was monitored clinically and photographically, which was graded as excellent (≥75% repigmentation), good (50−74% repigmentation) and poor (<50% repigmentation). Targeted ultraviolet B was discontinued if there was no evidence of repigmentation by the 12th dose.
The primary outcome measure monitored was the extent of repigmentation achieved. This was calculated separately for each body site (face, neck and trunk). This was then compared between the two groups. In addition, the number of doses needed for repigmentation to start, the cumulative dose of targeted ultraviolet B administered as well as the number of doses required to achieve complete repigmentation for each body site were also compared. Adverse events that were monitored included painful erythema, blistering, koebnerization, extension of lesions and any other adverse reaction. The chi-square test was used to assess the statistical significance of the results and a P value of < 0.05 was considered as statistically significant.
Results
The age of patients in the twice weekly group ranged from 8 to 36 years with a mean of 19.4 years, whereas in the once weekly group, it ranged from 10 to 28 years with a mean of 18.1 years. There were 11 males and 19 females in the twice weekly group, while the once weekly group had 14 males and 16 females.
The mean duration of vitiligo in the twice weekly and once weekly groups was 3.85 ± 2.58 years (range 1−12 years) and 3.3 ± 1.92 years (range 1−10 years) respectively. A total of 90 lesions were treated on the face, neck and trunk (chest or back). These included 48 lesions in the twice weekly group (24 on the face and neck, 24 on the trunk) and 42 lesions in the once weekly group (20 on the face and neck, 22 on the trunk).
Excellent results (≥75% pigmentation) were achieved in 63.3% (57/90) lesions while 24.4% (22/90) lesions exhibited a good response (50−74% pigmentation). In 11 lesions (12.2%), the response was termed as poor as the extent of pigmentation achieved was less than 50%.
On comparing the results between the two groups, 30 out of 48 lesions (62.5%) showed excellent response in the twice weekly group, while 27 out of 42 lesions (64.3%) showed similar results in the once weekly group [Table - 1].
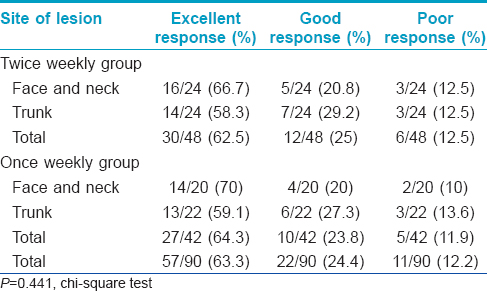
