Translate this page into:
Thrombophlebitis of the lateral chest wall (Mondor's disease)
2 Department of Clinical Imaging Ultrasound, Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania
3 Department of Histology, Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania
Correspondence Address:
Maria Crisan
Trascaului Street No. 4/27, Cluj-Napoca
Romania
| How to cite this article: Crisan D, Badea R, Crisan M. Thrombophlebitis of the lateral chest wall (Mondor's disease). Indian J Dermatol Venereol Leprol 2014;80:96 |
Abstract
Mondor's disease is a rare condition, which involves the thrombophlebitis of the superficial veins of the breast and anterior chest wall. A 37-year-old woman presented with sudden onset of local pain and edema on her right chest wall, accompanied by a longitudinal retraction of the skin during arm abduction in the area. Clinical, histological and ultrasonographic findings confirmed Mondor's disease and the treatment was symptomatic, using pain relievers and warm compresses. The symptomatology remitted within 2 weeks of therapy. Mondor's disease is a rare condition where ultrasound complements the clinical evaluation and allows the characterization of certain abnormalities, which correlated with functional biochemical data and other procedures may substitute the need of biopsy.Introduction
Mondor′s disease is a benign, self-limiting disorder affecting more commonly women and involving usually the lateral thoracic vein. It is characterized by a sclerosing thrombophlebitis of the subcutaneous veins of the chest wall. The clinical appearance is of a subcutaneous, firm, painless cord accompanied by the retraction of the overlying skin.
Case Report
We report the case of a 37-year-old woman presenting 2 unilateral, firm, subcutaneous cords, situated on the lateral thoracic wall, not attached to the overlying epidermis. Patient related the presence of mild, local pain and edema on her lateral chest wall for the past week; she was clinically assessed and in addition, histological and ultrasound investigations were performed.
From the clinical point of view, the overlying skin had a normal aspect, but paresthesia of the lateral chest wall often occurred during the night. A longitudinal retraction of the skin overlying the superficial thrombophlebitis of the thoracoepigastric vein was also visible during complete arm extension and abduction [Figure - 1].
 |
| Figure 1: Clinical aspect: Two longitudinal subcutaneous cords on the lateral chest wall, visible after arm abduction |
Conventional ultrasound (GE Logiq 7 ultrasound device) revealed hypoechoic tracts, without any vascular signal [Figure - 2].
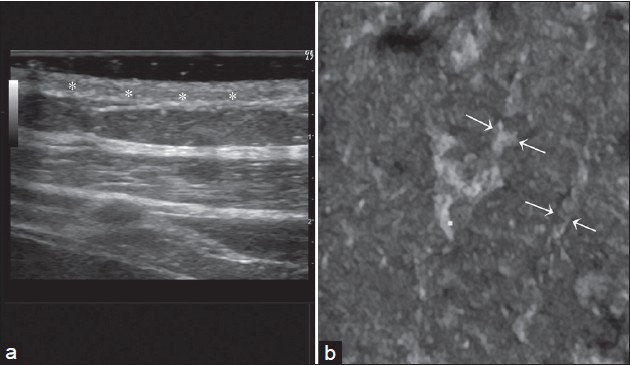 |
| Figure 2 (a and b): Two dimensional and three dimensional (3D) ultrasonographic assessment of the integument at vascular level. (a) Sectional assessment: Vascular structure appears echogenic; absence of lumen. Hypoechogenic center (*) corresponds to the obliterated vascular lumen. A signifi cant increase of the vascular wall thickness can be noticed. (b) 3D assessment – coronal plan view: Two vascular structures with obliterated lumen can be noticed; thick, echogenic walls, irregular, sinuous route (arrows). Subcutaneous tissue appears homogenous, with characteristic structure |
The histological examination revealed epidermis with normal features, a dermis with diffuse fibrosis and minimal lymphocytic infiltrate; subtle collagen fibers, disposed in an ordered manner, undulated by the retraction of the section at the level of the papillary dermis; dense fibrosis with thickened collagen fibers, irregularly disposed in the reticular dermis.
