Translate this page into:
The "sign of groove", a new cutaneous sign of internal malignancy
2 Department of Pathology, Medical College Hospital, Trivandrum, Kerala, India
Correspondence Address:
Pradeep S Nair
Kamala Sadan, Thampuran Mukku, Kunnukuzhi, Trivandrum - 695 037, Kerala
India
| How to cite this article: Nair PS, Nanda Kumar G, Jayapalan S. The "sign of groove", a new cutaneous sign of internal malignancy. Indian J Dermatol Venereol Leprol 2007;73:141 |
Abstract
A 36-year-old young male with multiple heterosexual contacts presented with bilateral inguinal bubo and the classical "sign of groove". A diagnosis of lymphogranuloma venereum (LGV) was made and a three-week course of doxycycline was given. Lack of response prompted us to investigate further. A biopsy of the bubo was consistent with non-Hodgkin's lymphoma (NHL). Immunohistochemistry of the lymph node done at the Regional Cancer Center (RCC), Trivandrum, confirmed the diagnosis as NHL of diffuse large B-cell type. The second patient, a 32-year-old male with two unprotected heterosexual contacts presented with a left-sided inguinal bubo of six weeks duration. An empirical course of doxycycline was given even though investigations did not reveal any STI. Lack of response prompted us to do a lymph node biopsy, which was consistent with NHL, which later with immunohistochemistry was confirmed as NHL, diffuse large cell type. We are reporting here that the "sign of groove" is not specific for LGV as thought earlier, but can occur in NHL also. |
| Unilateral bubo with �sign of groove� in case 2 |
 |
| Unilateral bubo with �sign of groove� in case 2 |
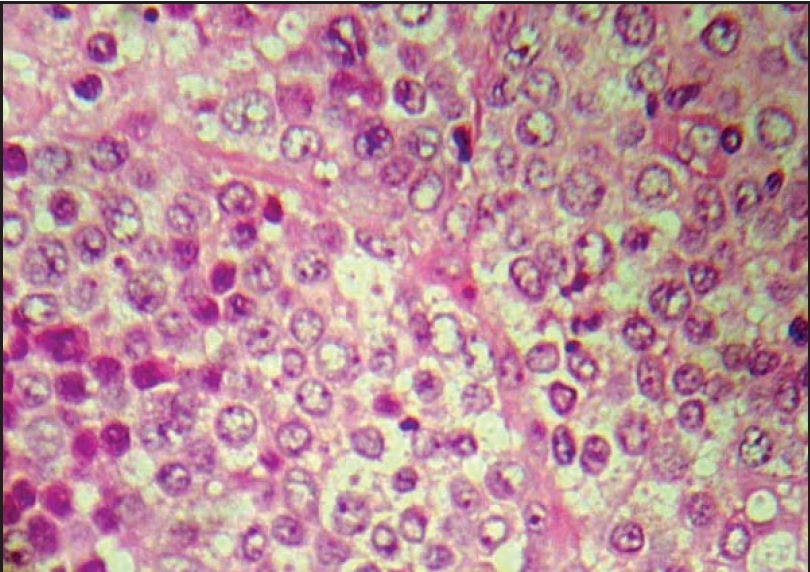 |
| Lymph node biopsy showing large mononuclear cells with vesicular nuclei and nucleoli suggestive of NHL, (H and E x1000) |
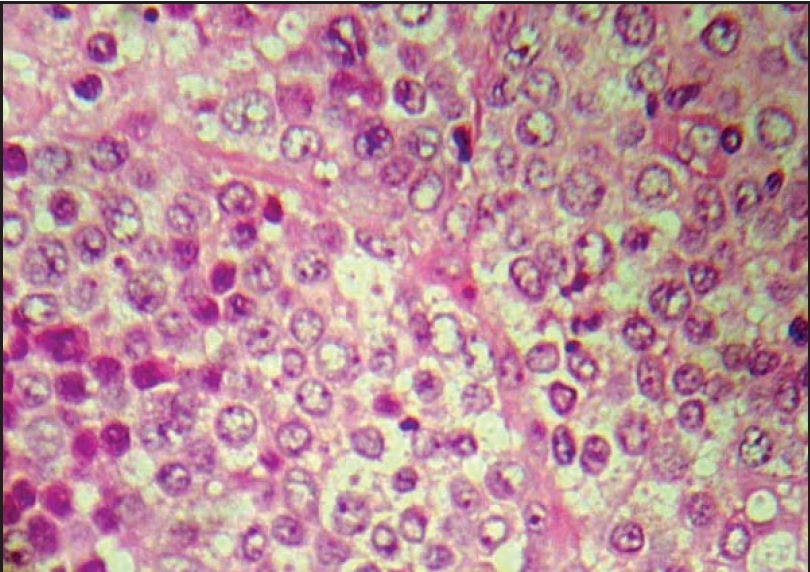 |
| Lymph node biopsy showing large mononuclear cells with vesicular nuclei and nucleoli suggestive of NHL, (H and E x1000) |
 |
| Bilateral inguinal bubo with �sign of groove� in case 1 |
 |
| Bilateral inguinal bubo with �sign of groove� in case 1 |
INTRODUCTION
Internal malignancy, whether organ-specific or hematological can present with a plethora of cutaneous manifestations. The skin lesions can occur as secondaries or as paraneoplastic syndromes or as part of certain genetic syndromes. Metastasis to the skin usually occurs by hematogenous spread, extension through skin lymphatics or by direct spread as in cases of Paget′s disease and carcinoma of the breast. [1] Secondaries in the skin usually present as papules, plaques and nodules, a common site being the anterior abdominal wall. Carcinoma of the breast, lungs, ovaries and GIT are common to cause cutaneous metastasis. [1] Paraneoplastic syndromes have a wide clinical spectrum and it is due to certain cytokines like transforming growth factor alpha (TGF-a) or peptides released by the malignant cells. [2],[3] Here we are presenting two cases with a new sign of internal malignancy hitherto not reported elsewhere.