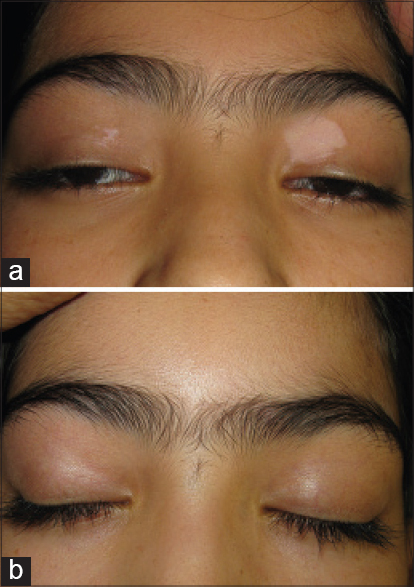
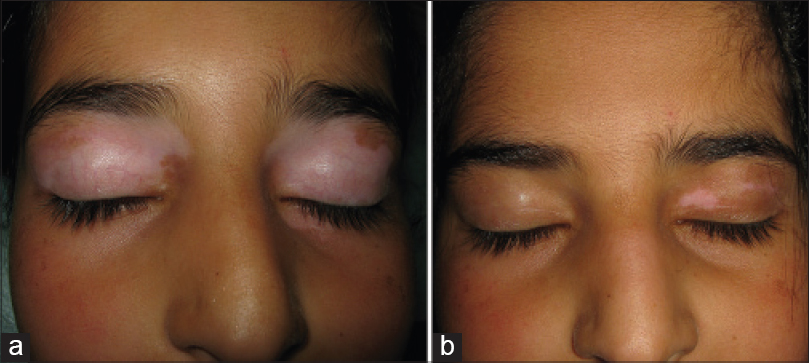
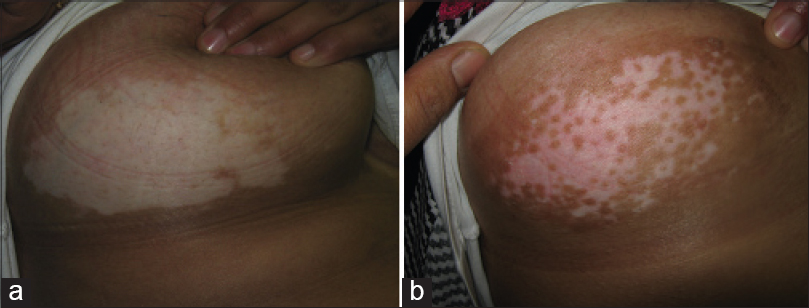
Comparing the results at individual body sites, 67% (16/24) lesions achieved excellent results on the face and neck in the twice weekly group [Figure - 1]a and [Figure - 1]b while 70% (14/20) lesions achieved a similar response in the once weekly group [Figure - 2]a and [Figure - 2]b. On the trunk, 58.3% (14/24) and 59.1% (13/22) of the lesions were able to achieve an excellent response in the twice weekly and once weekly groups respectively [Figure - 3]a and [Figure - 3]b. Good response was seen in 20.8% (5/24) lesions on the face and neck, and 29.2% (7/24) of lesions on the trunk in the twice weekly group. The corresponding figures in the once weekly group were 20% (4/20) on the face and neck, and 27.3% (6/22) on the trunk ([Figure - 4]a and [Figure - 4]b. Data was analyzed using SPSS software for Windows (IBM Corporation USA). The chi-square test was used to assess the statistical significance. No statistically significant difference was found between the repigmentation achieved by the two groups on different body sites (P = 0.441) [Table - 1].
 |
| Figure 1: (a) Vitiligo on the eyelids treated with twice weekly targeted ultraviolet B (b) Excellent response |
 |
| Figure 2: (a) Vitiligo on the eyelids treated with once weekly targeted ultraviolet B (b) about 90% repigmentation |
 |
| Figure 3: (a) Lesion on the breast in the twice weekly group patient (b) good response to targeted ultraviolet B |
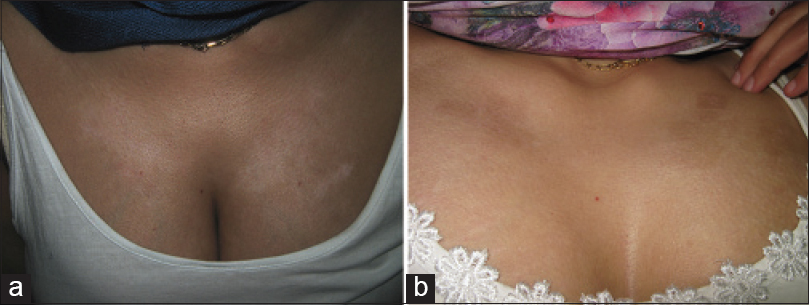 |
| Figure 4: (a) Lesions on the chest in the once weekly group patient (b) response after 16 doses of once weekly targeted ultraviolet B |
Onset of repigmentation was seen after an average of 4.69 doses (range 3−12) in the twice weekly group while it took an average of 4.35 doses (range 3−10) for repigmentation to start in the once weekly group [Table - 2]. Patients in the twice weekly group noticed the first evidence of pigmentation by the end of the 3 weeks (4.69 doses), while those in the once weekly group noticed it after about 1 month (4.35 doses). No statistically significant difference was observed between the two groups with respect to the number of doses required (chi-square test with P = 0.413).
