Translate this page into:
The utility of dermoscopy in the diagnosis of evolving lesions of vitiligo
Correspondence Address:
Sarvesh S Thatte
Department of Dermatology, Seth GS Medical College and K.E.M Hospital, Parel, Mumbai - 400 012
India
| How to cite this article: Thatte SS, Khopkar US. The utility of dermoscopy in the diagnosis of evolving lesions of vitiligo . Indian J Dermatol Venereol Leprol 2014;80:505-508 |
Abstract
Background: Early lesions of vitiligo can be confused with various other causes of hypopigmentation and depigmentation. Few workers have utilized dermoscopy for the diagnosis of evolving lesions of vitiligo. Aim: To analyze the dermoscopic findings of evolving lesions in diagnosed cases of vitiligo and to correlate them histopathologically. Methods: Dermoscopy of evolving lesions in 30 diagnosed cases of vitiligo was performed using both polarized light and ultraviolet light. Result: On polarized light examination, the pigmentary network was found to be reduced in 12 (40%) of 30 patients, absent in 9 (30%), and reversed in 6 (20%) patients; 2 patients (6.7%) showed perifollicular hyperpigmentation and 1 (3.3%) had perilesional hyperpigmentation. A diffuse white glow was demonstrable in 27 (90%) of 30 patients on ultraviolet light examination. Melanocytes were either reduced in number or absent in 12 (40%) of 30 patients on histopathology. Conclusion: Pigmentary network changes, and perifollicular and perilesional hyperpigmentation on polarized light examination, and a diffuse white glow on ultraviolet light examination were noted in evolving vitiligo lesions. Histopathological examination was comparatively less reliable. Dermoscopy appears to be better than routine histopathology in the diagnosis of evolving lesions of vitiligo and can obviate the need for a skin biopsy.INTRODUCTION
Vitiligo is an acquired, idiopathic disorder characterized by circumscribed depigmented macules and patches with or without leukotrichia. Melanocyte destruction in vitiligo is a slow process resulting in a progressive decrease in melanocyte numbers. [1] Normal skin has a typical reticulate pigmentary pattern that corresponds to the pigmentation along rete ridges with pale areas corresponding to the papillary dermis. [2] This reticulate pigmentary pattern is altered in various pigmentary disorders including vitiligo. [3] Evolving lesions of vitiligo are difficult to distinguish clinically from other causes of hypopigmentation and depigmentation. Dermoscopic examination can detect subtle changes in the pigmentary pattern which may be useful in the early diagnosis of vitiligo.
METHODS
Dermoscopic analysis of 30 established vitiligo patients who were developing new lesions was performed at the outpatient department (Department of Dermatology, Seth G.S. Medical College and K.E.M Hospital, Parel, Mumbai) after taking due permission and approval from the Institutional Ethics Committee (IEC).
Patients were selected by the convenience sampling method. After informed consent, a detailed history was taken, physical examination was performed and clinical photographs were taken using a Canon Powershot G12 camera. Newly developed lesions were selected based on patient′s history and clinical examination. Dermoscopy of the evolving lesion was performed followed by histopathological examination of the same lesion.
Dermoscopy was performed using a video dermoscope (Ultracam TLS; Dermaindia, Tamil Nadu, India) with inbuilt white light, polarized light and ultraviolet light sources. Polarized light was used to study changes in the pigmentary network while the ultraviolet source highlighted the presence of a white glow in the lesion.
The dermoscopic and histopathological data were analyzed and 95% confidence limits were calculated using the Fisher′s exact test (Clopper-Pearson method).
