Translate this page into:
Traditional versus e-learning during COVID-19 pandemic: An online survey on dermatology postgraduate teaching
Corresponding author: Dr. Neena Khanna, Department of Dermatology, Amrita Hospital, Faridabad, Haryana, India. neena_aiims@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Swarnkar B, Sharma A, Gupta V, Ramam M, Khanna N. Traditional versus e-learning during COVID-19 pandemic: An online survey on dermatology postgraduate teaching. Indian J Dermatol Venereol Leprol. 2024;90:382-4. doi: 10.25259/IJDVL_1172_2022
Dear Editor,
Like many other teaching institutes worldwide, we were suddenly forced to shift to an online training programme during the early part of the novel coronavirus-19 (COVID-19) disease pandemic. Our dermatology postgraduate teaching programme comprises a weekly seminar, journal club, clinical case discussion, spotters, dermatopathology discussion and lectures, which were conducted virtually via the Google Meet platform during the COVID-19 pandemic. We undertook a survey after more than a year of online teaching in our department at the All India Institute of Medical Sciences, New Delhi, to gain better insight into both modes of learning; traditional and the new e-learning. After approval from the institute ethics committee, a Google form (https://docs.google.com/forms/d/1K-SEr5KA1F0OOhB4OgPsJe3t79ge7s4FSyEwUL1Nmag/edit#responses) was emailed to our residents (n = 33) and faculty members (n = 10) and their responses were recorded anonymously. The Google form comprised 18 questions from a previously validated questionnaire,1 and another 18 questions, specific to our teaching programme, were developed by us.
Thirty-five of the 43 (81.3%) eligible participants: 21 (60%) postgraduates (7 first-year, 6 second-year and 8 final-year), 8 (22.9%) senior-residents and 6 (17.1%) faculty filled out the questionnaire. As compared to online teaching, respondents felt more attentive during traditional physical classroom teaching, believed it to be more efficient in encouraging them to learn by themselves and were better satisfied with it in meeting their educational needs. On the other hand, respondents were more comfortable raising queries in online classes. Time utilisation was considered better in online classes by more respondents (n = 17, 48.6% vs n = 11, 31.4%), while the audio-visual experience was considered better in physical classes (n = 22, 62.9% vs n = 8, 22.9%). Overall, traditional teaching was preferred for all teaching activities, except journal clubs and seminars, where both methods were preferred similarly [Figure 1]. Table 1 summarises the responses to the validated questionnaire.
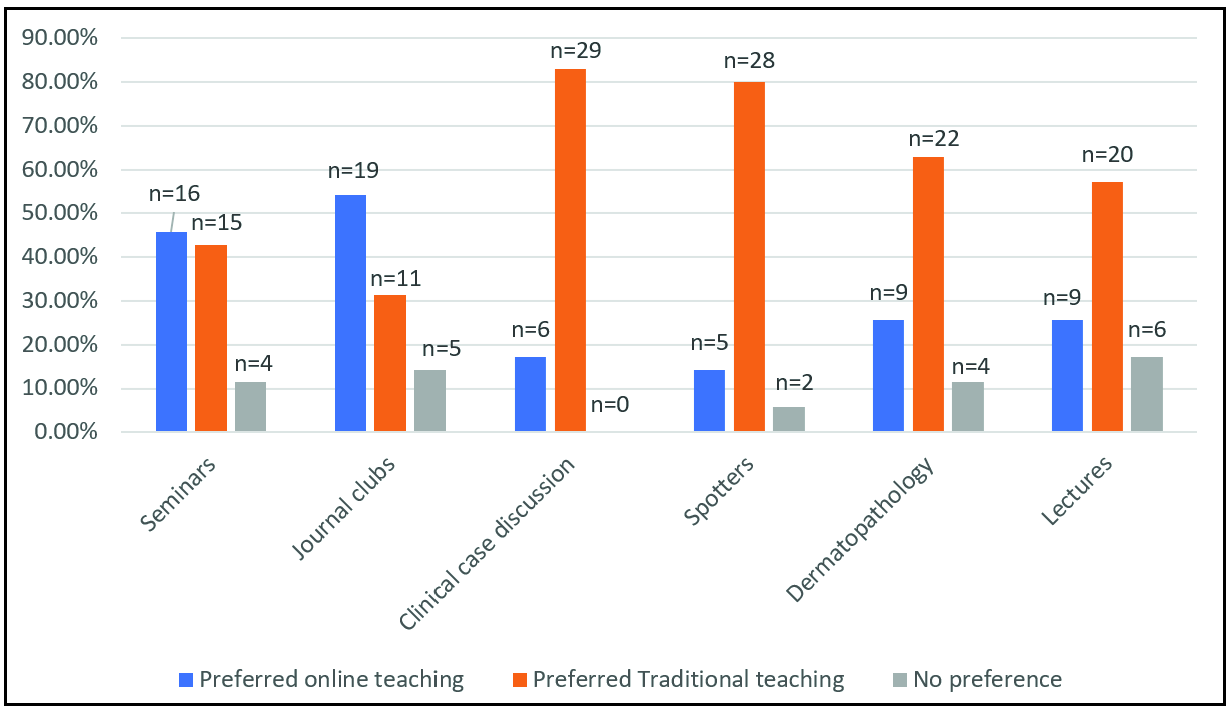
- Preferred teaching method for various academic activities in the dermatology curriculum (n = number of respondents out of 35).
| Question | Respondents with a response category >=4 on Likert scale* | p-value | |
|---|---|---|---|
| Online teaching (%) | Traditional teaching (%) | ||
| How convenient was it for you to attend academic sessions using both modes of teaching? | 25 (71.4%) | 18 (51.4%) | 0.08 |
| How attentive were you during the sessions? | 5 (14.3%) | 14 (40%) | 0.02 |
| How easy did you find comprehending the graphs and schematic diagrams? | 21 (60%) | 17 (48.6%) | 0.28 |
| How comfortable were you to raise the queries? | 23 (65.7%) | 13 (37.1%) | 0.03 |