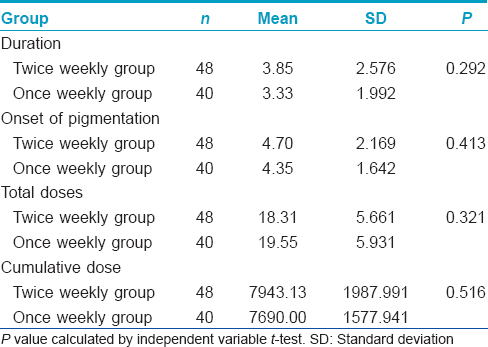
The cumulative dose of targeted ultraviolet B was also calculated in the two groups. It ranged from 3.37 to 14.06 J/cm 2 in the twice weekly group, with a mean cumulative dose of 8.26 J/cm 2. In the once weekly group, the value ranged from 5.1 to 12.05 J/cm 2 with a mean of 7.69 J/cm 2 [Table - 2]. Again, no significant difference was observed in this variable between the two groups on statistical analysis (chi-square test with P = 0.516).
Discussion
Targeted phototherapy with lasers, lamps or ultraviolet sources is becoming a popular treatment of vitiligo due to its efficacy and safety profile. Many clinical studies have demonstrated the efficacy of targeted phototherapy, including targeted ultraviolet B therapy in vitiligo.[13],[14],[15],[16],[17],[18],[19] In addition, a number of topical treatment options have been shown to have a synergistic effect with this treatment modality.[20],[21],[22] Clinical studies have demonstrated that the efficacy of targeted phototherapy including targeted ultraviolet B is site dependent in vitiligo, with the face and neck responding better than other body sites, and acral lesions responding the least favourably.
In most of the clinical studies on targeted phototherapy, either twice-weekly or thrice-weekly treatment regimens have been used. A twice-weekly treatment schedule has been most commonly followed, whether it is excimer laser, targeted broadband ultraviolet B or narrowband ultraviolet B.,[13],[14],[15],[16],[17],[18] There are only a few clinical studies which have employed a different dosage schedule or compared different dosage frequencies with targeted phototherapy devices in vitiligo.
A study by Hofer et al. in 2005 commented on the efficacy of different dosage schedules of targeted phototherapy with excimer laser in vitiligo. They found almost similar results with once weekly, twice weekly and thrice weekly light exposures. They observed that repigmentation started earlier in patients who were treated with twice or thrice weekly excimer laser treatment, compared to those who received treatment once weekly. The ultimate extent of repigmentation was almost similar in all the groups. They concluded that the ultimate repigmentation achieved seemed to depend entirely on the total number of treatments, and not their frequency.[23]
Another related study by Shen et al. from China reported similar observations with four different dosage schedules of excimer laser treatment. The patients in this study were treated with excimer laser on face and neck vitiligo at 0.5, 1, 2 and 3 exposures per week.[24] The final repigmentation achieved was almost similar in patients treated with 1, 2 or 3 exposures every week while those receiving 0.5 doses (one dose every two weeks) could not achieve the same level of repigmentation. Repigmentation occurred fastest with twice and thrice weekly exposures but the final repigmentation achieved was the same as that with once weekly treatment.[24]
We are not aware of any such comparison studies between different dosage frequencies by targeted ultraviolet B devices. However, there is a clinical study that has reported a successful outcome in vitiligo with a targeted ultraviolet B device, where treatment was delivered once every two weeks. This study reported >75% repigmentation in 69.5% of 734 patients treated over 12 months. Of the 734 patients treated, 112 (15.3%) patients achieved complete repigmentation of the treated lesions.[19] The device used in this study (Bioskin) provides targeted narrowband ultraviolet B with the emission spectrum of 300−320 nm peaking at 311 nm.
Practically, whenever targeted phototherapy is considered in any patient suffering from vitiligo, the most important factor that affects this choice is the ability of the patient to comply with a twice or thrice weekly treatment schedule. If given a choice, most patients would favour an option that interferes the least with their daily life. Visiting a phototherapy clinic twice or thrice a week for months together is a difficult proposition for most patients. This is the primary reason for the limited use of targeted phototherapy in vitiligo. Most of the patients are not able to get the benefit of this rapidly acting therapeutic modality.
