Translate this page into:
The efficacy of measles–mumps–rubella vaccine versus salicylic acid–lactic paint in the treatment of warts
Correspondence Address:
Shruti S Patil
Department of Dermatology, Venereology and Leprology, MGM Medical College and Hospital, Aurangabad, Maharashtra
India
| How to cite this article: Deshmukh AR, Nawale SS, Patil SS, Pawar SS. The efficacy of measles–mumps–rubella vaccine versus salicylic acid–lactic paint in the treatment of warts. Indian J Dermatol Venereol Leprol 2020;86:753 |
Sir,
A prospective study was conducted in the dermatology outpatient department of MGM Medical College and Hospital, Aurangabad, from November 2015 to April 2018. A total of 60 patients who were clinically diagnosed with cutaneous warts were included in the study. Pregnant or lactating women, immunocompromised patients or those receiving corticosteroids, patients within 3 months prior/post-vaccination, history of allergy to measles–mumps–rubella (MMR) vaccine or hypersensitivity to egg protein or to any ingredient of SAL paint or neomycin (because the vaccine may contain traces of neomycin), patients with meningitis, impairment of central nervous system, genital and perianal warts/facial warts, ulcerated or inflamed warts, leukemia, and other malignant diseases were excluded from the study.
The details of the study were clearly explained to the patients. Written informed consent was obtained. Detailed demographic data of each patient with clinical examination findings and digital photographs were recorded.
The patients were randomly divided into two groups with the help of random number table- Group A and B, each containing 30 patients each. Group A patients were given 0.3 mL of MMR vaccine intralesionally in the largest wart. Four injections were given every 2 weeks. Patients were followed up every 2 weeks and the last follow-up visit was scheduled 2 months after the last injection. Lesion count and reduction in the size of lesions were noted at each visit. The lesions were graded by percentage reduction in size of the largest lesion and also reduction in the lesion count. Group B patients were given SAL paint (composition: salicylic acid 16.7% and lactic acid 16.7% in flexible collodion base) for local application on the warts. Before application of SAL paint, lesions were pared down and/or soaked in warm water for at least 5 min. SAL paint was then applied to the warts twice a week for a maximum period of 2 months and stopped earlier if the lesions disappeared. Overall, the patients were called for four follow-up visits, first three visits 2 weeks apart and the last follow-up visit was scheduled 2 months after the third follow-up visit.
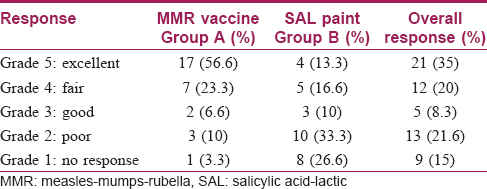
The response to treatment was evaluated as follows: Grade 1: no response, Grade 2: 1%–25% reduction in size – poor response, Grade 3: 26%–50% reduction in size – good response, Grade 4: 51%–75% reduction in size – fair response, and Grade 5: complete disappearance of lesion – excellent response. Size of the lesion was assessed by measuring tape.
Adverse effects of MMR vaccine were evaluated after each treatment session. The collected data was compiled in Microsoft Excel and analyzed using specific statistical tools such as Fisher's exact test, Chi-square with Yates' correction.
Verruca vulgaris or common warts are benign verrucous proliferative lesions of skin resulting from infection by human papilloma virus. Papilloma viruses are ubiquitous, epitheliotropic, non-enveloped, small, double-stranded DNA viruses.[1] Warts are commonly seen in school-going children and adolescents. Warts spread by direct and indirect contact and can occur almost on every part of the body.[2]
There are various modalities of treatment available which include either topical agents like salicylic acid, 5-flurouracil, podophyllotoxin or photodynamic therapy or surgical methods such as cryotherapy, laser ablation, electrosurgery, and so on. Immunotherapeutic agents include intralesional interferons, imiquimod, levamisole and zinc sulfate.[3] The use of immunotherapy in treatment of warts is mediated through activation of cell-mediated immunity. It has been shown that intralesional MMR vaccine results in regression of warts via immunomodulation and induction of the immune system.[4] Salicylic acid formulations are the most common preparations used in the treatment of warts. It is thought to work by exfoliation of epidermal cells (keratolytic action) and at high concentration, can be irritant. The most commonly used over-the-counter product is salicylic acid paint. This contains salicylic acid at concentrations of 16.7% in a collodion base and they are often mixed with lactic acid in a concentration of 16.7%. It still remains the treatment of choice for common warts of hands and feet.[5] Because of the high prevalence of warts and the necessity for treatment, we evaluated efficacy of MMR vaccine injection versus topical salicylic acid in treatment of warts. Treating wart is a therapeutic challenge for both patients and physicians as recurrence is a common phenomenon. No specific treatment is completely suitable for all patients.
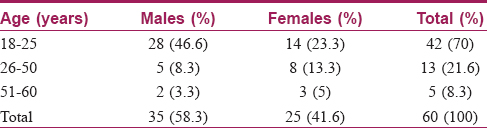
In this study, most of the patients belonged to the age group of 18–25 years, of which 28 (46.6%) were males and 14 (23.3%) were females [Table - 1]. Males were more affected than females, probably due to outdoor working conditions. Palms, soles, and lower limb involvement were commonly seen in this study. The results showed that sex ratio and age of the patients were nearly similar and there was no significant difference in the two groups.