The diagnosis of Mondor′s disease was confirmed by cutaneous ultrasound that revealed dense, vascular structures, with fibrosed lumen and by histology, using special collagen stains. [1]
Patient was treated with warm local compresses and pain relievers (ibuprofen) for 2 weeks, resulting in complete resolution within 14 days.
Dicussion
Mondor′s disease is a rare condition, thrombophlebitis of the superficial veins of the breast and anterior chest wall. First described in detail by Henri Mondor in 1939, it is more frequently seen in women, although it can also occur in men (3:1 ratio). [2],[3]
The disease can appear at any age, but it usually affects people within the ages of 30-60 years, and has a benign, self-limiting course. The etiology remains an object of speculation and in many cases it is idiopathic, but it has been associated with local trauma such as: surgical biopsy, breast surgery, mammary inflammations and infections, breast cancer, local muscle strains, vigorous upper extremity exercise, tight clothes, abuse of intravenous drugs or even an association of these factors. Rarely, it may also be associated with lymphoma, lupus erythematosus and rheumatic arthritis. [4] Pathophysiology involves pressure on the vein with stagnation of blood, as well as direct trauma to the vein itself. It may only involve one or more of the following three venous channels: the thoracoepigastric vein, the lateral thoracic vein and the superior epigastric vein. [5]
The sudden appearance of a subcutaneous cord, which is initially red and tender and subsequently becomes a painless, tough, fibrous band that is accompanied by tension and skin retraction, is characteristic. The cord is accentuated by traction, elevation of the breast or abduction of the ipsilateral arm and usually involves no systemic symptoms. Mondor′s disease affects veins that protrude from the mammary nipple-areolar complex and axilla (lateral thoracic vein), above and around the epigastrium (superior epigastric vein) and in the costal margin and superior abdominal wall (thoracoepigastric vein). The course of the disease is self-limiting, lasting weeks or rarely months, before resolving spontaneously without any risk of embolization. [6] The management of the disease is therefore only symptomatic, involving hot wet dressings and pain relievers. [7]
The differential diagnosis of Mondor′s disease includes: lymphangiectasia, lymphangioma, cellulitis, erythema nodosum and metastatic carcinoma of the skin.
Ultrasonography allows the clear visualization of vascular structures, the thickened vascular wall as well as the obliterated lumen of vessels, allowing a non-invasive diagnosis of the disease. Biopsy, though rarely indicated, should be taken into consideration since the process may involve not only the small superficial veins, but also small arteries and lymphatics. The typical histopathological appearance is of a partial or total thrombus obliterated sclerosing endophlebitis.
| 1. |
Laroche JP, Galanaud J, Labau D, Van Kien AK, Brisot D, Boge G, et al. Mondor's disease: What's new since 1939? Thromb Res 2012;130 Suppl 1:S56-8.
[Google Scholar]
|
| 2. |
Leal B, Vieira S, Carvalho B, Correia A, Almeida B. Mondor's disease in a patient previously treated for breast carcinoma in situ: A case report. N Z Med J 2012;125:100-2.
in situ: A case report. N Z Med J 2012;125:100-2.'>[Google Scholar]
|
| 3. |
Azijli K, Merkus J, Warmerdam P. A woman with a palpable abnormality in the breast. Ned Tijdschr Geneeskd 2013;157:A5021.
[Google Scholar]
|
| 4. |
Veronesi P, Zurrida S. Mondor's disease: Is there any correlation with breast cancer? Arch Intern Med 2003;163:1657-63.
[Google Scholar]
|
| 5. |
Cesarone MR, Belcaro G, Agus G, Georgiev M, Errichi BM, Marinucci R, et al. Management of superficial vein thrombosis and thrombophlebitis: Status and expert opinion document. Angiology 2007;58 Suppl 1:7S-14.
[Google Scholar]
|
| 6. |
Khan UD. Mondor disease: A case report and review of the literature. Aesthet Surg J 2009;29:209-12.
[Google Scholar]
|
| 7. |
Lee JT, Kalani MA. Treating superficial venous thrombophlebitis. J Natl Compr Canc Netw 2008;6:760-5.
[Google Scholar]
|
Fulltext Views
8,624
PDF downloads
3,218





