Translate this page into:
The histopathological and dermoscopic correlation of primary cutaneous mucinous carcinoma
2 Department of Dermatology, Chang Gung Memorial Hospital, Chang Gung University College of Medicine; Department of Cosmetic Science, Chang Gung University of Science and Technology, Taoyuan, Taiwan
3 Department of Pathology, Chang Gung Memorial Hospital, Taipei, Taiwan
Correspondence Address:
Sindy Hu
Chang Gung Memorial Hospital, 199, Tun-Hwa North Road, Taipei 105
Taiwan
| How to cite this article: Cheng CY, Huang YL, Kuo TT, Hu S. The histopathological and dermoscopic correlation of primary cutaneous mucinous carcinoma. Indian J Dermatol Venereol Leprol 2019;85:215-220 |
Sir,
Primary cutaneous mucinous carcinoma is a rare neoplasm of the skin, which was first described by Lennox et al. in 1952.[1] The clinical presentation of primary cutaneous mucinous carcinoma is a solitary, asymptomatic reddish or gray-blue nodule, which is often located on the face and scalp. In the present study, we enrolled four cases diagnosed as primary cutaneous mucinous carcinoma with dermoscopic examination in Chang Gung Memorial Hospital, Taoyuan, Taiwan from 2013 to 2018.
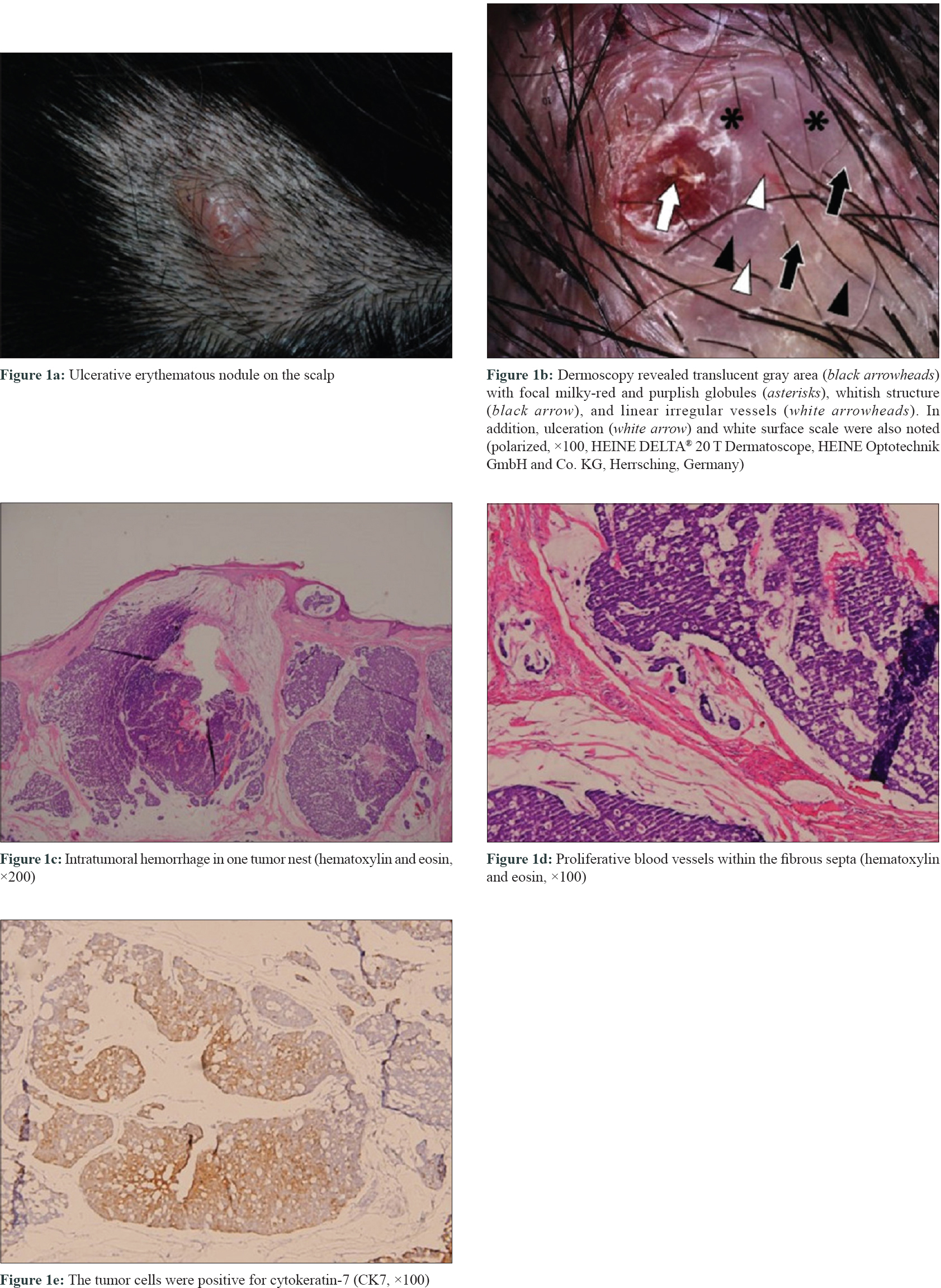
Case 1
A 49-year-old woman presented with a 6-month history of a single, slowly enlarging, tender, ulcerative, erythematous tumor on her scalp [Figure - 1]a. Dermoscopic examination showed a translucent gray area with scattered milky-red and purplish globules separated by whitish structures. Linear irregular vessels were also noted in the whitish structures [Figure - 1]b. Histopathological examination revealed a tumor nodule occupying the dermis and subcutis, which contained lobules of tumor nests in mucinous pools. Intratumoral hemorrhage in some tumor lobules and proliferative blood vessels within the fibrous septa were also present [Figure - 1]c and [Figure - 1]d. Immunohistochemistry was done as demonstrated in in [Figure - 1]e.