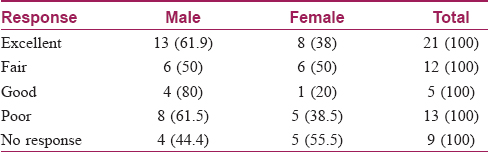
[Table - 2] shows that out of the total 60 patients, 21 (35%) patients showed excellent response, that is Grade 5 [17 (56.6%) were due to MMR vaccine and 4 (13.3%) were due to SAL paint], which indicates that there is a significant difference in both the groups (P = 0.001) [Figure - 1] and [Figure - 2]. [Table - 3] shows that out of the 21 patients who showed excellent clearance of warts (comprising both due to MMR vaccine and SAL paint), 13 (61.9%) patients were males and 8 (38%) patients were females. This table indicates no statistically significant difference (P = 0.7).
 |
| Figure 1: Therapeutic effect of intralesional MMR vaccine – before and after |
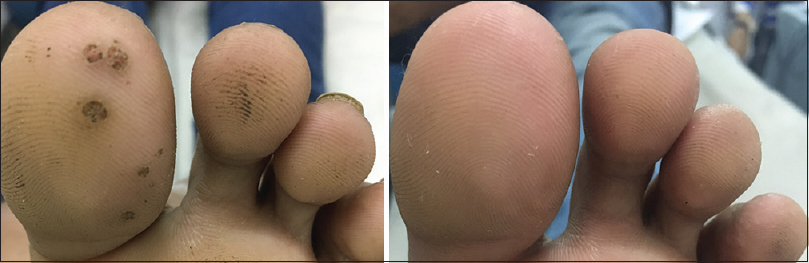 |
| Figure 2: Therapeutic effect of intralesional MMR vaccine – before and after |
Hence, a better therapeutic response was noted in patients receiving MMR vaccine rather than SAL paint. The findings of this study also showed that there was relapse seen in patients applying SAL paint. No important adverse effects were reported in any of the patients in both therapeutic groups, except pain at the time of injections. Warts with shorter duration (<6 months) responded better when compared with the ones present for a longer duration (>6 months).
In another study, Gamil et al. reported 87% complete cure, 4.3% relative cure, and 8.7% no cure with MMR vaccine. The authors of this study concluded that MMR vaccine may have desirable therapeutic effect on the treatment of wart, and similar results were also observed in our study.[3] Saini et al. reported 46.5% complete clearance in 40 of 86 patients and the patients with shorter duration of disease responded better which are comparable to our study.[6]
Intralesional immunotherapy is usually associated with mild insignificant side effects such as flu-like symptoms, edema, erythema, itching, and pain at the site of injection.[7] In case of intralesional MMR vaccine, pain at the site of injection was the main side effect observed. No swelling, redness, and itching at the site of injection was observed in the present study.[8]
Intralesional MMR vaccine has shown noteworthy advantage over topical SAL paint. Patients are advised to apply SAL paint by themselves, which might be responsible for its reported reduced efficacy and the cellular immunity is not activated which is responsible for the recurrence. Intralesional immunotherapy with MMR vaccine leads to clearance of distant noninjected warts too with no recurrence or adverse side effects.
We acknowledge the limitations of our study; it was an open-labelled study. However, intralesional MMR vaccine as an immunotherapy is an emerging modality of treatment for multiple warts with less recurrence rates with the additional advantage of clearance of warts at distant sites as well.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
IARC Working Group on the Evaluation of Carcinogenic Risk to Humans. Human Papillomaviruses. Lyon (FR): International Agency for Research on Cancer; 2007. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 90.) 1, Human Papillomavirus (HPV) Infection. Available from: https://www.ncbi.nlm.nih.gov/books/NBK321770.
[Google Scholar]
|
| 2. |
Al Aboud AM, Nigam PK. Wart (Plantar, Verruca Vulgaris, Verrucae) [Updated 2019 Sep 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431047.
[Google Scholar]
|
| 3. |
Lipke MM. An armamentarium of wart treatments. Clin Med Res 2006;4:273-93.
[Google Scholar]
|
| 4. |
Gamil H, Elgharib I, Nofal A, Abd-Elaziz T. Intralesional immunotherapy of plantar warts: Report of a new antigen combination. J Am Acad Dermatol 2010;63:40-3.
[Google Scholar]
|
| 5. |
Blank H, Rake G. Viral and Rickettsial Diseases of Skin, Eye and Mucous Membranes of Man. 4th ed. London: Churchill Livingstone; 1955. p. 121-7.
[Google Scholar]
|
| 6. |
Saini P, Mittal A, Gupta LK, Khare AK, Mehta S. Intralesional mumps, measles and rubella vaccine in the treatment of cutaneous warts. Indian J Dermatol Venereol Leprol 2016;82:343-5.
[Google Scholar]
|
| 7. |
Lichon V, Khachemoune A. Plantar warts: A focus on treatment modalities. Dermatol Nurs 2007;19:372-5.
[Google Scholar]
|
| 8. |
Horn TD, Johnson SM, Helm RM, Roberson PK. Intralesional immunotherapy of warts with mumps, Candida, and trichophyton skin test antigens: A single-blinded, randomized, and controlled trial. Arch Dermatol 2005;141:589-94.
[Google Scholar]
|
Fulltext Views
4,376
PDF downloads
2,203