RESULTS
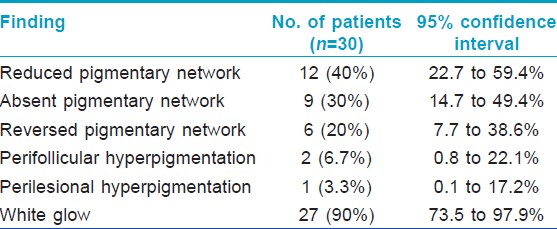
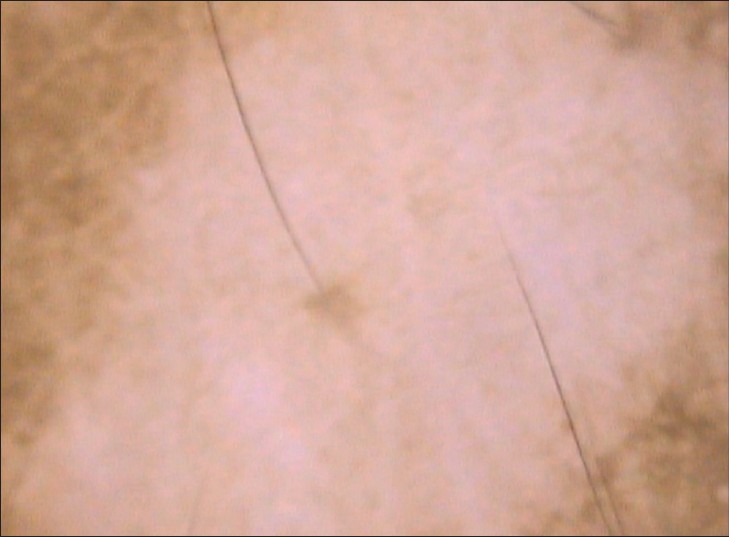
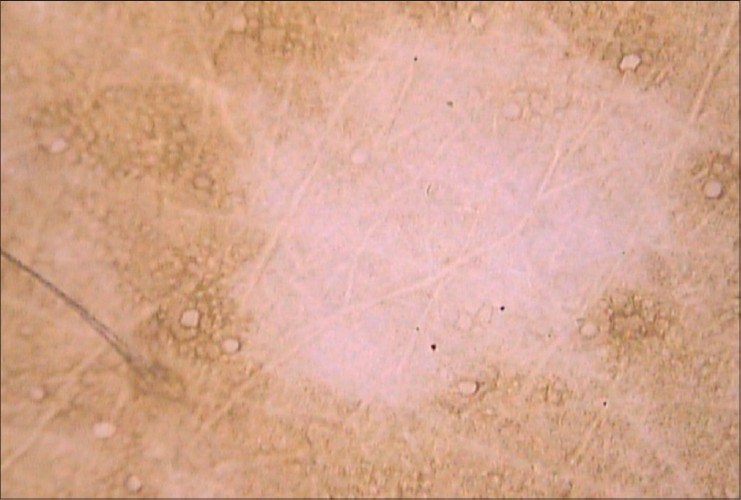
The duration of all the selected lesions was less than 1 month (range: 2-29 days, mean (SD): 15.4 days (7.9)). On polarized light examination, the pigmentary network was reduced in 12 (40%) of 30 patients [Figure - 1], absent in 9 (30%) patients [Figure - 2], and reversed in 6 (20%) patients [Figure - 3]. Perifollicular hyperpigmentation was present in 2 (6.7%) patients [Figure - 4] and perilesional hyperpigmentation was present in 1 (3.3%) patient [Figure - 5]. A diffuse white glow was seen in 27 (90%) of 30 patients on ultraviolet light examination [Figure - 6] and [Table - 1]. Dermoscopic images of normal skin are provided for comparison [Figure - 7] and [Figure - 8].