We studied vitiligo lesions on the face, neck and trunk as these are the sites where targeted ultraviolet B is most effective. Acral lesions and segmental vitiligo were excluded as they are considered to be relatively resistant to this treatment. We were able to achieve excellent results in 63.3% of the treated lesions, which is a figure consistent with almost all studies conducted on targeted ultraviolet B in vitiligo. Lesions on the face and neck responded better with 68.8% lesions showing excellent results collectively in both the twice weekly and once weekly treatment groups.
More significantly, on comparing the results between twice weekly and once weekly regimens, the extent of repigmentation achieved on each individual site was similar in both groups. We compared the extent of repigmentation between the groups separately for different body sites, as the efficacy of targeted ultraviolet B is site dependent, and no statistically significant difference was observed in this primary outcome measure. The secondary outcome measures were the cumulative dose of targeted ultraviolet B and the number of doses needed for the initiation of repigmentation. The cumulative dose of targeted ultraviolet B did not differ statistically between both groups. This means that patients do not require higher cumulative doses when the frequency of targeted ultraviolet B is decreased to once a week. It also provides indirect evidence that the efficacy of targeted ultraviolet B remains the same with once weekly and twice weekly treatment regimens.
The average number of doses received until the onset of repigmentation also did not differ significantly between both groups. Thus, the patients receiving targeted ultraviolet B once a week are expected to take a little longer to see the first evidence of repigmentation, compared to those receiving twice weekly exposures. However, by the time the repigmentation is first noticed, both groups are expected to have received the same number of doses.
We feel that compliance to treatment can be greatly improved if a once weekly treatment schedule is followed in targeted ultraviolet B therapy. The results show that therapeutic efficacy is not compromised. If the choice of once weekly treatment schedule is offered to vitiligo patients, it is likely many more would be willing to opt for targeted phototherapy, including targeted ultraviolet B therapy.
Limitations
The sample size for this comparison study is small and the two population groups are not randomized. Randomized controlled trials on larger population groups are needed to confirm the study results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ongenae K, Beelaert L, van Geel N, Naeyaert JM. Psychosocial effects of vitiligo. J Eur Acad Dermatol Venereol 2006;20:1-8.
[Google Scholar]
|
| 2. |
Kent G, al-Abadie M. Factors affecting responses on Dermatology Life Quality Index items among vitiligo sufferers. Clin Exp Dermatol 1996;21:330-3.
[Google Scholar]
|
| 3. |
Scherschun L, Kim JJ, Lim HW. Narrow-band ultraviolet B is a useful and well-tolerated treatment for vitiligo. J Am Acad Dermatol 2001;44:999-1003.
[Google Scholar]
|
| 4. |
Pacifico A, Leone G. Photo (chemo) therapy for vitiligo. Photodermatol Photoimmunol Photomed 2011;27:261-77.
[Google Scholar]
|
| 5. |
Hamzavi IH, Lim HW, Syed ZU. Ultraviolet-based therapy for vitiligo: What's new? Indian J Dermatol Venereol Leprol 2012;78:42-8.
[Google Scholar]
|
| 6. |
Goktas EO, Aydin F, Senturk N, Canturk MT, Turanli AY. Combination of narrow band UVB and topical calcipotriol for the treatment of vitiligo. J Eur Acad Dermatol Venereol 2006;20:553-7.
[Google Scholar]
|
| 7. |
Majid I. Does topical tacrolimus ointment enhance the efficacy of narrowband ultraviolet B therapy in vitiligo? A left-right comparison study. Photodermatol Photoimmunol Photomed 2010;26:230-4.
[Google Scholar]
|
| 8. |
Esfandiarpour I, Ekhlasi A, Farajzadeh S, Shamsadini S. The efficacy of pimecrolimus 1% cream plus narrow-band ultraviolet B in the treatment of vitiligo: A double-blind, placebo-controlled clinical trial. J Dermatolog Treat 2009;20:14-8.