CASE REPORT
Case 1
A 36-year-old unmarried male presented to our department with bilateral inguinal swellings of three months duration. The patient gave history of multiple unprotected heterosexual contacts with known partners and CSW′s. There was no history of any genital ulceration, papule, vesicle or discharge prior to the onset of the inguinal swelling. The swelling first appeared as a raised nontender erythematous plaque on the left and then on the right inguinal region. Within a course of two to three months the swelling increased in size, but there was no history of rupture of the lesions or ulceration. There were no constitutional symptoms. The patient did not give history of intravenous drug abuse or blood transfusion. On examination there were bilateral well-defined sausage-shaped buboes both above and below the inguinal ligament, with a prominent "sign of groove" [Figure - 1]. The skin over the bubo showed slight erythema, but no tenderness. On palpation a well-defined, nontender, firm and multi-locular bubo was seen above and below the inguinal ligament on both sides. The skin over the bubo could not be pinched. No other skin or mucosal lesions or lymphadenopathy was observed elsewhere.
The patient′s hemogram, urine examination, liver and renal function tests were normal. Chest X-ray was normal. Mantoux test was negative and sputum for AFB was negative. Blood VDRL, TPHA and ELISA for HIV 1 and 2 were negative. Fluid obtained by aspiration of the bubo did not show any organism by gram stain and a culture was sterile. An empirical diagnosis of lymphogranuloma venereum (LGV) was made because of the presence of the classical sign of groove and the high-risk behavior of the patient. The patient was given three-week course of 100 mg of doxycycline twice a day.
After three weeks of therapy, no response was noted. In addition to this, buboes increased in size. In view of non-response, patient was reinvestigated. Repeat hemogram showed anemia of 9 gm%. Peripheral smear showed microcytic hypochromic anemia, but no abnormal cells. An Ultrasound abdomen showed inguinal lymphadenopathy, but no hepatosplenomegaly. A whole body CT-Scan showed inguinal lymphadenopathy, but no involvement of any other organ. FNAC from the inguinal lymph nodes showed a few abnormal and atypical cells. Bone marrow examination was normal. A lymph node biopsy from the inguinal region showed loss of architecture with presence of large number of atypical mononuclear cells with vesicular nuclei and nucleoli, consistent with non-Hodgkin′s lymphoma [Figure - 2]. Immunohistochemistry of the lymph node specimen done at Regional Cancer Center (RCC), Trivandrum confirmed the diagnosis as non-Hodgkin′s lymphoma (NHL), diffuse large B-cell type (CD19 and Bcl-2 positive). We made a final diagnosis of NHL with a positive "sign of groove". The patient was referred to RCC, Trivandrum for further management.
