Translate this page into:
Three cases of IL36RN-associated pustulosis: An evolution of acrodermatitis continua of Hallopeau to generalized pustular psoriasis
Correspondence Address:
Zi-Gang Xu
Department of Dermatology, Beijing Children's Hospital, Capital Medical University, National Center for Children's Health, No. 56 South Li Shi Road, Xi Cheng District, 10045, Beijing
China
| How to cite this article: Chen YL, Wang ZY, Ma L, Xu ZG. Three cases of IL36RN-associated pustulosis: An evolution of acrodermatitis continua of Hallopeau to generalized pustular psoriasis. Indian J Dermatol Venereol Leprol 2020;86:562-565 |
Sir,
Generalized pustular psoriasis is characterized by generalized erythema and pustules accompanied by severe systemic symptoms. Acrodermatitis continua of Hallopeau is a rare localized pustulosis involing the digits and nails. It remains controversial whether acrodermatitis continua of Hallopeau is an independent disease or a localized form of generalized pustular psoriasis. Co-occurrence of both in one person has been reported.[1] In addition, the same IL36RN mutation loci were identified in a boy with acrodermatitis continua of Hallopeau and in his sister with generalized pustular psoriasis.[2] Thus, we speculated that the two might belong to a disease spectrum that shares the same pathogenesis. Herein, we report three children who experienced both acrodermatitis continua of Hallopeau and generalized pustular psoriasis. The IL36RN gene mutation was identified in all patients.
Patient 1 was an 8-year-old girl. She presented with generalized erythema, pustules and high fever when she was 5 years old and was diagnosed with generalized pustular psoriasis. After 2 months of treatment with acitretin (0.5 mg/kg/day), the pustules disappeared. After 2 years, erythema and pustules emerged on her distal fingertips and on the tips of her toes, which was accompanied by damage to her nails. A diagnosis of acrodermatitis continua of Hallopeau was made and oral acitretin (0.5 mg/kg/day) was given again. However, she experienced a repeated relapse-remission process during the 14-month treatment.
Patient 2 was a 9-year-old girl. When she was 1 year old, generalized pustules emerged in large areas of erythema. A diagnosis of generalized pustular psoriasis was made. The lesions disappeared on treating with topical corticosteroids. She experienced at least one relapse every 2 years thereafter, and generalized pustules reappeared when she was 5 years old. Although the severity of the generalized pustules was reduced with traditional Chinese herbs treatment, the pustular lesions remained on her fingers and toes. A diagnosis of acrodermatitis continua of Hallopeau was made. Acitretin was prescribed for 5 months, resulting in a partial improvement of the acrodermatitis continua of Hallopeau. When she was 8 years old, lesions of generalized pustular psoriasis and acrodermatitis continua of Hallopeau appeared again [Figure - 1]a and [Figure - 1]b. Oral acitretin and subcutaneous injection of etanercept were administered. The generalized pustular flares were eliminated, but the pustules remained on her digits and toes.