[Google Scholar]
|
| 9. |
Grimes PE. Advances in the treatment of vitiligo: Targeted phototherapy. Cosm Dermatol 2003;16:18-22.
[Google Scholar]
|
| 10. |
Mysore V. Targeted phototherapy. Indian J Dermatol Venereol Leprol 2009;75:119-25.
[Google Scholar]
|
| 11. |
Park KK, Liao W, Murase JE. A review of monochromatic excimer light in vitiligo. Br J Dermatol 2012;167:468-78.
[Google Scholar]
|
| 12. |
Welsh O, Herz-Ruelas ME, Gómez M, Ocampo-Candiani J. Therapeutic evaluation of UVB-targeted phototherapy in vitiligo that affects less than 10% of the body surface area. Int J Dermatol 2009;48:529-34.
[Google Scholar]
|
| 13. |
Akar A, Tunca M, Koc E, Kurumlu Z. Broadband targeted UVB phototherapy for localized vitiligo: A retrospective study. Photodermatol Photoimmunol Photomed 2009;25:161-3.
[Google Scholar]
|
| 14. |
Park KK, Liao W, Murase JE. A review of monochromatic excimer light in vitiligo. Br J Dermatol 2012;167:468-78.
[Google Scholar]
|
| 15. |
Le Duff F, Fontas E, Giacchero D, Sillard L, Lacour JP, Ortonne JP, et al.308-nm excimer lamp vs 308-nm excimer laser for treating vitiligo: A randomized study. Br J Dermatol 2010;163:188-92.
[Google Scholar]
|
| 16. |
Asawanonda P, Charoenlap M, Korkij W. Treatment of localized vitiligo with targeted broadband UVB phototherapy: A pilot study. Photodermatol Photoimmunol Photomed 2006;22:133-6.
[Google Scholar]
|
| 17. |
Asawanonda P, Kijluakiat J, Korkij W, Sindhupak W. Targeted broadband ultraviolet B phototherapy produces similar responses to targeted narrowband ultraviolet B phototherapy for vitiligo: A randomized, double-blind study. Acta Derm Venereol 2008;88:376-81.
[Google Scholar]
|
| 18. |
Majid I. Efficacy of targeted narrowband ultraviolet B therapy in vitiligo. Indian J Dermatol 2014;59:485-9.
[Google Scholar]
|
| 19. |
Menchini G, Tsoureli-Nikita E, Hercogova J. Narrow-band UV-B micro-phototherapy: A new treatment for vitiligo. J Eur Acad Dermatol Venereol 2003;17:171-7.
[Google Scholar]
|
| 20. |
Passeron T, Ostovari N, Zakaria W, Fontas E, Larrouy JC, Lacour JP, et al. Topical tacrolimus and the 308-nm excimer laser: A synergistic combination for the treatment of vitiligo. Arch Dermatol 2004;140:1065-9.
[Google Scholar]
|
| 21. |
Lu-yan T, Wen-wen F, Lei-hong X, Yi J, Zhi-zhong Z. Topical tacalcitol and 308-nm monochromatic excimer light: A synergistic combination for the treatment of vitiligo. Photodermatol Photoimmunol Photomed 2006;22:310-4.
[Google Scholar]
|
| 22. |
Saraceno R, Nisticò SP, Capriotti E, Chimenti S. Monochromatic excimer light 308 nm in monotherapy and combined with topical khellin 4% in the treatment of vitiligo: A controlled study. Dermatol Ther 2009;22:391-4.
[Google Scholar]
|
| 23. |
Hofer A, Hassan AS, Legat FJ, Kerl H, Wolf P. Optimal weekly frequency of 308-nm excimer laser treatment in vitiligo patients. Br J Dermatol 2005;152:981-5.
[Google Scholar]
|
| 24. |
Shen Z, Gao TW, Chen L, Yang L, Wang YC, Sun LC, et al. Optimal frequency of treatment with the 308-nm excimer laser for vitiligo on the face and neck. Photomed Laser Surg 2007;25:418-27.
[Google Scholar]
|
Fulltext Views
7,881
PDF downloads
2,036