| How satisfied were you with the way speakers addressed most of the queries? | 23 (65.7%) | 21 (60%) | 0.47 |
| How effective were the sessions in encouraging you to take an initiative to learn by yourself? | 13 (37.1%) | 21 (60%) | 0.02 |
| How satisfied were you with the sessions in meeting your educational needs? | 16 (45.7%) | 25 (71.4%) | 0.02 |
| How effective were the academic interactions to facilitate your overall learning in: | |||
| Seminars | 14 (40%) | 22 (62.9%) | 0.04 |
| Journal club | 12 (48%) | 17 (48.6%) | 0.19 |
| Clinical case discussion | 5 (14.3%) | 26 (74.3%) | <0.001 |
| Spotters | 10 (28.6%) | 30 (85.7%) | <0.001 |
| Dermatopathology | 16 (45.7%) | 26 (74.3%) | 0.01 |
| Lectures | 11 (31.4%) | 19 (54.3%) | 0.02 |
| How important are the following features of online teaching for you? | |||
| Flexibility to attend the session from wherever you are | 24 (68.6%) | NA | |
| Access to video recording of the sessions facilitating learning at your own speed for a given presentation | 22 (62.8%) | NA | |
| Ability to view recorded sessions more than once for revision | 22 (62.8%) | NA | |
| Ability to look up information critical to understanding of the concepts during the conduct of session | 20 (57.1%) | NA | |
| Accessibility to distant expertise from other departments/institutions | 20 (57.1%) | NA | |
| Ability to give instant feedback on content and presentation | NA | 18 (51.4%) | |
| Ability to have eye-to-eye contact and view gestures of the speaker | NA | 24 (68.6%) | |
| Ability to interact in a group | NA | 23 (65.7%) | |
| Ability to view the slides with respect to one's seating location | NA | 18 (51.4%) | |
NA, not applicable
Among the responses to the questions specific to our programme, more respondents reported less anxiety while speaking during online classes (n = 21, 60% vs. n = 5, 14%), but picked traditional method for developing public speaking skills and confidence (n = 27, 77% vs n = 1, 3%). More students were likely to evade a difficult question or cheat to find the answer during an online class (n = 21, 72% vs n = 1, 3%). The majority of them found it difficult to describe clinical findings in clinical case presentations in online sessions (n = 12, 34.3% vs n = 2, 5.7%) while it was more difficult to respond to a direct question in traditional teaching sessions (n = 11, 31.4% vs n = 4, 11.4%). More respondents reported being distracted during online sessions (n = 12, 34.3% vs n = 1, 2.9%). Physical discomfort (eye strain, neck pain, etc.) during the classes was reported by only a small proportion (<=20%) for both modes. Traditional teaching was viewed as a better method of learning than online teaching to make a clinical diagnosis, be it on images (n = 14, 40% vs n = 6, 17.1%) or by examining a patient (n = 28, 80% vs n = 2, 5.7%). While attending an online class, the majority had faced a connectivity problem at some time (n = 31, 88.6%), had logged in without really attending at least once (n = 29, 83%), or faced an embarrassing situation due to the mic or video being switched on by mistake at least once (n = 25, 71.4%). When asked about their overall experience with the modes of teaching, about (n = 28) 80% of the respondents rated their experience as ‘good’ with traditional teaching as compared to (n = 19) 54% with online teaching. More faculty members and senior residents preferred online classes for the flexibility in choosing cases for discussion (n = 7/14, 50% vs n = 2/14, 14.3%), but the interaction with students was felt to be better in traditional classes (n = 10/14, 71.4% vs n = 2/14, 14.3%). Overall, a similar proportion (n = 6/14, 42.9% and n = 5/14, 35.7%) of faculty members and senior residents preferred online or physical mode, while (n = 3/14) 21.4% had no preference (Supplementary data).