 |
| Figure 1: Reduced pigmentary network |
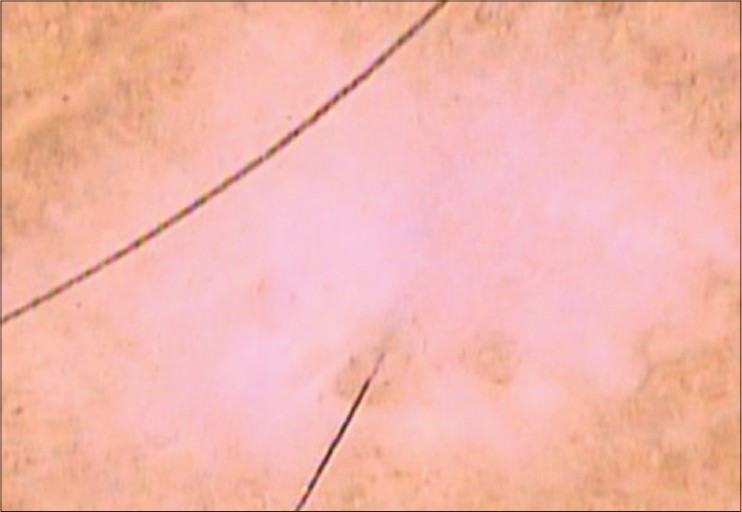 |
| Figure 2: Absent pigmentary network |
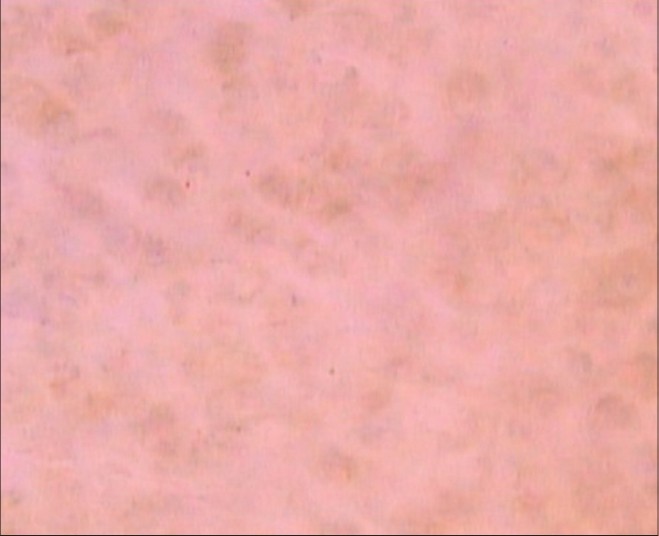 |
| Figure 3: Reversed pigmentary network |
 |
| Figure 4: Perifollicular hyperpigmentation |
 |
| Figure 5: Perilesional hyperpigmentation |
 |
| Figure 6: Diffuse white glow |
 |
| Figure 7: Normal reticulate pigmentary network (provided for comparison) |
 |
| Figure 8: Absence of white glow (provided for comparison) |
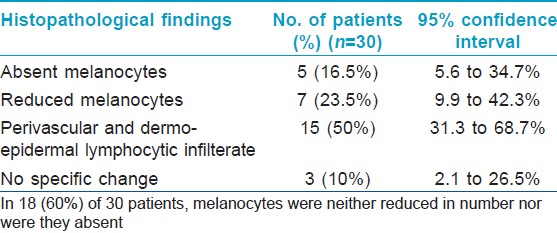
Histopathological examination was done in all patients. A biopsy was performed from the same lesion that was selected for dermoscopic examination. Among these 30 patients, melanocytes were reduced in 7 (23.5%) and absent in 5 (16.5%) patients. Perivascular and dermo-epidermal junctional lymphocytic infiltrate was noted in 15 (50%) patients. No specific changes were demonstrable on histopathological examination in 3 (10%) patients. The melanocytes were normal in number in 18 (60%) of 30 patients [Table - 2].
Confidence intervals were calculated for both dermoscopic as well as histopathological findings using the Fisher exact (Clopper-Pearson) method.
DISCUSSION
Some workers have studied the utility of dermoscopy in the diagnosis of vitiligo. Chuh and Zawar noted a pattern of depigmentation with residual reservoirs of perifollicular pigment signifying focally active or repigmenting vitiligo. [4] Meng et al., studied 176 patients with various types of depigmentation of whom 97 had vitiligo. They observed residual perifollicular pigmentation in 57 (91.9%) of 62 patients with progressing vitiligo and 22 (62.9%) of 35 those with stable vitiligo However, residual perifollicular pigmentation was absent in the 79 patients with non-vitiligo depigmentation. The presence of telangiectasia, early reservoirs of pigmentation and perilesional hyperpigmentation were related to the stage of vitiligo and treatment history of patients. [5] Their study differed from ours in that they included all types of vitiligo (evolving, stable and devolving) as well as other causes of hypopigmentation and depigmentation. Our analysis focused on identifying dermoscopic signs of evolving lesions of vitiligo.