Case 2
A 32-year-old unmarried male presented with left sided inguinal swelling of six weeks duration. He gave history of two unprotected heterosexual exposures, but no history of genital ulceration. He was given empirical treatment from his local hospital with doxycycline and later erythromycin as a part of "syndromic treatment" for bubo, but was referred to our hospital due to lack of response. On examination the patient had a left inguinal bubo with the classical "sign of groove" [Figure - 3]. The patient did not have any other skin or mucosal lesion. Serological tests and urine examination did not show evidence of any STD. FNAC of lymph node showed a few cells with hyperchromatic nuclei. Bone marrow biopsy was normal. Ultrasound scan of abdomen showed gross inguinal lymphadenopathy, but no organomegaly. An inguinal lymph node biopsy showed NHL. Immunohistochemistry done in the RCC, Trivandrum was suggestive of NHL, diffuse large B-cell type, CD19 positive and Bcl-2 positive. The patient was referred to RCC for further management.
DISCUSSION
The "sign of groove" was first described by Greenblatt in 1953 as a characteristic sign in LGV to denote the sausage shaped swellings of the inguinal lymph node above and the femoral lymph node below the inguinal ligament, the inguinal ligament forming a groove in between the swellings. [4],[5] But our case reports show that it can occur in NHL as well. The inguinal ligament is a tough fibrous structure attached medially to the pubic tubercle and laterally to the anterior superior iliac spine. This feature makes it naturally resistant to any pressure and hence forms a groove when there are swellings both above and below the inguinal ligament as seen in LGV and NHL. However a previous study done in South India on the cutaneous manifestations of NHL in 32 cases did not observe this sign. [6]
Primary cutaneous B-cell lymphoma of the skin presents with plaques, nodules and tumors on the skin, but without lymph node involvement and is very rare. The histopathology is also characteristic with a "bottom heavy" infiltrate of malignant cells. [7] We are reporting these two cases to highlight that the "sign of groove" should be considered as a sign of internal malignancy (as in our cases). Physicians/dermatologists should make themselves aware of this sign in cases of inguinal swellings.
| 1. |
Schwartz RA. Cutaneous metastatic disease. J Am Acad Dermatol 1995;33:161-82.
[Google Scholar]
|
| 2. |
Schwartz RA. Acanthosis nigricans. J Am Acad Dermatol 1994;31:1-19.
[Google Scholar]
|
| 3. |
Ellis DL, Yats RA. Sign of leser-trelat. Clin Dermatol 1993;11:141-8.
[Google Scholar]
|
| 4. |
King A, Nicol C, Rodin P. Lymphogranuloma venereum. In: Venereal diseases. King A, Nicol C, Rodin P, editors. 4th ed. English Language Book Society and Bailliere Tindall: London; 1980. p. 258-67.
[Google Scholar]
|
| 5. |
Garrido Neves, Lupi O. Lymphogranuloma venereum. In: Borchardt A, Noble MA, editors. Sexually transmitted diseases: Epidemiology, pathology, diagnosis and treatment. CRC Press: New York; 1997. p. 117-28.
[Google Scholar]
|
| 6. |
Sathish Kumar S, Maria Kuruvilla, Ganesh Pai S, Dinesh M. Cutaneous manifestations of Non-Hodgkin's lymphoma. Indian J Dermatol Venereol Leprol 2003;69:12-5.
[Google Scholar]
|
| 7. |
Bhat I, Janaki C, Sentamilselvi G, Janaki R. Primary cutaneous B cell lymphoma. Indian J Dermatol Venereol Leprol 2003;69:289-91.
[Google Scholar]
|
Fulltext Views
8,257
PDF downloads
2,035