 |
| Figure 1: |
Case 2
A 64-year-old woman had one non-tender, slowly growing, erythematous nodule on her left lower eyelid for 2 years [Figure - 2]a. Dermoscopy revealed translucent gray globules encircled with grayish-white areas in an arch-like pattern and linear irregular vessels located peripherally. In addition, focal brownish area was also noted [Figure - 2]b. Microscopic findings showed a nodule of cribriform glands with focal mucin production and blood vessels growing in fibrous septa [Figure - 2]c. Perivascular hemosiderin deposition was present in the upper dermis [Figure - 2]d. Immunohistochemistry done is shown in [Figure - 2]e, [Figure - 2]f, [Figure - 2]g.
 |
| Figure 2: |
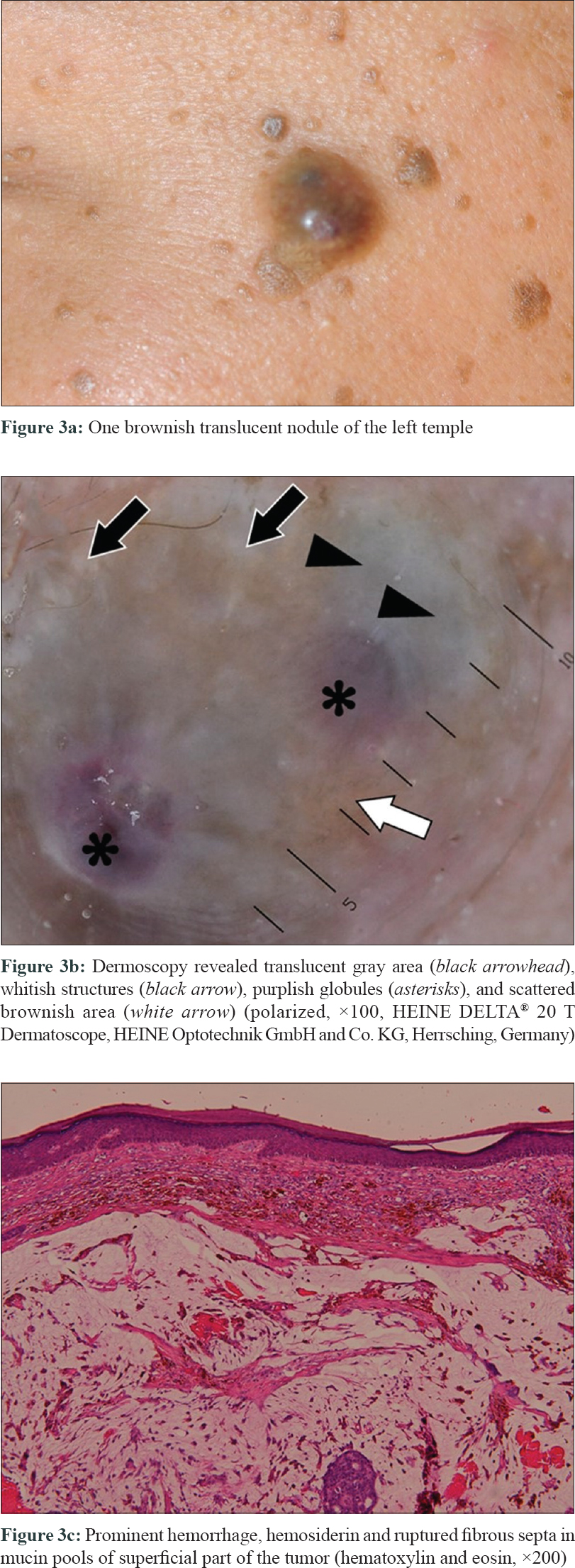
Case 3
A 49-year-old man presented with a slowly growing, nontender, brownish translucent nodule on his left temple for 2 to 3 years [Figure - 3]a. Dermoscopic examination showed multiple translucent gray area, clusters of whitish cloud-like structure, purplish globules, as well as scattered brownish areas [Figure - 3]b. Histopathology showed a dermal nodule composed of cribriform epithelial cells in mucin lakes. Massive intratumoral hemorrhage with hemosiderin deposition in the superficial part of the tumor was noted. Some of fibrous septa were ruptured and the debris floated in mucin pools [Figure - 3]c.