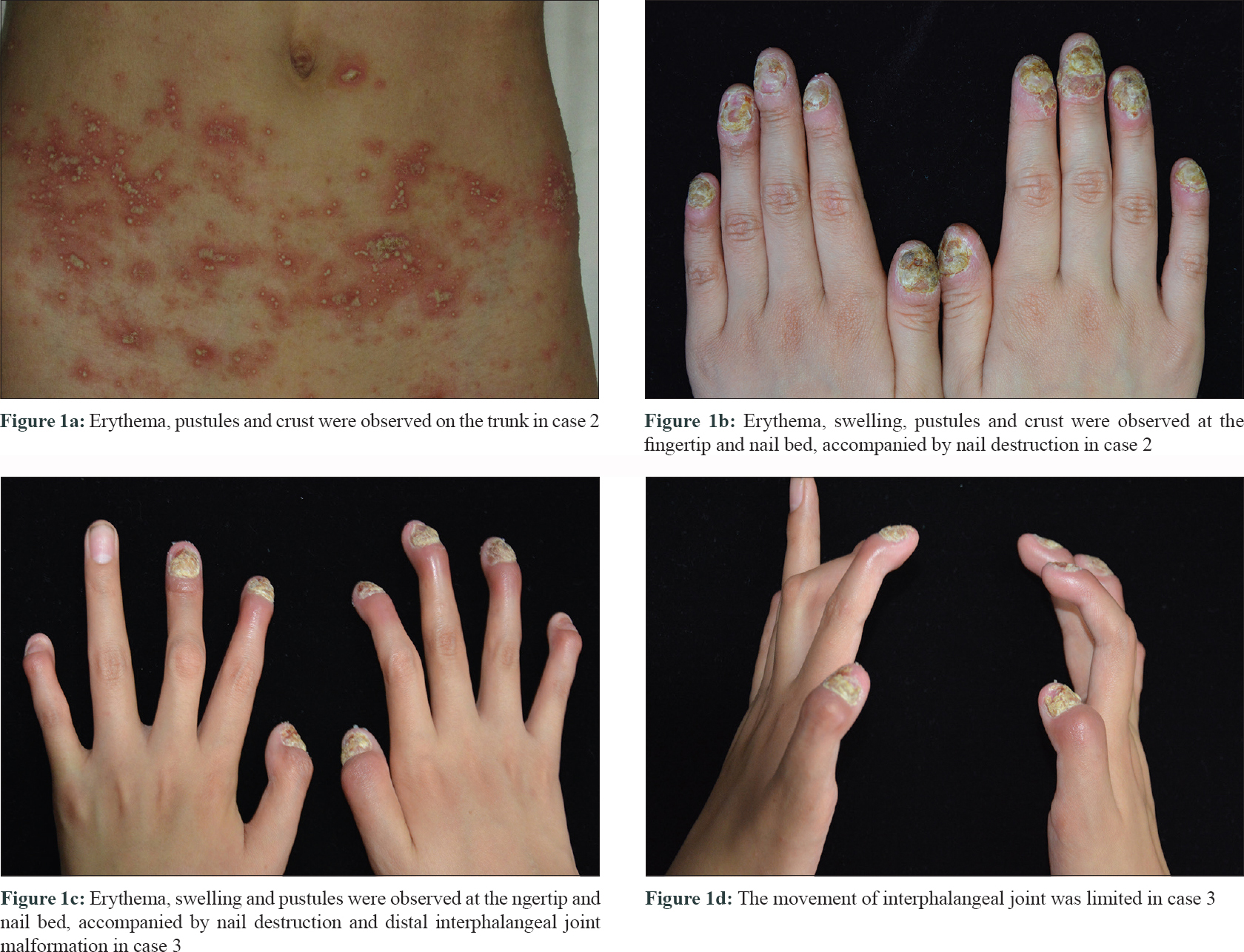 |
Patient 3 was a 13-year-old girl. She initially presented with erythema and pustules on her fingers when she was 4-year-old. The lesions extended to her feet when she was 8-year-old. A diagnosis of acrodermatitis continua of Hallopeau was made. When she was 12-year-old, the pustular lesions exacerbated and interphalangeal joint malformation appeared [Figure - 1]c and d]. Radiography demonstrated that the bone density of the phalanx was low and that the carpal joints and sacroiliac joints were rough and narrow. Several months later, generalized erythema and pustules with systemic symptoms appeared. A diagnosis of generalized pustular psoriasis was made. These lesions quickly improved with acitretin and cyclosporine. Nevertheless, the lesions on the extremities and nails were resistant to treatment.
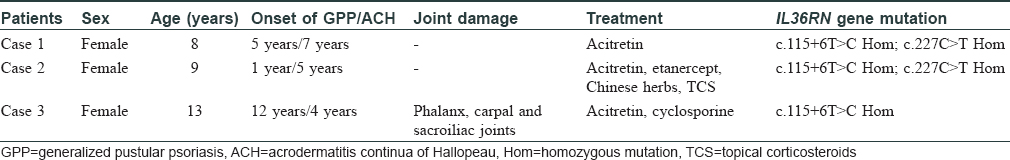
Peripheral blood samples from all three patients and their parents were subjected to IL36RN gene mutation screening [Figure - 2] and [Table - 1]. Patients 1 and 2 carried both c.115+6T>C and c.227C>T homozygous mutations; patient 3 carried only the c.115+6T>C homozygous mutation. The mutations were all inherited from their parents.