Various dermoscopic findings are associated with stability and repigmentation of vitiligo. These include marginal and perifollicular hyperpigmentation, reticular pigmentation and marginal reticular pigmentation. [6] In our analysis, we noted reduced pigmentary network, absent pigmentary network, reversed pigmentary network, perifollicular hyperpigmentation and perilesional hyperpigmentation in the evolving vitigo lesions; a white glow was present in 27 (90%) of 30 patients. In our case series, perifollicular pigmentation was present in only 2 (6.7%) patients since repigmenting and stable vitiligo patients were excluded. [6]
A white or depigmented net-like pattern with pigmentation in between has been termed as reversed pigmentary network. This finding has not earlier been mentioned in vitiligo. However, reversed pigmentary network is a well known finding in dermoscopy of melanoma and melanocytic nevus in which it is described as reticular light areas with dark holes in the network. [7] This description was similar to our finding of reversed pigmentary network in evolving lesions of vitiligo [Figure - 3].
The loss of epidermal melanin in vitiligo lesions produces a window through which the light-induced autofluorescence of dermal collagen can be seen resulting in the bright blue-white glow. [8]
In conclusion, dermoscopy scores over routine histopathology in the diagnosis of evolving lesions of vitiligo and can obviate the need for a skin biopsy in doubtful cases.
| 1. |
Ortonne JP. Vitiligo and Other Disorders of Hypopigmentation. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. Spain: Elsevier; 2008. p. 913-4.
[Google Scholar]
|
| 2. |
Haldar SS, Nischal KC, Khopkar US. Dermoscopy: Applications and Patterns in Diseases of the Brown Skin. In: Khopkar U, editor. Dermoscopy and Trichoscopy in Diseases of the Brown Skin: Atlas and Short Text. New Delhi, India: Jaypee Brothers Medical Publishers; 2012. p. 16.
[Google Scholar]
|
| 3. |
Gutte R, Khopkar US. Dermoscopy: Differentiating evolving vitiligo from a Hypopigmented patch of Leprosy. In: Khopkar U, editor. Dermoscopy and Trichoscopy in Diseases of the Brown Skin: Atlas and Short Text. New Delhi: Jaypee Brothers Medical Publishers; 2012. p. 112-3.
[Google Scholar]
|
| 4. |
Chuh AA, Zawar V. Demonstration of residual perifollicular pigmentation in localized vitiligo-a reverse and novel application of digital epiluminescence dermoscopy. Comput Med Imaging Graph 2004;28:213-7.
[Google Scholar]
|
| 5. |
Meng R, Zhao G, Cai RK, Xiao M, Jiang Z. Application of polarized light dermoscopy in the early diagnosis of vitiligo and its differential diagnosis from other depigmented diseases. Chinese J Dermatol 2009;42:810-3.
[Google Scholar]
|
| 6. |
Chandrashekhar L. Dermoscopy: A tool to assess stability in Vitiligo. In: Khopkar U, editor. Dermoscopy and Trichoscopy in Diseases of the Brown Skin: Atlas and Short Text. New Delhi, India: Jaypee Brothers Medical Publishers; 2012. p. 112-3.
[Google Scholar]
|
| 7. |
Baªak PY, Hofmann-Wellenhof R, Massone C. Three cases of reverse pigment network on dermatoscopy with three distinctive histopathologic diagnoses. Dermatol Surg 2013;39:818-20.
[Google Scholar]
|
| 8. |
Gupta LK, Singhi MK. Resident's Page: Wood's Lamp. Indian J Dermatol Venereol Leprol 2004;70:131-5.
[Google Scholar]
|
Fulltext Views
11,038
PDF downloads
2,463