 |
| Figure 3: |
Case 4
A 48-year-old man had one slowly growing, nontender, translucent erythematous nodule on his left cheek for 5 years [Figure - 4]a. Dermoscopy showed multiple translucent gray area and pinkish globules separated by whitish halo-like structures, focal purplish globules, as well as short, linear, irregular and dotted vessels [Figure - 4]b. Histopathology revealed a dermal nodule composed of tumor nests with glandular lumina in pools of mucin separated by fibrous strands. Proliferative dilated blood vessels surrounding the tumor and intratumoral hemorrhage in some tumor nests were also shown microscopically [Figure - 4]c. Immunohistochemistry was demonstrated in [Figure - 4]d.
 |
| Figure 4: |
The characteristics and correlation of dermoscopic and histopathological findings are summarized in [Table - 1] and [Table - 2]. All the patients had undergone computed tomography and/or positron emission tomography, and metastasis from other organs was excluded. In our series, case 3 underwent Mohs micrographic surgery whilst others received wide local surgical excision. No recurrence was observed during the follow-up for at least 6 months.


Primary cutaneous mucinous carcinoma is a rare, slow-growing tumor with indolent clinical course.[2] The characteristic pathological changes are tumors with pools of mucin divided by thin fibrous septa. The neoplastic epithelial cells in mucin lakes resemble “floating islands.” The diagnosis of primary cutaneous mucinous carcinoma should be differentiated from metastasis of mucinous adenocarcinoma from other organs because microscopic findings of both are often indistinguishable.[3]
In the present case series, we found that the consistent dermoscopic findings of primary cutaneous mucinous carcinoma were translucent gray globules or area as well as whitish structures. The translucent gray globules were correlated with the tumor nests in mucin pools. The whitish structure was associated with the fibrous septa within the tumor or the fibrous capsule surrounding the tumor. It was mainly a halo-like structure since the fibrous septa were intact in most cases. In case 3, the floating fibrous debris in mucin pools caused cloud-like appearance of whitish structure.
In addition, we found that the main dermoscopic vascular morphology of primary cutaneous mucinous carcinoma was linear irregular pattern which has not been earlier described.[4],[5] The vascular pattern was correlated with the vessels growing in fibrous septa or capsules. Besides, dotted vascular pattern was also noted in case 4, which may be associated with the focal vertical growth of blood vessels surrounding the tumor. The purplish globules and brownish areas in dermoscopic examination may be associated with the intratumoral hemorrhage and hemosiderin deposition, respectively. The secondary pathological changes of the primary tumor may cause diverse dermoscopic manifestations.
The present case series demonstrated that translucent gray globules or area, linear irregular vascular pattern, as well as whitish structure were the characteristic dermoscopic findings of primary cutaneous mucinous carcinoma. Dermoscopy may be a useful tool to help the physician diagnose this rare entity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Lennox B, Pearse AG, Richards HG. Mucin-secreting tumours of the skin with special reference to the so-called mixed-salivary tumour of the skin and its relation to hidradenoma. J Pathol Bacteriol 1952;64:865-80.
[Google Scholar]
|
| 2. |
Adefusika JA, Pimentel JD, Chavan RN, Brewer JD. Primary mucinous carcinoma of the skin: The Mayo clinic experience over the past 2 decades. Dermatol Surg 2015;41:201-8.
[Google Scholar]
|
| 3. |
Kamalpour L, Brindise RT, Nodzenski M, Bach DQ, Veledar E, Alam M. Primary cutaneous mucinous carcinoma: A systematic review and meta-analysis of outcomes after surgery. JAMA Dermatol 2014;150:380-4.
[Google Scholar]
|
| 4. |
Togawa Y. Review of vasculature visualized on dermoscopy. J Dermatol 2017;44:525-32.
[Google Scholar]
|
| 5. |
Ayhan E, Ucmak D, Akkurt Z. Vascular structures in dermoscopy. An Bras Dermatol 2015;90:545-53.
[Google Scholar]
|
Fulltext Views
3,909
PDF downloads
2,474