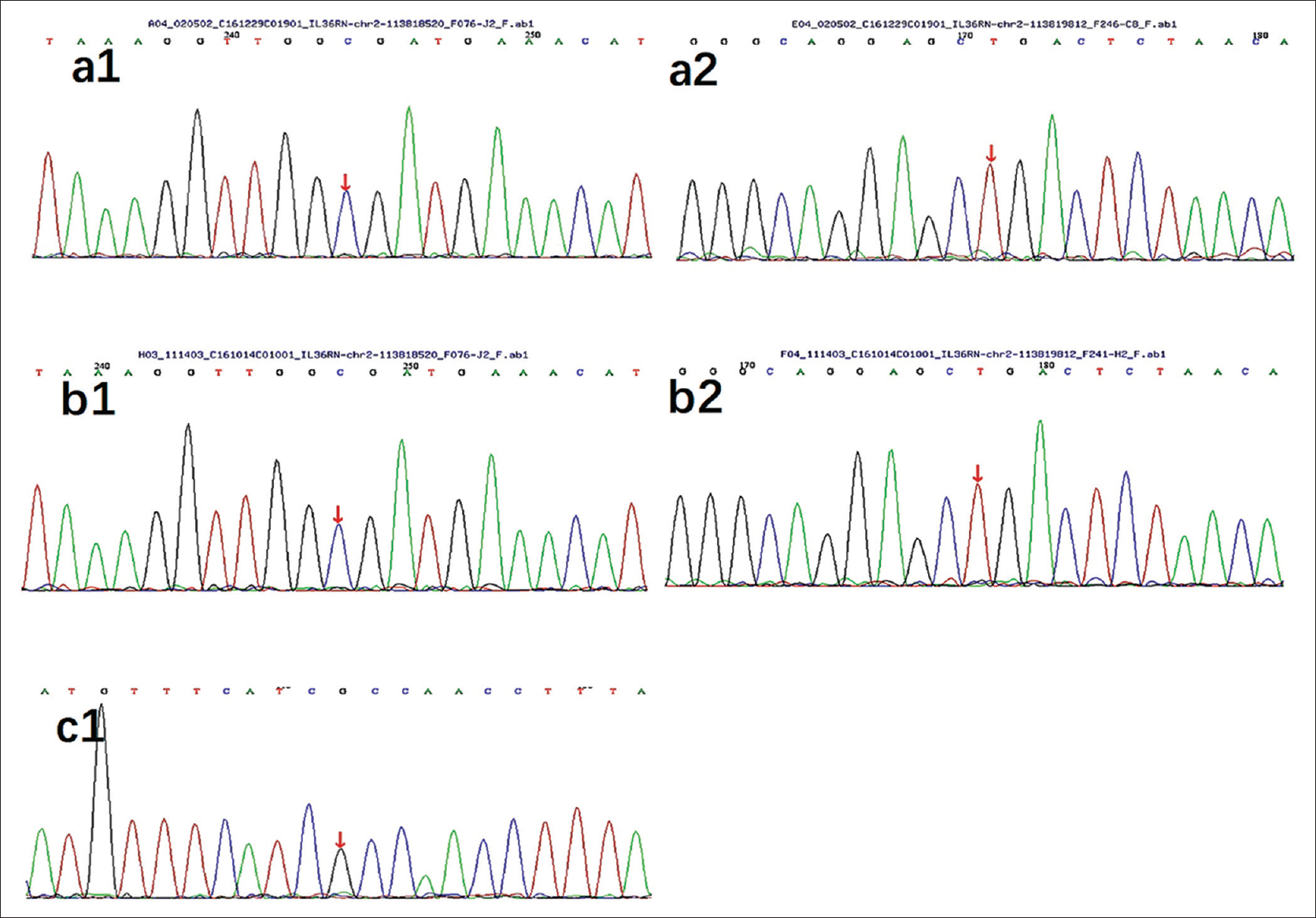 |
| Figure 2: IL36RN gene mutations in case 1 (a1, a2), case 2 (b1, b2) and case 3 (c1) |
In 2011, IL36RN gene mutation was first identified in nine Tunisian families with generalized pustular psoriasis and subsequently, in patients with acrodermatitis continua of Hallopeau.[3],[4] IL36RN genemutations lead to the functional deletion of the interleukin-36 receptor antagonist, enhancing the effect of interleukin-36 and resulting in activation of the NF-κB signaling pathway.[3] The deficiency of interleukin-36 receptor antagonist is classified as a new group of autoinflammatory diseases.[3]
The IL36RN mutations c.115+6T>C and c.227C>T mutations were identified in our three patients. The c.115+6T>C mutation, which is the most frequent change in Asian patients with pustular psoriasis, disrupts the splicing of exon 3 and leads to the synthesis of a truncated protein.[4] The c.227C>T mutation is a missense mutation in exon 4, leading to a reduction in the stability and function of the interleukin-36 receptor antagonist.[5]
None of the three patients had a family history of psoriasis, and all experienced both generalized pustular and acrodermatitis continua of Hallopeau variants, which occurred successively or simultaneously. All three patients had a good response to acitretin in the generalized pustular stage but a poor response in the acrodermatitis continua of Hallopeau stage. Hence, we treated acrodermatitis continua of Hallopeau with oral acitretin in combination with cyclosporine or etanercept. Although the acrodermatitis lesions were alleviated with combination therapy in a short period, they often relapsed soon thereafter.