Recently, Nguyen et al published the feedback of dermatology faculty and residents (n = 65) regarding their experiences of the online dermatology curriculum in the United States. The features of online teaching, such as flexibility in attendance from any place and the opportunity to learn from distant speakers, were considered important by the majority, as seen in our survey as well. The major challenges faced with online curriculum were difficulty staying engaged, less spontaneous feedback and a lack of human features. Overall, a similar proportion of respondents (83% versus 76%) were satisfied with both offline and online teaching in their study.2 Another study including physiology postgraduates also found no statistically significant difference between the two modes of teaching in meeting their educational needs,1 while a study including surgery postgraduates reported that the majority favoured online teaching.3 A meta-analysis found no evidence to suggest the superiority of offline mode over online teaching for medical undergraduates.4
Our survey indicates that traditional teaching methods are preferred over online teaching, particularly for sessions like case discussions, spotters and dermatopathology slide discussions. This is an important finding, considering that dermatology is often considered a visual science where ‘looking’ is enough to make an accurate assessment. We did not find a clear preference for activities like journal club and seminars. Online classes were associated with less anxiety about public speaking and lent themselves suitably to such activities. The other important advantages include attending lectures from a remote site, access to experts from distant places and recording the lectures for watching later at a more convenient time as well as for revisions.
As the COVID-19 norms were relaxed, we shifted to a hybrid mode of teaching, with seminars and journal clubs continuing online while the rest shifted back to the traditional manner. It would appear that the right balance of both online and physical classroom teaching may be the way forward, not only in dermatology training programmes but also in other postgraduate and undergraduate programmes.
The results of our study are limited by a small sample size from a single institute. The improved technology and user comfort with online teaching post-COVID-19 pandemic may have a potential confounding effect on the survey responses.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Student perceptions on synchronous virtual versus face-to-face teaching for leader-centered and participant-centered postgraduate activities during COVID-19. Adv Physiol Educ. 2021;45:554-62.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Online dermatology curriculum experiences among US dermatology residents and faculty. Clin Dermatol 2022 S0738-081X(22)00106-7
- [Google Scholar]
- Utility of real-time online teaching during COVID era among surgery postgraduates. Indian J Surg 2020:1-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. 2019;24:1666538.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