Our findings provide evidence that acrodermatitis continua of Hallopeau and generalized pustular psoriasis belong to a disease spectrum with similar clinical features and the same genetic background. However, the conclusion is limited by the small number of patients and no further functional study of the mutant gene.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients/parents have given their consent for patient images and other clinical information to be reported in the journal. The patient/parents understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
The study was supported by Beijing Natural Science Foundation (7174300), Capital Clinical Characteristics (Z161100000516070), Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding (ZYLX201601) and Special Fund of The Pediatric Medical Coordinated Development Center of Beijing Municipal Administration (XTZD20180502).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kim KH, Kim HL, Suh HY, Jeon JW, Ahn JY, Park MY, et al. A case of acrodermatitis continua accompanied with osteolysis and atrophy of the distal phalanx that evolved into generalized pustular psoriasis. Ann Dermatol 2016;28:794-5.
[Google Scholar]
|
| 2. |
Abbas O, Itani S, Ghosn S, Kibbi AG, Fidawi G, Farooq M, et al. Acrodermatitis continua of Hallopeau is a clinical phenotype of DITRA: Evidence that it is a variant of pustular psoriasis. Dermatology 2013;226:28-31.
[Google Scholar]
|
| 3. |
Marrakchi S, Guigue P, Renshaw BR, Puel A, Pei XY, Fraitag S, et al. Interleukin-36-receptor antagonist deficiency and generalized pustular psoriasis. N Engl J Med 2011;365:620-8.
[Google Scholar]
|
| 4. |
Setta-Kaffetzi N, Navarini AA, Patel VM, Pullabhatla V, Pink AE, Choon SE, et al. Rare pathogenic variants in IL36RN underlie a spectrum of psoriasis-associated pustular phenotypes. J Invest Dermatol 2013;133:1366-9.
[Google Scholar]
|
| 5. |
Körber A, Mössner R, Renner R, Sticht H, Wilsmann-Theis D, Schulz P, et al. Mutations in IL36RN in patients with generalized pustular psoriasis. J Invest Dermatol 2013;133:2634-7.
[Google Scholar]
|
Fulltext Views
3,700
PDF downloads
1,408





